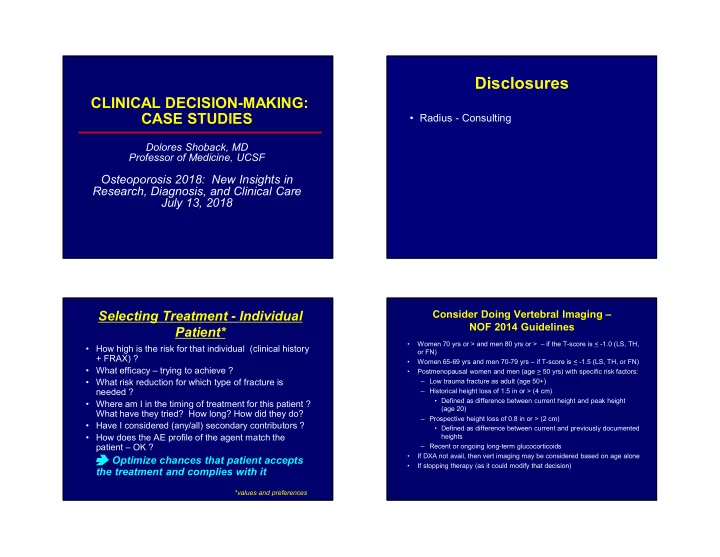
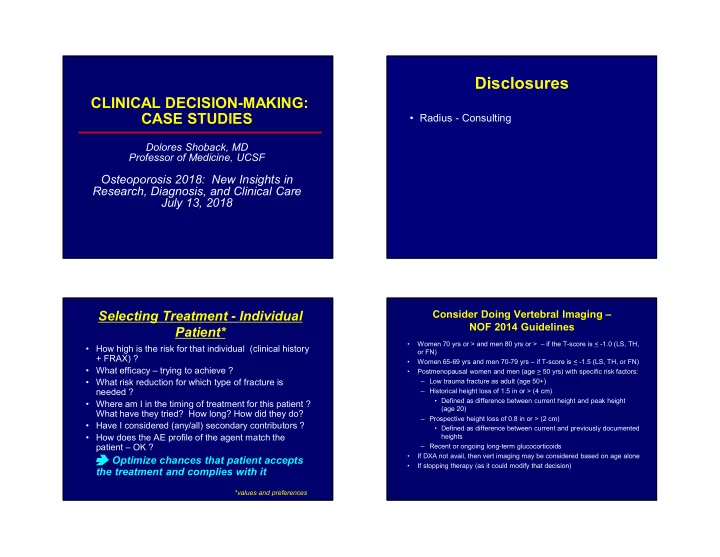
Disclosures CLINICAL DECISION-MAKING: CASE STUDIES • Radius - Consulting Dolores Shoback, MD Professor of Medicine, UCSF Osteoporosis 2018: New Insights in Research, Diagnosis, and Clinical Care July 13, 2018 Selecting Treatment - Individual Consider Doing Vertebral Imaging – NOF 2014 Guidelines Patient* • Women 70 yrs or > and men 80 yrs or > – if the T-score is < -1.0 (LS, TH, • How high is the risk for that individual (clinical history or FN) + FRAX) ? • Women 65-69 yrs and men 70-79 yrs – if T-score is < -1.5 (LS, TH, or FN) • What efficacy – trying to achieve ? • Postmenopausal women and men (age > 50 yrs) with specific risk factors: • What risk reduction for which type of fracture is – Low trauma fracture as adult (age 50+) needed ? – Historical height loss of 1.5 in or > (4 cm) • Defined as difference between current height and peak height • Where am I in the timing of treatment for this patient ? (age 20) What have they tried? How long? How did they do? – Prospective height loss of 0.8 in or > (2 cm) • Have I considered (any/all) secondary contributors ? • Defined as difference between current and previously documented • How does the AE profile of the agent match the heights patient – OK ? – Recent or ongoing long-term glucocorticoids • If DXA not avail, then vert imaging may be considered based on age alone Optimize chances that patient accepts • If stopping therapy (as it could modify that decision) the treatment and complies with it *values and preferences 1
Considerations: Treatment – Considerations – New Starts Experienced Patient Anti-resorptive • Try to establish the kind and duration of prior - Bisphosphonate therapy (very hard) - Denosumab Anabolic – - Raloxifene • Try to establish response – collect all DXA teriparatide - (Duavee- reports, analyze along with treatment history abaloparatide CE/Basodoxifene) (also hard) - ET/HT (younger) • Assess compliance – you may get some surprising results (easier than you think) eGFR • Check fracture history Costs ($$$) Active dental issues • Consider 2 o workup (surprising what might Contraindications Infectious risk (skin, GU) Hypocalcemia risk Daily injection hurdle have been missed celiac disease, Breast ca, CVD, clot risks Patient values and hypercalciuria, Ca malabsorption etc) Concomitant meds preferences Case 1 Case 1 – cont’d 56 yo woman referred by Gyn for second • Exam: 5 feet, 98 lbs; nl VS, + systolic murmur opinion – skeletal health in 2018 • LAB: CBC – wnl, CMP (Ca, creat, LFTs) – wnl; 25 OH vitamin D 53 ng/ml, TSH 1.52 • Menarche age 11, regular cycles, 1 FT pregnancy, menopause age 52; no h/o OCPs, depo-Provera L-spine L fem neck L total hip • ~Age 33 - thought to have rib fractures (after hug) 2016 0.769 0.778 0.713 • H/O - ‘joint pains’ and +ANA, treated for 1 year with prednisone (20 mg/d – highest; tapered off in 2017) -3.4 -1.9 -2.3 (age 54) – Prescribed HT (refused), alendronate (never took) • Meds: Ca suppl, vit D3 2000 IU/D 2018 ++ 0.561 0.555 0.604 • ROS: heavy bleeding (fibroids, 5 by U/S), +several -4.4 -2.7 -2.8 (age 56) breast biopsies (all neg), MV prolapse ( ++ different lab) • FH: father with hip fracture (Parkinson’s disease) • Habits: no smoking or alcohol; minimal exercise, low FRAX* 19% 10-yr risk of major osteoporotic frx, 2.3% dietary Ca 10-yr risk of hip frx (20%, 3% - US thresholds) *Parental hip frx, steroids 2
North American Menopause Society: Approach to Management Position Statement ( Menopause , 24, 728, 2017) Postmenopausal + glucocorticoid osteoporosis • HT (ET, EPT) – most effective for vasomotor • Complete workup: anti-tissue transglutaminase Ab, 24 symptoms and GU syndrome of menopause, prevents hr urine Ca, PTH, T/L spine films (r/o occult frx) bone loss and fracture Management • Treatment – individualized (type, dose, routes, • Optimize Ca intake (vit D3-ok), start wt bearing duration) to maximize benefits and reduce risk, with exercise (5/7 days per week) periodic re-evaluation of risks and benefits • Despite FRAX not meeting US thresholds (spine xrays • Women < 60 yrs old or within 10 yrs of menopause neg) offer pharmacologic therapy ? – If no contraindications, benefit/risk ratio – good, esp if – Hormone therapy +vasomotor symptoms and at high risk for bone loss or – Raloxifene fractures (this pt no VMS) – Bazedoxifene+CE (Duavee) • Women > 60 yrs old or >10 yrs postmenopause – Bisphosphonate – Risks higher for CV disease, stroke, VTE, dementia (not – Denosumab endorsing in these women) – Teriparatide Continue therapy if documented indication (“silent” – Abaloparatide on duration “individualize”) * Age and Adverse Event Profile: HT Management – Agreed to more calcium (1,200 mg/d), exercise My choice Her choice Hormone therapy * Raloxifene XXX Bazedoxifene + CE* Bisphosphonate #2 Denosumab Teriparatide #1 Abaloparatide #1 * fibroids, breast disease (Gyn rec against any form of HT) Individualized management, shared decision-making NAMS Position Statement, Menopause, 24, 728 , 2017 3
Case 2 Case 2 – cont’d 56 yo woman referred by Women’s Health • Exam: 115 lbs, BMI 21.4; nl VS and exam Clinic for management of low BMD in 2015 • LAB: CBC – wnl, CMP (Ca, creat, LFTs) – wnl; 25 OH vitamin D 21 ng/ml; TSH 1.61; 24 h urine Ca 70 mg • Menarche age 12, regular cycles, menopause age 51; (100-250); PTH 36 (15-88); SPEP nl no OCPs, depo-Provera, glucocorticoids L-spine L fem neck L total hip • Fell on ice (age 48) – living in NJ tibial frx 2/2015 0.706 0.637 0.746 • PMH: + duodenal ulcer (2 unit-UGI bleed in 2015); h/o -3.1 -1.9 -1.6 gastric ulcer; + hyperlipidemia; +HTN (age 56) • Meds: HCTZ 12.5 mg, Simva 20 mg, Omeprazole 20 mg bid, occas MVI Spine xrays: disc space narrowing (L4-5, L5-S1, no frx) • ROS: +sciatica (back pain; shooting pains in both CT: mod DDD, disc bulges @ multiple levels, no frx legs) • FH: +osteoporosis in mother (wheelchair late in life) FRAX (2015)*: 13% 10-yr risk of major osteoporotic frx, • Habits: + smoking (40 pack-years), occ social drinker; 2.5% 10-yr risk of hip frx (20%, 3% - US thresholds) active at work (small business owner0, but limited exercise; low dietary Ca * Counting fall on ice (age 48) Approach to Management Approach to Management Postmenopausal osteoporosis – evident at age 56 Postmenopausal osteoporosis – evident at age 56 (+FH, smoking, petite body habitus, low Ca intake, +/-vit D) (+FH, smoking, petite body habitus, low Ca intake, +/-vit D) • Complete workup: anti-tissue transglutaminase Ab • Complete workup: anti-tissue transglutaminase Ab Management Management • Optimize Ca and vit D3 intake (1200 mg, 2000 IU/d), • Optimize Ca and vit D3 intake (1200 mg, 2000 IU/d), start wt bearing exercise (5/7 days per week), reduce start wt bearing exercise (5/7 days per week), reduce lifting at work, STOP smoking lifting at work, STOP smoking • FRAX - does not meet US thresholds offer • FRAX - does not meet US thresholds offer pharmacologic therapy ?? (spine T score -3.1) pharmacologic therapy ?? (spine T score -3.1) – Hormone therapy * smoking concern – Raloxifene – Bazedoxifene+CE (Duavee) * smoking concern – Bisphosphonate *** oral – no d/t GI bleed, ulcers – Denosumab – Teriparatide ** refused daily injections, missed 2 f/u appt’s 4
Tissue Selective Estrogen Complex BMD Responses to TSEC vs PBO (12 mon) (CE + SERM Bazedoxifene) • Conjugated estrogen + bazedoxifene 20 mg • Like estrogen – “boxed warning” women over age 65 – increased risk of dementia, endometrial cancer, stroke, DVT • This combination – no increased risk for endometrial hyperplasia; insufficient data to evaluate risk for CV events (no progestin) • Contraindications: uterine bleeding, breast ca, arterial/venous TEE’s, liver disease, thromophilic disease • AE’s (RCTs): decently tolerated, less vaginal • 1172 pm women, mean age 54.9 years, FRAX score bleeding vs CE (H2H trials) 5% or less “protective” Gallagher JC et al, Menopause, 2016 Case 2 – cont’d Lumbar spine Total hip • Opted for IV zoledronic acid (compliance, avoid PO) • Received in 2/2016 and 2/2017 (5 mg) • Interval history (6/2018): inferior wall STEMI – requiring 4 stents in 4/2017; d/c smoking completely L-spine L fem neck L total hip 2/2015 0.706 0.637 0.746 7 years • 7 year study (2 extensions) -3.1 -1.9 -1.6 (age 56) • 7492 women, age 55-85 6/2018 0.767 0.652 0.761 yrs (average 66-67) -2.5 -1.8 -1.5 • Osteoporotic at baseline (age 59) (BMD, prevalent vert frx) % change +8.6% +2.4% +2.0% • Reduction in vert frx 42% and 37% (BZA 20 vs 40 Management now: Post-STEMI (no enthusiasm for mg/d) – no effects on estrogen-based therapy); at spine, + changes exceed least significant change (so real) nonvert frx (3 years rx) Palacios S et al, Menopause, 2015 5
Recommend
More recommend