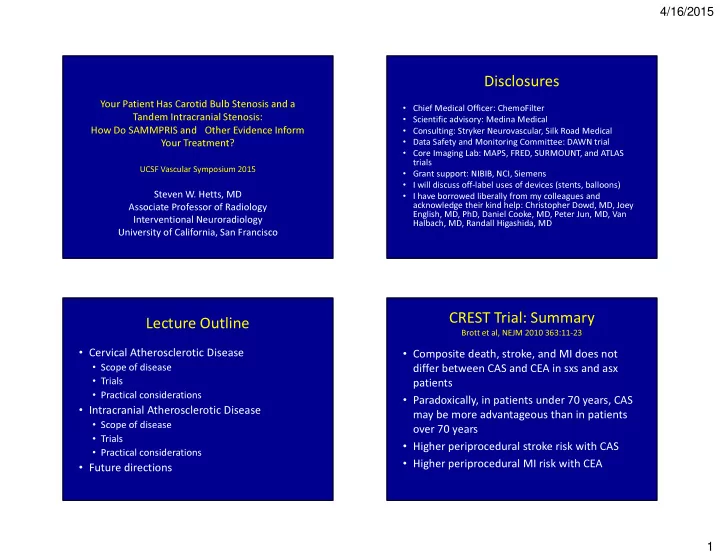
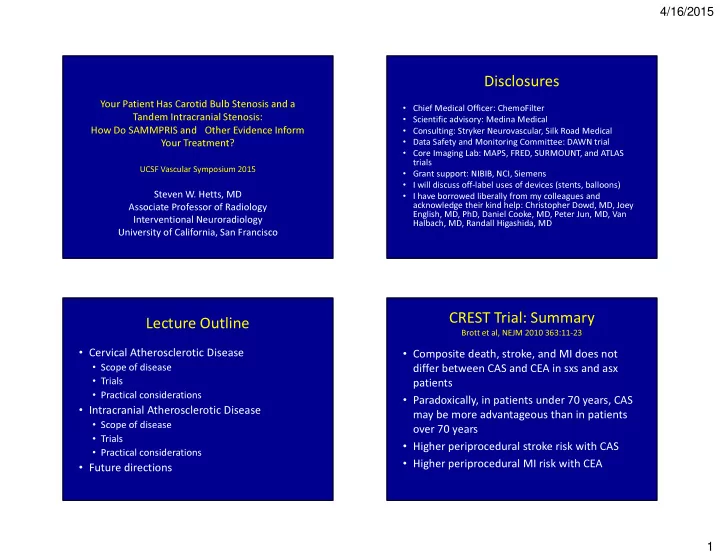
4/16/2015 Disclosures Your Patient Has Carotid Bulb Stenosis and a • Chief Medical Officer: ChemoFilter • Scientific advisory: Medina Medical Tandem Intracranial Stenosis: • Consulting: Stryker Neurovascular, Silk Road Medical How Do SAMMPRIS and Other Evidence Inform • Data Safety and Monitoring Committee: DAWN trial Your Treatment? • Core Imaging Lab: MAPS, FRED, SURMOUNT, and ATLAS trials UCSF Vascular Symposium 2015 • Grant support: NIBIB, NCI, Siemens • I will discuss off-label uses of devices (stents, balloons) • I have borrowed liberally from my colleagues and Steven W. Hetts, MD acknowledge their kind help: Christopher Dowd, MD, Joey Associate Professor of Radiology English, MD, PhD, Daniel Cooke, MD, Peter Jun, MD, Van Interventional Neuroradiology Halbach, MD, Randall Higashida, MD University of California, San Francisco CREST Trial: Summary Lecture Outline Brott et al, NEJM 2010 363:11-23 • Cervical Atherosclerotic Disease • Composite death, stroke, and MI does not • Scope of disease differ between CAS and CEA in sxs and asx • Trials patients • Practical considerations • Paradoxically, in patients under 70 years, CAS • Intracranial Atherosclerotic Disease may be more advantageous than in patients • Scope of disease over 70 years • Trials • Higher periprocedural stroke risk with CAS • Practical considerations • Higher periprocedural MI risk with CEA • Future directions 1
4/16/2015 Carotid Stenting Indications CAS: Patient Selection • Hemodynamically Significant > 50-70% • High Risk Surgical Patients • Failed Medical Therapy – Severe Coronary or Pulmonary Disease • Clinically Symptomatic – Recent MI, Stroke • Surgically Difficult Access – Stroke – Lesions arising off Aortic Arch – TIA – Lesions above the Mandible >C2 – Focal Neurological Signs – All Intracranial Lesions – Amaurosis Fugax • Traumatic or Spontaneous Dissections Pre Treatment Assessment Relative Carotid Stenting Indications • Complete Neurological • Multiple Vessel Disease Assessment – Occlusion of Contralateral Carotid or Vertebral • Brain MRI/CT Scan – Tandem Stenosis with Intracranial Lesion • Recurrent Stenosis Post Endarterectomy • Anti-Platelet Medications • History of Cervical Radiation • Cerebral Blood Flow • Long Segment Lesions >4 cm Studies • Traumatic Carotid Pseudoaneurysms • Complete Angiographic Assessment 2
4/16/2015 53 yo F with progressive stepwise L hemiparesis Case Example Tandem cervical ICA and MCA stenoses Treatment options • Medical management • Stent cervical ICA under conscious sedation • Stent cervical ICA under MAC • Stent cervical ICA under GA • Stent cervical ICA and PTA MCA under GA • Stent cervical ICA and stent MCA under GA • ECA-ICA bypass • Run the other way 3
4/16/2015 Cerebral diagnostic DSA pre ICA stent Cervical ICA stenting Cerebral DSA pre and post ICA stent Initially no change in HP post ICA stenting, then worsening HP 4
4/16/2015 Original DWI before ICA stenting New areas of temporal ischemia Now what would you do? CT Perfusion • Medical management rCBV MTT • ICU pressor challenge • PTA MCA • Stent MCA • ECA-ICA bypass • Run the other way • Get more imaging 5
4/16/2015 M2 MCA severe stenosis CT Perfusion rCBV MTT ICAD: Scope of Disease Medical Therapy for ICAD • 8-10% of strokes and TIAs in USA due to ICAD • Anticoagulation for ICAD described in 1955 • 70,000-90,000 strokes/TIAs per year • Retrospective studies suggested warfarin was • Recurrent stroke risk 15-25% per year superior to ASA for ICAD stroke prevention • WASID (2005): landmark prospective trial • Higher ICAD rate in Black, Asian, and Hispanic comparing ASA to warfarin for recurrent populations stroke/TIA prevention • WASID showed no benefit of warfarin over ASA and increased risk of bleeding 6
4/16/2015 ECA-ICA Bypass for ICAD PTA and Stenting for ICAD • Described in 1967 to prevent stroke in • WASID trial suggested that best medical therapy for ICAD still had high risk for recurrent stroke patients with symptomatic ICA or MCA • Reasonable to research PTA and stenting as well stenoses • Prospective ECIC bypass trial (NEJM 1985) as new medications for ICAD • Off label use of coronary PTA balloons since – 1377 pts randomized to bypass or medical tx 1980s – ECIC bypass no better for ICA lesions • Off label use of coronary stents since 1990s – ECIC bypass worse for severe MCA stenoses • SAMMPRIS Trial • COSS Trial (stopped in 2010 by NIH) – Randomized symptomatic ICAD patients to medical – ECIC bypass for carotid occlusion patients with therapy (ASA/clopidogrel) or stent designed for ICAD increased oxygen extraction fraction by PET plus ASA/clopidogrel M2 MCA severe stenosis MCA PTA 7
4/16/2015 Stenting catheter navigation MCA stenting DSA post MCA revascularization DSA before ICA and MCA stenting 8
4/16/2015 Intracranial Atherosclerosis: Ischemic Stroke Mechanisms DSA post MCA revascularization 1. Flow-limiting -> Hypoperfusion -> Deep Watershed Ischemia 3. Perforator Injury -> Deep “ Lacunar ” Infarcts 2. Distal Emboli -> Wedged-Shaped Cortical Infarcts SAMMPRIS TRIAL SAMMPRIS TRIAL Predicted Event Rates: 30 day 1 year Predicted Event Rates: 30 day 1 year Medical Arm 11% 25% Medical Arm 11% (5.8%) 25% Stenting Arm 5-9% 8-15% Stenting Arm 5-9% (14.7%) 8-15% 9
4/16/2015 WINGSPAN STENT SYSTEM Important SAMMPRIS Information to Follow 1. Influence of Presenting Pattern of Ischemia and/or Location of Stenosis on the Risk of Procedural Ischemia 2. Extent/Location of Infarction and Timing of Revascularization Potential Complications 1. Flow-limiting -> Hypoperfusion -> Deep Watershed Ischemia 3. Perforator Injury -> Deep “ Lacunar ” Infarcts 2. Distal Emboli -> Wedged-Shaped Cortical Infarcts 4. Reperfusion Injury -> Edema and/or Hemorrhage 5. Procedural -> Wire Perforation, SAH/IPH Future Directions in Cervical and Intracranial Atherosclerosis • Medical – new antiplatelets – statins Thank You • Surgical – CEA for many, CAS for some • Endovascular: optimization of stenting – Distal emboli steven.hetts@ucsf.edu – Perforator occlusion – Patient selection based on stroke type 10
Recommend
More recommend