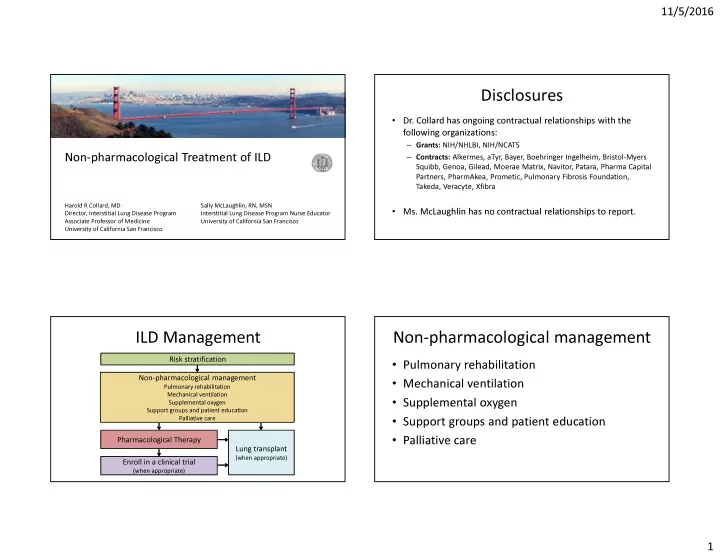
11/5/2016 Disclosures • Dr. Collard has ongoing contractual relationships with the following organizations: – Grants: NIH/NHLBI, NIH/NCATS – Contracts: Alkermes, aTyr, Bayer, Boehringer Ingelheim, Bristol-Myers Non-pharmacological Treatment of ILD Squibb, Genoa, Gilead, Moerae Matrix, Navitor, Patara, Pharma Capital Partners, PharmAkea, Prometic, Pulmonary Fibrosis Foundation, Takeda, Veracyte, Xfibra Harold R Collard, MD Sally McLaughlin, RN, MSN • Ms. McLaughlin has no contractual relationships to report. Director, Interstitial Lung Disease Program Interstitial Lung Disease Program Nurse Educator Associate Professor of Medicine University of California San Francisco University of California San Francisco ILD Management Non-pharmacological management Risk stratification • Pulmonary rehabilitation Non-pharmacological management • Mechanical ventilation Pulmonary rehabilitation Mechanical ventilation • Supplemental oxygen Supplemental oxygen Support groups and patient education • Support groups and patient education Palliative care • Palliative care Pharmacological Therapy Lung transplant (when appropriate) Enroll in a clinical trial (when appropriate) 1
11/5/2016 Pulmonary rehabilitation • “a comprehensive intervention based on a thorough patient assessment followed by Pulmonary rehabilitation patient-tailored therapies that include, but are not limited to, exercise training, education, and behavior change ….” Spruit AJRCCM 2013;188:e13 Do you refer ILD patients to PR? IPF: Pulmonary rehabilitation • “The majority of patients with IPF should be A. Yes, and almost all of my patients go. 46% treated with pulmonary rehabilitation...” B. Yes, but many of my patients cannot go 31% due to insurance issues 17% C. Yes, but many of my patients cannot go 6% – WEAK YES recommendation due to location/tansportation issues – LOW QUALITY evidence . . . . . . . . . . . . h f y y o D. No, I do not find PR helpful in ILD m m R l P l a f f o o d t s n y y o n n f i m a a t m m o a l n d t t o u u n d b b a I , , , s s , s e e o e Y Y N Y Raghu AJRCCM 2011;183:788 2
11/5/2016 Change in 6MW distance after PR Change in dyspnea after PR Holland Cochrane Syst Review 2014 Holland Cochrane Syst Review 2014 Change in QOL after PR Duration of PR benefit? Holland Cochrane Syst Review 2014 Ryerson Resp Med 2014;108:203 3
11/5/2016 Duration of PR benefit? Challenges to PR implementation • Insufficient reimbursement for PR programs • Lack of payer coverage for patients • Lack of knowledge/awareness • Limited training opportunities for staff Ryerson Resp Med 2014;108:203 Rochester AJRCCM 2015;192:1373 How often do you use MV in ILD? A. Frequently (75% or greater) 63% B. Often (25-75%) Mechanical ventilation 28% C. Rarely (less than 25%) 9% ) ) % % . . . 5 5 r 7 2 g - r 5 n o 2 a % ( h n t 5 e s 7 s t ( f e O l y ( l t y n l e e r u a q R e r F 4
11/5/2016 How often do you use MV in IPF? IPF: Mechanical ventilation • “The majority of patients with respiratory A. Frequently (75% or greater) 77% failure due to IPF should not receive B. Often (25-75%) mechanical ventilation...” C. Rarely (less than 25%) 21% 2% – WEAK NO recommendation – LOW QUALITY evidence ) ) . % % . . 5 5 r g 7 2 - r 5 n o 2 a h % ( n t 5 s 7 e t s ( e f y O l ( l t y n l e e r u a q R e r F Raghu AJRCCM 2011;183:788 MV in idiopathic pulmonary fibrosis MV in idiopathic pulmonary fibrosis • Study using Nationwide Inpatient Sample (US) • Study using Nationwide Inpatient Sample (US) • Patients from 2006-2012 with IPF by ICD9 • Patients from 2006-2012 with IPF by ICD9 1703 received 1703 received mechanical ventilation mechanical ventilation 17,700 patients 17,700 patients with IPF with IPF 778 received non- 778 received non- invasive ventilation invasive ventilation Rush Resp Med 2016;111:72 Rush Resp Med 2016;111:72 5
11/5/2016 MV in idiopathic pulmonary fibrosis MV in idiopathic pulmonary fibrosis 50 50 60 60 Limitations: Mortality (%) Mortality (%) Mortality (%) Mortality (%) 55 55 40 40 1. Heterogeneous population by diagnosis 50 50 - patients without IPF - patients intubated for non-respiratory reason 30 30 45 45 2. Heterogeneous population by disease severity 40 40 20 - no measure (except for oxygen use) available 20 - sicker patients may not have been offered 2006 2008 2010 2012 2006 2008 2010 2012 2006 2008 2010 2012 2006 2008 2010 2012 mechanical ventilation Intubation Non-invasive Intubation Non-invasive Rush Resp Med 2016;111:72 Rush Resp Med 2016;111:72 ATS: Supplemental oxygen • “We recommend that patients with IPF and Supplemental oxygen clinically significant resting hypoxemia should Support groups and patient education be treated with long-term oxygen therapy...” Palliative care – STRONG YES recommendation – VERY LOW QUALITY evidence Raghu AJRCCM 2011;183:788 6
11/5/2016 SECTION HEADING Supplementary oxygen is: Supplemental Oxygen Goal A. Easy for most of my patients to get 65% Keep saturation ≥ 90% at rest, with activity, during sleep, at altitude (planes) AND covered stay active 2011 – Center for Medicare and Medicaid Services (CMS) Competitive Bidding B. Easy for some patients, difficult for 27% Program = poor reimbursement to oxygen suppliers others 8% = restricted choice of, and access to, equipment C. Difficult for most patients to get = people in lower socioeconomic levels, rural areas, people who need . . . . . . . . p s . t i y n t a higher flows unable to get the equipment they need m e p i covered t f a t o s p o t m s e o m ATS efforts m r o o s f r o t r l f o u y f c s y i a s f f E a i D E 26 In general, my patients: Support groups help patients & family • A. Feel well-educated about their disease Learn about disease and treatment • 57% Feel supported by others who understand • and have adequate support available Develop self-sufficiency • 39% Learn to navigate healthcare system more effectively • Learn to be a more knowledgeable/engaged patient B. Are confused and scared about their • Make better decisions about their health care • disease and lack support Maintain a sense of normalcy • 4% Improve coping skills • Share stories with those who understand C. Are somewhere in between • Help others . . • . r . . a . . . Fell less anxious a c b d s n e d i • t n e a a r Change health behaviors c e d u h e d w e s • u e - l f m Fell less isolated and more hopeful l n e o o w c s l e e e r r e A A F 7
11/5/2016 Education Palliative Care and Hospice • Distressing symptoms of dyspnea, cough, fatigue www.pulmonaryfibrosis.org • Decreased activity levels and difficulty carrying out ADLs • Fear of suffocation www.scleroderma.org • Depression, fear, anxiety, social isolation, dependence www.lamfoundation.org • Caregiver well-being • Financial burdens www.stopsarcoidosis.org • Spiritual/existential distress • Bereavement Summary • Non-pharmacological care is am important component of comprehensive ILD care! • Availability of key treatments (e.g. pulmonary Non-pharmacological Treatment of ILD rehabilitation, supplemental oxygen) can be a big problem for patients! • In general, patients should be connected with Harold R Collard, MD Sally McLaughlin, RN, MSN support and advocacy groups! Director, Interstitial Lung Disease Program Interstitial Lung Disease Program Nurse Educator Associate Professor of Medicine University of California San Francisco University of California San Francisco 8
Recommend
More recommend