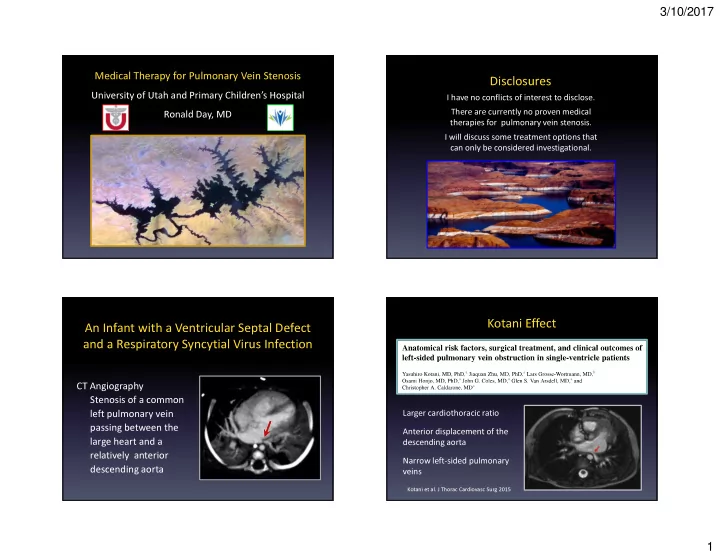
3/10/2017 Medical Therapy for Pulmonary Vein Stenosis Disclosures University of Utah and Primary Children’s Hospital I have no conflicts of interest to disclose. There are currently no proven medical Ronald Day, MD therapies for pulmonary vein stenosis. I will discuss some treatment options that can only be considered investigational. Kotani Effect An Infant with a Ventricular Septal Defect and a Respiratory Syncytial Virus Infection CT Angiography Stenosis of a common Larger cardiothoracic ratio left pulmonary vein passing between the Anterior displacement of the large heart and a descending aorta relatively anterior Narrow left-sided pulmonary descending aorta veins Kotani et al. J Thorac Cardiovasc Surg 2015 1
3/10/2017 Pathogenesis of Pulmonary Vein Stenosis Prevention of Pulmonary Vein Stenosis Observation and Challenge So could heart size be a potential factor Stenosis is more common in the left pulmonary veins Conditions associated with cardiomegaly Prematurity (patent ductus arteriosus) Congenital heart defects Heart transplantation Additional factors that stimulate intraluminal changes at the left atrial connection and in the upstream vessels Necrotizing enterocolitis (Heching HJ et al) Inflammation Respiratory infections Genetic tendancy for microvascular disease (MTHFR) Mechanical injury: interventions with good intentions Pathogenesis of Pulmonary Vein Stenosis Treatment of Pulmonary Vein Stenosis Vinblastine and Methotrexate Increased muscular thickness of pulmonary veins Extensive growth of cells in the intima with Rationale: Chemotherapy to suppress proliferation features consistent with myofibroblasts March 2000 to October 2006 29 patients were offered therapy 15 patients were treated without withdrawal 6 patients survived more than one year Vinblastine and Methotrexate could potentially alter the progression of pulmonary vein stenosis in some patients. However, there was enough toxicity that treatment was often interrupted or delayed. Rehman et al. Congenit Heart Dis 2011 Pogoriler et al. Pediatr Dev Pathol 2016 2
3/10/2017 Pathogenesis of Pulmonary Vein Stenosis Pathogenesis of Pulmonary Vein Stenosis Pulmonary Vein Banding Pulmonary Vein Banding Similar cellular changes in the wall of upstream Banded pulmonary veins demonstrated vessels as veins in human pulmonary vein stenosis an increase in the expression of TGF- β 1 Endothelial to Mesenchymal Cell Transformation: Myofibroblasts TGF β 1 TGF β 1/GAPDH CD31 α -SMA Merged Sham Sham Banded Banded Kato et al. J Thorac Cardiovasc Surg 2014 Kato et al. J Thorac Cardiovasc Surg 2014 Potential Therapy for Pulmonary Vein Stenosis Pathogenesis of Pulmonary Vein Stenosis Histology of Seven Patients Evaluated the effects of Losartan in neonatal pigs who underwent banding of their pulmonary veins Bilateral disease involving 2 vessels Losartan decreased intimal hyperplasia Immunoreactivity for several tyrosine kinase receptors Intensity of staining: Grades (0 negative to 4 marked) in the upstream vessels, at least short-term Previous Treatment Banded Losartan Unbanded Sham Angioplasty (5), surgery (4), chemotherapy (1), brachytherapy (1) Cells in the lesions of pulmonary vein stenosis stained mildly to markedly with tyrosine kinase receptors Platelet-derived growth factor receptors (PDGFR), α and β Vascular endothelial growth factor receptor (VEGFR), 2 Reidlinger et al. Cardiovasc Pathol 2006 Zhu et al. J Thorac Cardiovasc Surg 2014 3
3/10/2017 Treatment of Pulmonary Vein Stenosis Treatment of Pulmonary Vein Stenosis Imatinib (Gleevec) and Bevacizumab (Avastin) Imatinib (Gleevec) and Bevacizumab (Avastin) Single arm, prospective, open-label trial Best Assess Assess Assess Anatomic Disease Disease Disease FDA approved Palliation Status Status Status Industry sponsored Drug Therapy Aims Describe the feasibility of administering Gleevec, with or without Avastin, to mitigate the progression of multi- Interventional Catheterization, Surgery, Lung Transplant vessel disease for intraluminal pulmonary vein stenosis 0 weeks 48 weeks 72 weeks 24 weeks Safety: incidence of serious adverse events Patient Primary Final Enrollment Endpoint Endpoint Efficacy: disease status and survival Callahan et al. AAP Abstract 2016 Callahan et al. AAP Abstract 2016 Treatment of Pulmonary Vein Stenosis Treatment of Pulmonary Vein Stenosis Imatinib (Gleevec) and Bevacizumab (Avastin) Imatinib (Gleevec) and Bevacizumab (Avastin) Patient Population n = 48 Interventions before drug therapy Premature birth n = 18 (38%) Catheter-mediated n = 48 (100%) Genetic syndrome n = 13 (27%) median 2 (1 - 6)/patient Surgical n = 47 (98%) Congenital heart disease n = 38 (79%) median 1 (1 - 3)/patient Anomalous pulmonary venous connections n = 17 (35%) “sutureless” repair n = 40 (85%) Single ventricle physiology n = 6 (13%) Bilateral PVS n = 39 (81%) Interventions during or after drug therapy Median vessels involved 4 (range 2- 5) Catheter-mediated n = 42 (88%) median 3 (1 - 12)/patient Mean gradient ≥4 mmHg Surgical n = 2 (4%) Relatively high risk patients Callahan et al. AAP Abstract 2016 Callahan et al. AAP Abstract 2016 4
3/10/2017 Treatment of Pulmonary Vein Stenosis Treatment of Pulmonary Vein Stenosis Imatinib (Gleevec) and Bevacizumab (Avastin) Imatinib (Gleevec) and Bevacizumab (Avastin) Local recurrence with or without stabilization All Patients N = 48 Re-stenosis in previously affected veins Alive 37 (77%) Recurred 36 (75%) Progression with or without stabilization New or worsening disease in ≥ 2 veins Progressed 6 (13%) New obstruction in previously unaffected vein Stabilized 16 (33%) Proximal disease extending distally (upstream) New vein atresia Stabilization was associated with Absence of lung disease (p = 0.03) Stabilization Higher percentage of eligible drug doses received ≥ 6 months without recurrence or progression (90% vs. 83%; p = 0.03) Callahan et al. AAP Abstract 2016 Callahan et al. AAP Abstract 2016 Therapy for Pulmonary Vein Stenosis Therapy for Pulmonary Vein Stenosis Observation and Challenge Observation and Challenge 5
3/10/2017 Treatment of Pulmonary Hypertension Therapy for Pulmonary Vein Stenosis Associated with Pulmonary Vein Stenosis Observation and Challenge What is an acceptable pulmonary arterial pressure? Parallel Circulation 1/Rp (Total) = 1/Rp (R) + 1/Rp (L) 1/3 = 1/6 + 1/6 Single Lung (2 vessel disease) Rp = 6 units-m 2 CI = 3 L/min-m 2 Mean PAP = 25 mmHg RPAWP = 7 mmHg LPAWP = 23 mmHg Treatment of Pulmonary Hypertension Associated with Pulmonary Vein Stenosis Number of Mean Duration Patients, 13 (years) Nighttime Oxygen 11 9.7 (1.3-17.6) 7 8.5 (2.2-12.3) Calcium Channel Blocker Phosphodiesterase V Inhibitor 9 5.6 (1.1-10.9) Endothelin Receptor Antagonist 4 5.1 (0.3-14.1) 2 0.8 (0.6-1.0) Prostacyclin Analog Domingo et al. (preparing for submission) Domingo et al. (preparing for submission) 6
3/10/2017 Treatment of Pulmonary Hypertension Pulmonary Vein Stenosis Associated with Pulmonary Vein Stenosis Challenges Limited understanding Factors that cause stenosis Factors that result in the progression of disease Failure to collaborate and improve the quality of care Diversity in care Strategies to screen for and monitor stenosis No proven methods to treat inoperable stenoses Optimal timing of treatment is unknown Thank You! Pulmonary Vein Stenosis University of Utah and Primary Children’s Hospital Hope Opportunity to improve collaboration A network of individuals who care - Congenital heart surgeons - Interventional cardiologists - Providers committed to research and basic care Multiple disciplines - Scientists with expertise in vascular biology Final Disclosure - Families Ronald Day has no compelling desire to harm beavers. 7
Recommend
More recommend