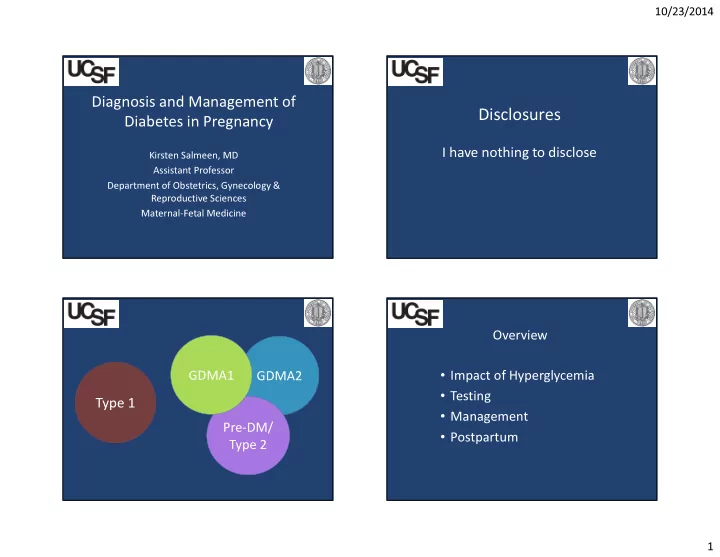
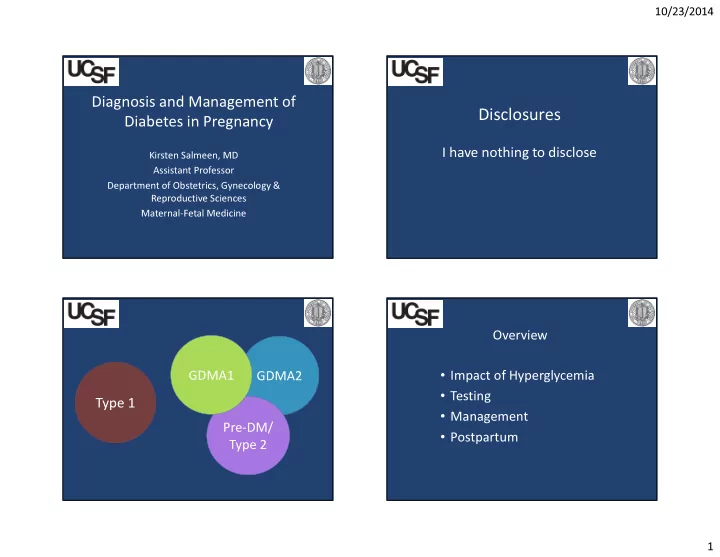
10/23/2014 Diagnosis and Management of Disclosures Diabetes in Pregnancy I have nothing to disclose Kirsten Salmeen, MD Assistant Professor Department of Obstetrics, Gynecology & Reproductive Sciences Maternal-Fetal Medicine Overview • Impact of Hyperglycemia GDMA1 GDMA2 • Testing Type 1 • Management Pre-DM/ • Postpartum Type 2 1
10/23/2014 Normal Glucose In Pregnancy: Glucose & Insulin Non Diabetics GLUCOSE PREGNANT NON-PREGNANT Normal Pregnancy: - Fasting HYPO glycemia INSULIN - Postprandial HYPER glycemia PREGNANT - HYPER insulinemia NON-PREGNANT Hernandez Diabetes Care 2011 Cunningham et al. Williams Obstetrics, 23rd Edition Glucose & Insulin – The Fetus Glucose & Insulin – Pregnancy • Transfer of glucose across placenta is by • Pregnancy = “Pancreatic Stress Test” facilitated diffusion via glucose transport proteins • Human placental lactogen blocks peripheral • Glucose is the primary substrate for fetal growth uptake and use of glucose in the mother • The fetus makes its own insulin • Insulin sensitivity is > 50% lower • Hyperinsulinemia likely drives excess fetal growth 2
10/23/2014 Pregnancy Outcomes in GDM Overview Approximate Overall % Relative Risk/Odds Ratio • Impact of Hyperglycemia Macrosomia 20 RR ~1.4 Pre-Eclampsia 15 RR ~1.7 • Testing Cesarean Section Varies RR ~ 1.2 Shoulder Dystocia 3-5 OR ~ 1.2 • Management IUFD ~ 0.05 RR ~ 2 • Postpartum HAPO Study Cooperative Research Group N Engl J Med 2008 Schmidt M Diabetes Care 2001 Wendland E BMC Pregnancy Childbirth 2012 Hyperglycemia & Pregnancy Hyperglycemia & Pregnancy Outcomes Outcomes Preeclampsia Macrosomia Cesarean Section Fasting Glucose Macrosomia (%) (%) (%) (%) 50 gram, 1-hour < 100 mg/dL 3.0 12.2 17.5 < 72 mg/dL 9.7 100 – 114 mg/dL 6.3 12.5 20.8 74-76 mg/dL 14.4 116 – 134 mg/dL 5.6 15.4 23.0 > 134 mg/dL 5.9 17.2 23.4 78-82 mg/dL 14.1 P-value for trend 0.01 0.001 0.001 > 82 mg/dL 20.5 Sermer et al AJOG 1995 Sermer et al AJOG 1995 3
10/23/2014 Hyperglycemia & Pregnancy Hyperglycemia & Pregnancy Outcomes Outcomes 2 hour 2 hour 2 hour 2 hour Odds Outcome (%) 95% CI Fasting Fasting Fasting Fasting Odds < 102 102-114 115-128 ≥ 130 Ratio Outcome (%) 95% CI < 74 74-77 79-81 ≥ 83 Ratio Birthweight 22.9 27.4 28.8 32.3 1.16 1.01-1.34 Birth weight ≥ 4000 g 23.4 27.9 28.5 31.7 1.14 1.06-1.22 ≥ 4000 g Birthweight 5.2 5.3 5.6 8.6 1.16 1.01-1.34 Birth weight > 4500 g 4.3 6.3 6.8 8.1 1.23 1.08-1.40 ≥ 4500 g LGA 16.0 20.7 21.1 27.2 1.23 1.13-1.33 LGA 17.2 18.9 22.7 25.6 1.19 1.10-1.29 PIH/PreE 4.8 6.9 8.4 7.2 1.16 1.02-1.31 PIH/PreE 5.8 6.6 7.1 7.9 1.12 0.99-1.26 Shoulder 0.4 1.2 1.8 2.9 1.78 1.32-2.40 Shoulder Dystocia 1.4 0.8 1.7 2.2 1.21 0.92-1.62 Dystocia Jensen AJOG 2001 Jensen AJOG 2001 HAPO Glucose Levels Level Fast (mg/dL) 1 hr (mg/dL) 2 hr (mg/dL) 1 < 75 ≤ 100 ≤ 90 • Does hyperglycemia without overt diabetes during pregnancy increase risk of adverse pregnancy outcomes? 2 75-79 106-132 91-108 3 80-84 133-155 109-125 • Blinded study of ~25,000 women at 15 centers in 9 countries 4 85-89 156-171 126-139 • Primary outcomes: birthweight > 90%ile for GA, primary CD, 5 90-94 172-193 140-157 neonatal hypoglycemia, cord-blood C-peptide level > 90%ile 6 95-99 194-211 158-177 7 ≥ 100 ≥ 212 ≥ 178 • Primary predictor: Levels of hyperglycemia HAPO Study Cooperative Research Group N Engl J Med 2008 HAPO Study Cooperative Research Group N Engl J Med 2008 4
10/23/2014 HAPO Results Impacts of Macrosomia – Maternal Weight Prolonged Labor (%) Excess Bleeding (%) CD (%) 3000 – 3999 g 0.9% 0.5 18 4000 – 4499 g 1.2 0.7 25.5 4500 – 4999 g 1.3 0.9 35.6 > 5000 g 1.5 1.1 50.6 Boulet SL et al. Am J Obstet Gynecol. 2003;188(5):1372-8; Acker et al. Obstet Gynecol. 1985;66:762; Nesbitt et al. Am J Obstet Gynecol. 1998;179:476; Sandmire et al. Int J Gynaecol Obstet. 1988;26:65; Overland E et al. Am J Obstet Gynecol. 2009;200(5):506 HAPO Study Cooperative Research Group N Engl J Med 2008 Impacts of Macrosomia - Impacts of Macrosomia – Fetal Childhood 3000 – 4,000 – 4,499 g 4,500 – 4,999 g ≥ 5,000 g P = 0.004 3999 g LGA Outcome % % OR CI % OR CI % OR CI 5 min 0.1 0.1 1.3 1.2-1.4 0.2 2.0 1.8-2.3 0.5 5.2 4.1-6.6 Apgar ≤ 3 P = 0.56 AGA LGA Assisted ventilation 0.3 0.3 1.2 1.1-1.2 0.5 1.9 1.7-2.0 1.3 4.0 3.5-4.6 AGA ≥ 30 min Birth 0.3 0.5 2 1.9-2.1 0.8 3.1 3.0-3.3 1.3 4.5 4.0-5.2 injury Neonatal Cumulative hazard (risk) function for development of metabolic Mortality 0.7 0.6 0.87 0.8-1 0.7 1.0 0.8-1.2 1.9 2.7 1.9-3.8 syndrome according to birth weight. Rate* * Per 1,000, < 28 days Gillman Pediatrics 2003 Boulet AJOG 2003 5
10/23/2014 Overview • Impact of Hyperglycemia • Increasing blood glucose (even without overt • Testing diabetes) is associated with worsening • Treatment pregnancy outcomes including macrosomia, • Postpartum pre-eclampsia and cesarean section in an approximately linear fashion. When to test? How are average-risk patients Initial Visit: screened for GDM in your practice? • Overweight/obese A. Two step testing (1-hour, 50 gram glucose • History of gestational diabetes or glucose intolerance loading test followed by fasting 3-hour, 100 gram • Prior LGA infant loading test if needed) at 24-28 weeks • Family history of type 2 DM B. One step testing (fasting 2-hour, 75 gram loading • Maternal age > 35 test at 24-28 weeks 57% • High-risk ethnic groups (non-Caucasian) C. Fasting blood sugar and/or hemoglobin A1c in • PCOS the first trimester D. A and C 21% 24 – 28 Weeks: E. B and C 13% • Everyone else 7% 2% • High-risk patients who screened negative earlier . . . C C . . . . . t t d . d d s s n n e e o t t o a a l p p b A B e e t t g s s n e i o t w n s O a T F 6
10/23/2014 GDM Testing Controversy What defines disease ? F 75-79 F 90-94 1 hr 172-193 1 hr 106-132 2 hr 140-157 2 hr 91-108 HAPO Study Cooperative Research Group. N Engl J Med. 2008. Sensitivity v Specificity In your opinion, what primary cesarean section rate defines disease? One-Step Two-Step Carpenter Coustan National Diabetes Data Group 35% Universal Screening Risk-Based Screening A. > 15% 30% Early Screening 24-28 Week Screening B. > 20% 24% Hemoglobin A1c No Hemoglobin A1c C. > 25% Testing for 1 abnormal value No f/u for 1 abnormal value 12% D. > 30% More Sensitive, Less Specific Less Sensitive, More Specific MORE women WITHOUT disease LESS women WITHOUT disease test positive test positive % % % % 5 0 5 0 1 2 2 3 > > > > 7
10/23/2014 Prenatal Outcomes and Screening One-Step vs. Two-Step Testing Strategies Two-Step GDM Normal GDM by by CC Glucose One-Step IADPSG (%) Step 1: (%) Tolerance (%) Non-Fasting, 50 g, 1 hr serum *Primary Fasting, 75 g, 1 & 2 hr serum IAD- 19.5 17.8 14.8 glucose measurement Cesarean PSG glucose measurement ≥ 130/140 mg/dL � Step 2 *Shoulder 1.2 0.71 0.91 Dystocia 1+ abnormal value � GDM Step 2: Fasting, 100 g, 3 hr glucose test *PPH 1.5 1.4 1.3 GDM prevalence ~ 20% 2+ abnormal values � GDM CC Control * Not statistically significant GDM prevalence ~ 5-10% Ethridge Obstet Gynecol 2014 Prenatal Outcomes and Screening Prenatal Outcomes and Screening Strategies Strategies Odds of Outcome compared to 1 hr, 50 g < 140 mg/dL Pregnancy outcomes among 1,750 women diagnosed with GDM by Carpenter- Coustan criteria and 1,526 women diagnosed by IADPSG criteria. Outcome OGTT Negative IADPSG (N=155) CDA (N=358) GDM Rate by CC = 10.6% (N=526) GDM rate by IADPSG = 35.5% * Composite 0.9 (0.8-1.2) 1.4 (1.1 – 1.9) 1.4 (1.1-1.8) 2-Step CC Criteria IADPSG Criteria PIH/Pre-E 0.9 (0.6-1.7) 3.0 (1.7-5.6) 1.2 (0.7-2.1) GDM NGT P: GDM NGT P: CD 1.1 (0.9-1.4) 1.4 (1.01-1.2) 1.3 (1.05-1.7) % % GDM vs NGT % % GDM vs NGT LGA (> 90%ile) 1.2 (0.9-1.6) 1.8 (1.1-2.9) 1.5 (1.1-2.2) Gest HTN 4.9 4.0 0.047 5.7 2.2 0.009 Delivery 0.049 0.026 * Composite of: hypertensive disorders, shoulder dystocia, 3 rd or 4 th degree Vaginal 57.9 58.4 69.7 73.2 laceration, LGA, NICU admission, neonatal: respiratory complication, CD 27.6 25.7 22.1 18.5 hypoglycemia, jaundice Forceps 14.5 15.9 8.2 8.3 CDA Guidelines: 1 hr, 50 g > 140 � 2 hr, 75 g < 95/191/160 LGA 4.9 4.6 0.9 4.8 3.2 0.04 Duran Diabetes Care 2014 Mayo AJOG 2014 8
Recommend
More recommend