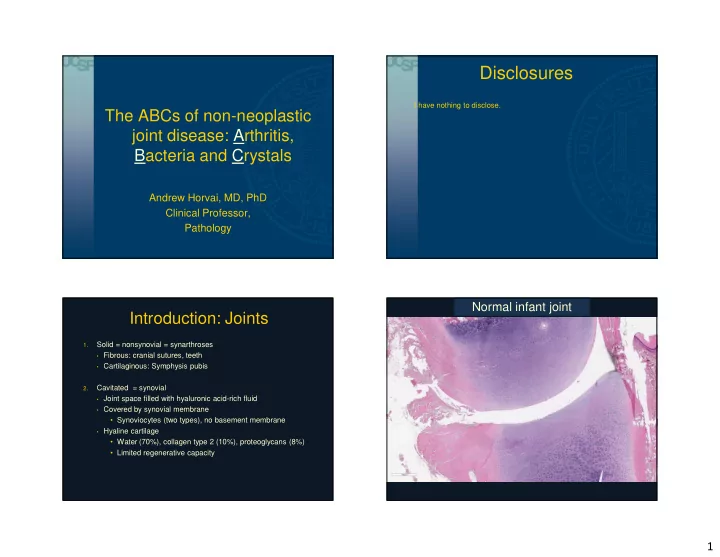
Disclosures I have nothing to disclose. The ABCs of non-neoplastic joint disease: Arthritis, Bacteria and Crystals Andrew Horvai, MD, PhD Clinical Professor, Pathology Normal infant joint Introduction: Joints Solid = nonsynovial = synarthroses 1. • Fibrous: cranial sutures, teeth • Cartilaginous: Symphysis pubis Cavitated = synovial 2. • Joint space filled with hyaluronic acid-rich fluid • Covered by synovial membrane • Synoviocytes (two types), no basement membrane • Hyaline cartilage • Water (70%), collagen type 2 (10%), proteoglycans (8%) • Limited regenerative capacity 1
Normal adult joint Normal synovium Non-neoplastic joint disease Osteoarthritis Definition: A degeneration of articular cartilage resulting in Noninfectious arthritis o o structural and functional failure of synovial joints o Osteoarthritis (OA) Clinical: o Rheumatoid arthritis (RA) o o Others o Most common disease of joints o Seronegative spondyloarthropathies o Incidence o Juvenile idiopathic arthritis (JIA) o Primary (oligoarticular): 40% of people over 70 o Crystal induced arthritis o Secondary (polyarticular): Rare, underlying disease, younger o Gout o Knee, hip, DIP and PIP joints o Pseudogout Pathogenesis o Infectious arthritis o o Chondrocyte injury, genetic predisposition, biomechanical o Septic (bacterial) arthritis o Cartilage degradation > repair o Infected arthroplasty o Loss of cartilage and chondrocytes o Lyme arthritis o Despite suffix – itis inflammation is minimal 2
Osteoarthritis Osteoarthritis: duplicated tidemark 3
Osteoarthritis: Schmorl’s node Osteoarthritis: subchondral cyst Rheumatoid arthritis Rheumatoid arthritis Definition: Chronic inflammatory, autoimmune disorder principally o attacking joints producing a nonsuppurative, proliferative and inflammatory arthritis Clinical o o Prevalance 1-5% o Female: Male 3:1 o MCP and PIP, wrist, elbow o Extraarticular: lung, kidney, soft tissue (rheumatoid nodule) Pathogenesis o o Genetics (HLA) + Environmental (infection, smoking) o T H 1 T H 17 and B cell responses to self antigens (citrullinated peptides) o Lymphocytes, antibodies and immune complex enter joint o Pannus, destruction of bone and cartilage, 4
Rheumatoid arthritis Rheumatoid arthritis Rheumatoid arthritis Rheumatoid arthritis 5
Rheumatoid nodule Rheumatoid nodule Arthritis summary Other non-infectious arthritis Seronegative spondyloarthropathies o o Sacroiliac joints o Pathology best seen in ligamentous attachments (entheses) o RhFactor-, association with HLA-B27 o Subtypes: Ankylosing spondylitis, reactive arthritis, enteritis associated arthritis, psoriatic arthritis Juvenile idiopathic arthritis o o Heterogeneous group of joint disorders, present before age 16 and persist for at least 6 weeks o Oligoarthritis, large joints o ANA+ RhFactor- Horvai A, Robbins Textbook of Pathology, Elsevier, 2015 6
Enthesopathy of Ankylosing spondylitis Ankylosing spondylitis Juvenile idiopathic arthritis Crystal induced arthritis 7
Gout (Calcium urate) arthritis Gout Definition: Transient attacks of acute arthritis initiated by urate o crystals within and around joints. Clinical: o o Incidence ~ 50 / 100,000 o M>F, renal failure, obesity predispose o Monoarticular acute arthritis, MTP joint most common o Asymptomatic intercritical period o Chronic tophaceous gout Pathogenesis o o Hyperuricemia (6.8 mg/dL) necessary but not sufficient o Most commonly due to reduced excretion of urate o Age, genetics, EtOH, obesity, thiazide diuretic o Urate crystals trigger inflammation, leukocyte recruitment Gout (alcohol process) Acute Gout arthritis (joint aspirate) 8
Gout (alcohol process) Gout Gout (polarized optics) Pseudogout (calcium pyrophosphate dihydrate, CPPD) Definition: Deposition of CPPD crystals in and around joints o causing acute, chronic or subacute arthritis. Clinical: o o May be asymptomatic; CPPD crystals may be secondary degenerative phenomenon in joints and soft tissue o M=F, >50 years old o Knees, elbows most commonly affected o Relapsing course, ~50% chronic joint damage similar to OA Pathogenesis o o Not known o Proteoglycans in articular cartilage normally inhibit mineralization, their loss may promote CPPD deposits 9
Pseudogout Pseudogout CPPD CPPD 10
CPPD (polarized optics) Infectious arthritis Septic (bacterial) arthritis Septic arthritis Definition: Pyogenic or granulomatous infection of synovium and articular o surfaces Other Clinical: o Gram o Fever, swollen, erythematous, painful joint negative o Synovial fluid grey-green, 20K-200K WBC/ µ L, >75% PMN S. aureus o Compared to osteomyelitis, joint infection is a more urgent problem S. because cartilage has limited appear to regenerate Pneumoniae Pathogenesis o o Inoculation of joint by infectious organisms o Usually bacterial o Hematogenous S. pyogenes o Periosteal o Direct 11
Septic arthritis Septic (bacterial) arthritis Definition: Pyogenic or granulomatous infection of synovium and o articular surfaces Orthopedic hardware (joint prostheses) at high risk o Lyme arthritis o o Infection with Borrelia burgdorferi o 10% develop arthritis in late stage, large joints (since most cured) o Borrelia in joints (~25% by Warthin Starry, ~50% by PCR) Infectious arthritis Infectious arthritis 12
Infectious arthritis Infectious arthritis Granulomatous infectious arthritis Infected arthroplasty 13
Hardware loosening Infected arthroplasty Early Late • Aseptic loosening (85%) • Septic loosening (15%) • Wear induced particle Time <3 months > 24 months debris • Infection S. Aureus Coag – Staph Organisms E. Coli P. Acnes • Stress shielding (atrophy) Route Direct Hematogenous • Hardware failure Clinical Fever Loosening ↑ WBC Instability Pain Pain Removal Antibiotic cement spacer The “delayed” form (3-24 months) with overlapping features � Immediate replacement 6 wks IV antibiotics between Early and Late. Septic loosening Septic loosening � Gold standard: Positive culture from multiple sites � Intraoperative: Neutrophils in synovium or granulation tissue or capsule Criterion Sensitivity Specificity Feldman 5 neutrophils/hpf in > 5 hpf* 25% 98% Athanasou 10 neutrophils/10 hpf 70% 64% *hpf: 400X (0.5 mm 2 ) high power field. Bori G et al. J Bone Joint Surg 2007 89:1232 14
Septic loosening PMNs in capsule: YES PMNs in fibrin: NO PMNs in vessels: NO 15
Wear debris reaction Other common arthroplasty findings Wear debris reaction � Xanthoma cells � Capsule (synovial metaplasia) � Foreign materials � � Barium: radio-opaque contrast � Methyl methacrylate: cement � Polyethylene: articular surface (large prosthesis) � Silastin: silicone rubber (small prosthesis) Rosenberg, A. E., et al. (2011). Semin Diagn Pathol 28(1): 65-72. Wear debris reaction Xanthoma cells 16
Barium and Me-Methacrylate Polyethylene Polyethylene Lyme disease Horvai A, Robbins Basic Pathology, Elsevier, 2017. 17
Lyme arthritis (images courtesy Dr. M. Klein, HSS) Take-home messages 1. Osteoarthritis, the most common joint disease, usually lacks inflammation 2. Lymphoid follicles with germinal centers is consistent with rheumatoid arthritis but is seen in other autoimmune arthritides 3. Neutrophils in fibrin and vascular lumina do not count for septic loosening of a prosthesis 4. CPPD crystals can occur as a secondary phenomenon in degenerative joints for various reasons and are not diagnostic of pseudogout 18
Recommend
More recommend