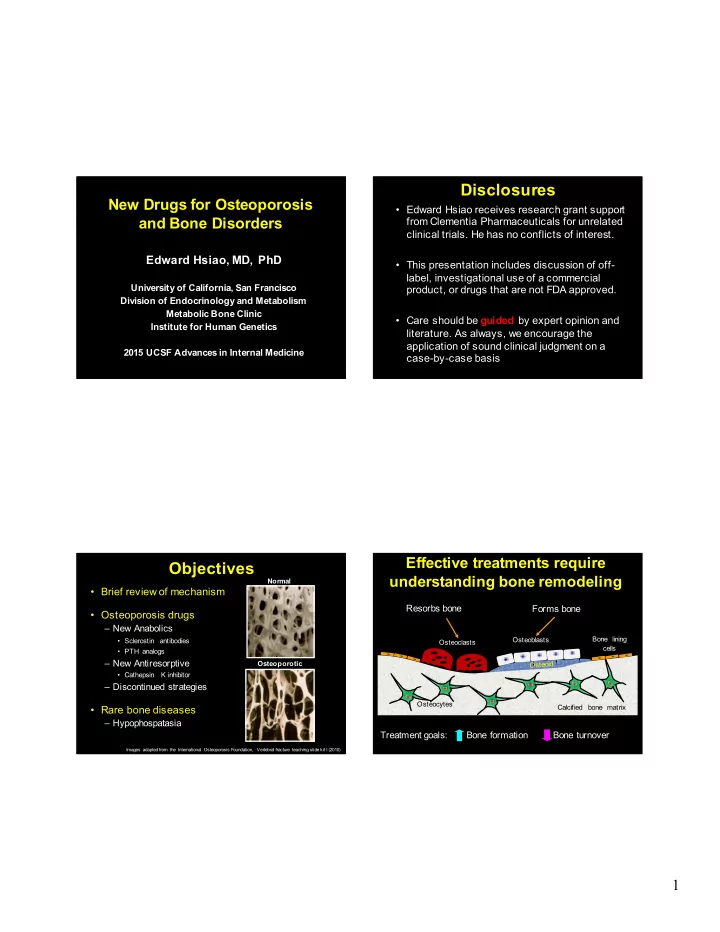
Disclosures New Drugs for Osteoporosis • Edward Hsiao receives research grant support and Bone Disorders from Clementia Pharmaceuticals for unrelated clinical trials. He has no conflicts of interest. Edward Hsiao, MD, PhD • This presentation includes discussion of off- label, investigational use of a commercial University of California, San Francisco product, or drugs that are not FDA approved. Division of Endocrinology and Metabolism Metabolic Bone Clinic • Care should be guided by expert opinion and Institute for Human Genetics literature. As always, we encourage the application of sound clinical judgment on a 2015 UCSF Advances in Internal Medicine case-by-case basis Effective treatments require Objectives understanding bone remodeling Normal • Brief review of mechanism Resorbs bone Forms bone • Osteoporosis drugs – New Anabolics Bone lining Osteoblasts • Sclerostin antibodies Osteoclasts cells • PTH analogs – New Antiresorptive Osteoporotic • Cathepsin K inhibitor – Discontinued strategies Osteocytes Calcified bone matrix • Rare bone diseases – Hypophospatasia Treatment goals: Bone formation Bone turnover Images adapted from the International Osteoporosis Foundation, Vertebral fracture teaching slide kit I (2010) 1
Current Treatments for Recent Changes in Drugs Osteoporosis for Osteoporosis Increase Bone Formation Decrease Bone Turnover • Parathyroid hormone • Hormone Therapy (HT) • Anabolics • Antiresorptives (rPTH, Teriparatide) • SERM/Raloxifene (Evista) – Anti-sclerostin – Cathepsin K inhibitor • Calcitonin (Miacalcin) antibodies • Ondanacatib • Bisphosphonates • Romosozumab – New considerations • Blomosozunab – Alendronate (Fosamax) for denosumab – Risedronate (Actonel) – PTHrP analog – Ibandronate (Boniva) – Restrictions on – Zoledronate (Reclast/Aclasta) • Abaloparatide strontium ranelate (in • (Strontium ranelate) EU market) • RANKL inhibitors – Vibration Therapy – Denosumab (Prolia) Sclerostin is a Key Mediator Recent Changes in Drugs of Bone Formation for Osteoporosis X Sclerosteosis Wnt Sclerostin X • Anabolics • Antiresorptives – Anti-sclerostin – Cathepsin K inhibitor antibodies LRP5/6 • Ondanacatib Frizzled • Romosozumab – New considerations • Blomosozunab for denosumab Normal – PTHrP analog – Restrictions on β-Catenin • Abaloparatide strontium ranelate (in EU market) Activation of bone – Vibration Therapy Formation pathways Brunkow et al. Am J Hum Gen 2001 2
Anti-Sclerostin Antibody #1: Romosozumab: Phase I Romosozumab • Additional Phase I study • Romosozumab (Amgen/UCB: AMG785, CDP7851) – Multiple doses – Humanized monoclonal antibody – 32 postmenopausal women with low bone mass • Phase 1 study: • 6 doses, 1-2 mg/kg every 2 weeks, or – Single dose of AMG785, 72 men and women; – Peak serum concentration achieved after 1 week sq • 3 doses of 2-34 mg/kg every 4 weeks, or – Half life of 11-18 days placebo – Dose ranging was done from 0.1-10 mg/kg – 16 healthy men with low bone mass. – 10mg/kg (maximum dose tested) • 1 mg/kg every 2 weeks, or • 120-184% increase in P1NP, BSAP, Osteocalcin • 54% decrease in CTX • 3 mg/kg every 4 weeks, or placebo • Largest BMD effect at day 85 • +5.3% lumbar spine BMD • + 2.8% in total hip BMD Padhi, et al. JBMR 2011 Padhi, et al. J Clin Pharm 2014 Romosuozumab Romosozumab: Phase II • 419 postmenopausal women – T score between -2.0 and -3.5 in spine, total hip or femoral neck. – Monthly sq (70, 140, or 210 mg) or every 3 months (140 or 210 mg), for 12 months – Open label comparison to • 12 weeks of drug, 12 weeks of followup • Alendronate 70 mg weekly • Teriparatide 20 ug/day • Appropriate changes in serum markers observed. • No major effect on hip BMD • Persistence of effect after dosing stopped Padhi, et al. J Clin Pharm 2014 3
Romosozumab Gives Romosozumab: Phase III Higher Increase in BMD • Recent announcements indicate that it meets goals, but full publications pending • STRUCTURE trial* (Sept 2015 press release) – 436 postmenopausal women previously treated with bisphosphonates – Romosozumab vs teriparatide – Met goals for total hip BMD • FRAME trial** (Feb. 2016 press release) – 7180 patients, 210 mg sq/month – Reduced incidence of new vertebral fractures at 12 and 24 mo • Every 3 months – same as 70 mg/mo dose – Reduced incidence of clinical fractures at 12 mo – Unclear benefit for non-clinical fractures at 12 and 24 mo. – Approx 5% increase in BMD at spine – Bone formation markers return to normal after 6-12 mo *STudy evaluating effect of RomosozUmab Compared with Teriparatide in postmenopaUsal women with osteoporosis at high risk for fracture pReviously treated with bisphosphonatE therapy ** FRActure study in postmenopausal woMen with ostEoporosis Anti-sclerostin Antibody #2: Romosozumab Side Effects Blosozumab (Reported in Phase I-III) • Injection site reactions • Humanized monoclonal antibody • No clear increase in serious adverse events – Eli Lilly (LY2541546) over alendronate, teriparatide • 20% develop binding antibodies, with 3% • Phase I trials showing in vitro blocking ability, but subjects – Single and multiple dose regimens tolerated up to still showed biologic response 750 mg every 2 weeks for 8 wks – 3.4-7.7% increase in lumbar BMD at Day 85 • Awaiting results of Phase III for full profile McColm, et al. JBMR 2014 4
23996473 Blosozumab: Phase II Blosozumab: Phase II Durability of treatment • 120 postmenopausal women, T score between -2.0 and -3.5 • Followup study for 1 year post treatment – 88 of 120 women previously studied Lumbar Spine Total Hip – Suggests antiresorptive will be needed Recker, et al. JBMR 2015 Recknor, et al. JBMR 2015 Osteoblast Activation by PTHrP: Recent Changes in Drugs Parathyroid Hormone Related Protein for Osteoporosis PTH/PTHrP Receptor • Anabolics • Antiresorptives PTHrP PTH – Anti-sclerostin – Cathepsin K inhibitor antibodies Osteoblasts Bone lining • Ondanacatib cells • Romosozumab – New considerations • Blomosozunab for denosumab – PTHrP analog G s GPCR bone – Restrictions on • Abaloparatide strontium ranelate (in anabolic response Calcified bone matrix EU market) – Vibration Therapy Treatment goals: Bone formation Bone turnover 5
Abaloparatide: A PTHrP analog Abaloparatide: Phase III • Synthetic peptide analog of human • ACTIVE fracture prevention trial PTHrP – 2463 postmenopausal women • Phase II: – 18 mo daily 80 ug abaloparatide vs placebo vs 20 ug teriparatide. – 24 weeks of daily sq injections – 89% decrease in new fracture rate vs. placebo • Postmenopausal women – Teriparatide showed an 80% decrease • 20, 40, or 80 ug vs 20 ug of teriparatide • No significant differences in wrist fractures • Increased BMD in spine and hip at 6, 12, and 18 months – Lumbar spine BMD increased 2.8-6.7%, vs – Major complications: hypercalcemia, and injection site 5.5% in teriparatide and 0.8% in placebo reactions. – Femoral neck increased 1.4-2.6%, vs. • Extension trial in progress 0.5% in teriparatide and 0.4% in placebo Leder, et al. JCEM 2015 2015 Endocrine Society poster: LB-OR01-3 Cathepsin K: Functions in Recent Changes in Drugs Osteoclast Resorption Pits for Osteoporosis Resorbs bone • Anabolics • Antiresorptives – Anti-sclerostin – Cathepsin K inhibitor Cathepsin K antibodies Osteoclasts • Ondanacatib - secreted by osteoclasts • Romosozumab - cleaves helical collagen – New considerations • Blomosozunab - induces bone resorption for denosumab – PTHrP analog – Restrictions on • Abaloparatide strontium ranelate (in Osteocytes EU market) – Vibration Therapy Treatment goals: Bone formation Bone turnover 6
Ondanacatib: Phase II Ondanacatib: Anti-Cathepsin K • Related to two other Cathepsin K inhibitors – Relacatib: nonselective inhibitor of K, L, V, and S • No clinical information • Kumar, et al. Bone 2007 (monkey model) – Balicatib: showed BMD increases, but had cutaneous adverse events. • Adami, et al. JBMR 2006 • 399 postmenopausal women – Ondanacatib: selective for Cathepsin K and orally – Generally well tolerated bioavailable. – No significant major side effects reported • Bone, et al. JBMR 2009 Denosumab Recent Changes in Drugs • Human monoclonal antibody that inhibits RANKL (required for for Osteoporosis osteoclast function and survival) • Given 60 mg sq every 6 months over 3 years reduces fracture risk (FREEDOM) and Freedom extension • Anabolics • Antiresorptives – Anti-sclerostin – Cathepsin K inhibitor Vertebral Non- Hip N vertebral (Ref #) antibodies • Ondanacatib Alendronate 0.55 0.84 0.60 12,068 • Romosozumab (0.43-0.69) (0.74-0.94) (0.40-0.92) (2) (10 mg qd) – New considerations • Blomosozunab Zoledronate 0.30 0.75 0.59 7,765 for denosumab (5 mg/yr iv) (0.24-0.38) (0.64-0.87) (0.42-0.83) (1) – PTHrP analog – Restrictions on Denosumab 0.32* 0.80* 0.60 7868 • Abaloparatide strontium ranelate (in (60 mg/6 mo sq) (0.26-0.41) (0.67-0.95) (0.37-0.97) (3) EU market) Relative risk of drug vs. placebo * Hazard ratios (secondary endpoints of study) – Vibration Therapy 1. Black, et al. NEJM 2007 (HORIZON) 2. Wells, et al. Cochrane DB or Syst. Rev. 2008 (CD001155 Alendronate) 3. Cummings, et al. NEJM 2009 (FREEDOM) 7
Recommend
More recommend