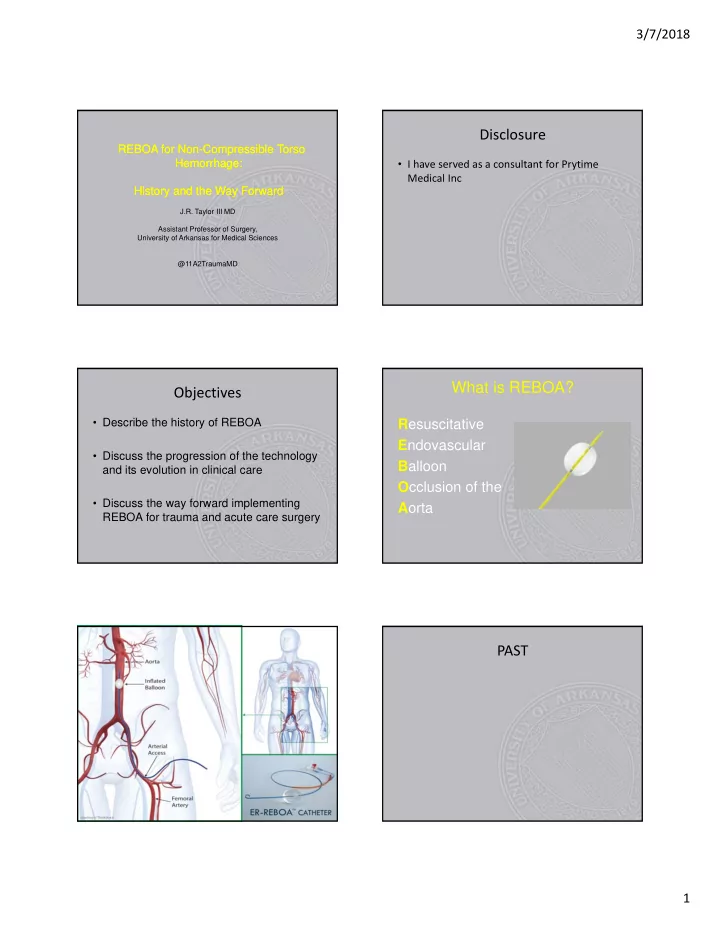
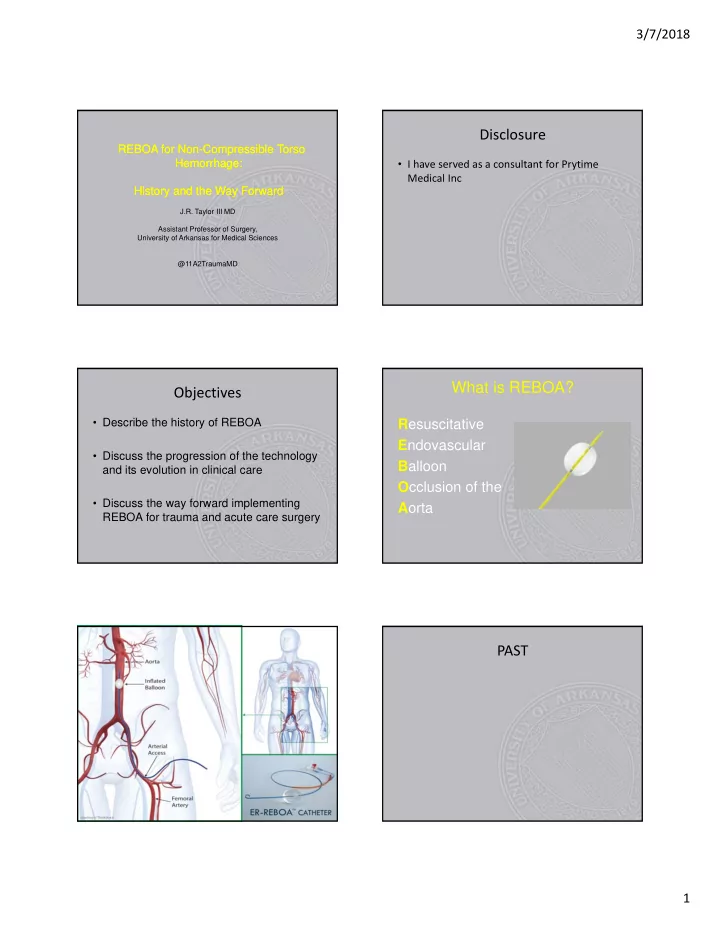
3/7/2018 Disclosure REBOA for Non-Compressible Torso REBOA for Non-Compressible Torso Hemorrhage: Hemorrhage: • I have served as a consultant for Prytime Medical Inc History and the Way Forward History and the Way Forward J.R. Taylor III MD Assistant Professor of Surgery, University of Arkansas for Medical Sciences @11A2TraumaMD What is REBOA? Objectives • Describe the history of REBOA R esuscitative E ndovascular • Discuss the progression of the technology B alloon and its evolution in clinical care O cclusion of the • Discuss the way forward implementing A orta REBOA for trauma and acute care surgery PAST 1
3/7/2018 Korean War Medical Advances • MASH Unit • Helicopter as flying ambulance • Blood collection and distribution using plastic containers • Body armor • First attempted during the Korean War • Two patients with intra-abdominal hemorrhage • Placed AFTER patients received >10 units blood • Catheter placed through femoral artery • Balloon inflated at level of diaphragm 2
3/7/2018 PRESENT OIF / OEF / GWOT Medical Advances • Tourniquets • Improved body armor • Golden hour • Damage control resuscitation Five Steps: 1.Obtain femoral arterial access 2.Balloon selection and positioning 3.Balloon inflation 4.Balloon deflation 5.Sheath removal – Closure of arteriotomy – Confirm distal pulses 3
3/7/2018 Aortic Occlusion Zones • Select zone of occlusion based upon injury pattern • Zones I and III preferred • Avoid occlusion in Zone II • Confirm zone of occlusion on plain x ray or fluoroscopy Conclusions from this series • REBOA is a feasible and effective means of proactive aortic control for patients in end- stage shock from blunt and penetrating mechanisms • Can be safely placed by Acute Care Surgeons with some, but no formal, vascular training • More studies necessary to define population where REBOA is truly beneficial Overall (N = 96) Resuscitative REBOA p value Thoracotomy (n=72) (n=24) Age 30.5(23.5, 48) 41 (24,62) 0.33 Median (P25,P75) Male %(n) 87.5% (63) 79.2%(19) 0.33 Blunt %(n) 44.4% (32) 66.7% (16) 0.10 ISS 34 (22,59) 29 (19,41) 0.17 Median (P25,P75) AIS Head 3 (0,5) 4 (3,5) 0.29 Median (P25,P75) AIS Chest 3 (3,4) 3.5 (3,4) 0.91 Median (P25,P75) AIS Abdomen 2 (0,4) 3 (2,4) 0.26 Median (P25,P75) AIS Extremity 1.5 (0,3) 4 (3,4) <0.001 Median (P25,P75) Survival Rate % (n) 9.7% (7) 37.5% (9) 0.003 4
3/7/2018 Among Deaths Resuscitative REBOA Deaths (N=80) Thoracotomy (n=15) p value Comparison of Cause of ICU Deaths (n=65) Death All Deaths %(n) 90.3% (65) 62.5% (15) 0.003 Died in ED %(n) 69.2% (45) 26.7% (4) <0.001 RT ICU Deaths (n=14) REBOA ICU Deaths Died in OR %(n) 9.2% (6) 20% (3) 0.69 (n=8) Died in ICU %(n) 21.6% (14) 53.3% (8) 0.17 Early death from hemorrhage 71.4% (10) 0% (0) %(n) Age Median 31 (24,46) 40.5 (24,66) 0.41 Multiple organ failure %(n) 14.3% (2) 12.5% (1) (P25,P75) Male %(n) 87.7% (57) 73.3% (11) 0.22 Head injury %(n) 14.3% (2) 87.5% (7) Blunt %(n) 44.6% (29) 73.3% (11) 0.08 ISS Median 35.5 (22,67) 34 (20,45.5) 0.39 (P25,P75) Comparison of Survivors Conclusions from this series Among Resuscitative REBOA • Use of REBOA in patient with noncompressible Survivors Thoracotomy Alive (n=9) p value hemorrhage from abdomen and pelvis is feasible and (N=16) Alive (n=7) effectively controls hemorrhage Survivors % (n) 9.7% (7) 37.5% (9) 0.003 Age Median 29 (21,51) 43 (25,59) 0.71 • Patients undergoing REBOA have at least equivalent (P25,P75) overall survival and fewer early deaths Male % (n) 85.7% (6) 88.9% (8) 1.00 Blunt % (n) 42.9% (3) 55.6% (5) 1.00 • Any patient with a suspected or confirmed major ISS Median 29 (16,34) 26 (17,29) 0.56 intrathoracic injury and cardiovascular collapse should (P25,P75) still undergo resuscitative thoracotomy 5
3/7/2018 Case Example 1 • 42 y/o male crushed between two cranes while at work • Presented to the OSH with a GCS 15, hypotension intubated at OSH, hypotensive, placed in pelvic binder transferred to MHH • VS @ presentation, SBP 60, HR 120, normal cxr, pelvis xray Case Example 1 • Cordis placed, right femoral arterial line place, pelvic binder moved inferiorly • Persistent hypotension right femoral REBOA placed SBP improved to 130 • Taken to the CT scanner and subsequently to the interventional radiology suite for angiography +/- embolization 6
3/7/2018 Case Example 1 • Angiography without evidence of actively bleeding arterial source REBOA removed, sheath maintained in right groin • RUG showed prostatic urethral injury, so percutaneous SP tube placed • Taken to the operating room found to have mesenteric injury with devitalized small bowel segment x 2 small bowel resection with HS anastomosis x 2, no other injury, NJ feeding tube placed, fascia closed • Sheath removed after hemodynamics normalized, coagulopathy corrected Case Example 1 Case Example 2 • POD 1 went for placement of uniplanar • 41 y/o male s/p auto-pedestrian with external fixator anterior pelvis, closed traumatic right lower extremity amputation below the knee reduction percutaneous screw fixation of right SI joint disruption, closed reduction • OSH intubated patient, placed right lower extremity proximal tourniquet and transferred percutaneous screw fixation left sacral to MH fracture • At evaluation, BP 60/40 52/30 massive transfusion protocol started, right femoral arterial line placed, left subclavian cordis 7
3/7/2018 Case Example 2 • FAST initially negative then positive with massive transfusion • 7FR sheath exchanged for right femoral arterial line REBOA deployed to Zone I Case Example 2 Case Example 2 • Taken to the OR for exploratory laparotomy • Taken to STICU overnight for resuscitation • At laparotomy found to have multiple Grade • 7FR sheath pulled at bedside once TEG III liver lacerations that underwent normalized 72 hour post removal duplex hepatorraphy and packing wound vac showed no evidence of pseudoaneurysm placed • Taken next day to OR for pack removal • Right lower extremity mangled and non- without evidence of further bleeding and salvageable gigli amputation undertaken formalization of AKA • After liver packing and hepatorraphy balloon • Discharged to rehab after 41 day hospital deflated, hemodynamics maintained, and balloon removed stay Case Example 3 • 34 y/o male with GSW to left thigh • Taken to OSH where improvised tourniquet was placed 8
3/7/2018 Case Example 3 • Given hasty tourniquet right femoral artery access was obtained, 7FR sheath placed and REBOA deployed but not inflated • Tourniquet removed, vascular control obtained, and balloon removed without inflation Case Example 3 • Destructive injury to SFA, shunt placed 2 hours after time of injury • Artery repaired with reverse saphenous vein graft • Discharged from hospital on POD 3 Future Prehospital REBOA 9
3/7/2018 Emergency Room Use Non ‐ Trauma 10
3/7/2018 Acute Care Surgery Endovascular Training for Acute Care Surgeons • BEST Basic Endovascular Skills for Trauma Course coordinated by the American College of Surgeons Committee on Trauma • Endovascular procedures on vascular surgery rotations aren’t just for fellows / chiefs it is a skill that translates to other parts of surgery 11
3/7/2018 Questions? 12
Recommend
More recommend