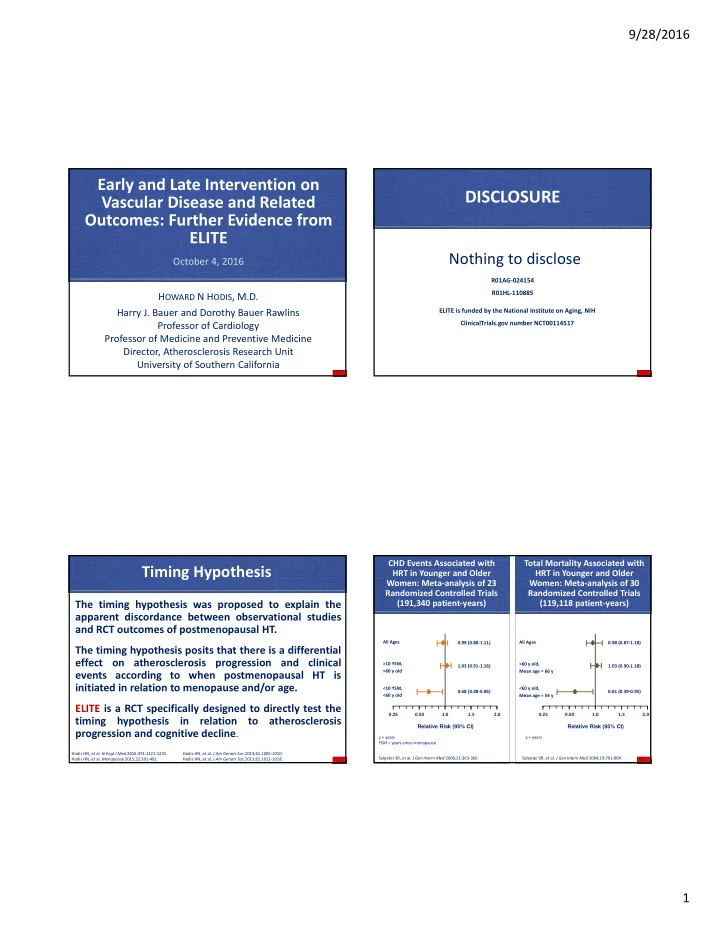
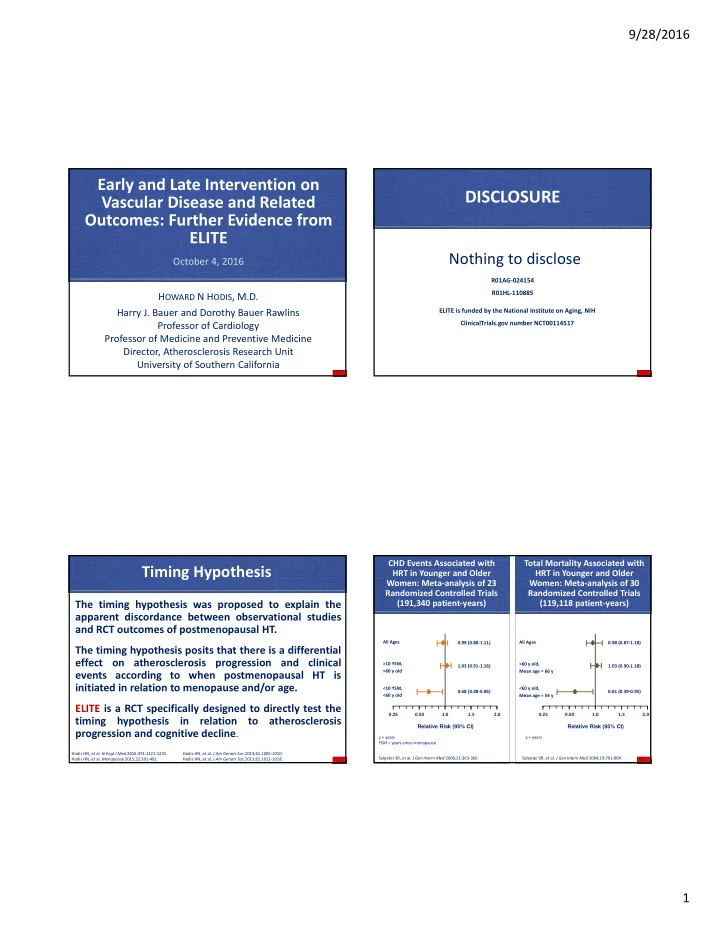
9/28/2016 Early and Late Intervention on DISCLOSURE Vascular Disease and Related Outcomes: Further Evidence from ELITE Nothing to disclose October 4, 2016 R01AG ‐ 024154 R01HL ‐ 110885 H OWARD N H ODIS , M.D. Harry J. Bauer and Dorothy Bauer Rawlins ELITE is funded by the National Institute on Aging, NIH Professor of Cardiology ClinicalTrials.gov number NCT00114517 Professor of Medicine and Preventive Medicine Director, Atherosclerosis Research Unit University of Southern California CHD Events Associated with Total Mortality Associated with Timing Hypothesis HRT in Younger and Older HRT in Younger and Older Women: Meta ‐ analysis of 23 Women: Meta ‐ analysis of 30 Randomized Controlled Trials Randomized Controlled Trials The timing hypothesis was proposed to explain the (191,340 patient ‐ years) (119,118 patient ‐ years) apparent discordance between observational studies and RCT outcomes of postmenopausal HT. All Ages 0.99 (0.88 ‐ 1.11) All Ages 0.98 (0.87 ‐ 1.18) The timing hypothesis posits that there is a differential effect on atherosclerosis progression and clinical >10 YSM, >60 y old, 1.03 (0.91 ‐ 1.16) 1.03 (0.90 ‐ 1.18) >60 y old Mean age = 66 y events according to when postmenopausal HT is initiated in relation to menopause and/or age. <10 YSM, <60 y old, 0.68 (0.48 ‐ 0.96) 0.61 (0.39 ‐ 0.95) <60 y old Mean age = 54 y ELITE is a RCT specifically designed to directly test the 0.25 0.50 1.0 1.5 2.0 0.25 0.50 1.0 1.5 2.0 timing hypothesis in relation to atherosclerosis Relative Risk (95% CI) Relative Risk (95% CI) progression and cognitive decline . y = years y = years YSM = years ‐ since ‐ menopause Hodis HN, et al. N Engl J Med 2016;374:1221 ‐ 1231. Hodis HN, et al. J Am Geriatr Soc 2013;61:1005 ‐ 1010. Salpeter SR, et al. J Gen Intern Med 2006;21:363 ‐ 366. Salpeter SR, et al. J Gen Intern Med 2004;19:791 ‐ 804. Hodis HN, et al. Menopause 2015;22:391 ‐ 401. Hodis HN, et al. J Am Geriatr Soc 2013;61:1011 ‐ 1018. 1
9/28/2016 Cochrane Meta ‐ analysis: Cochrane Meta ‐ analysis: Relative Risk of CHD: Observational Randomized Controlled Trials of All ‐ Cause Mortality from Studies and Randomized Trials CHD Events Associated with HRT Randomized Controlled Trials of in Younger and Older HRT in Younger and Older Postmenopausal Women Postmenopausal Women Observational Studies 0.64 Age 30 ‐ 55 y Time Since Menopause <6 y 0.68 HRT Randomized Trials Age <60 y 0.52 Time Since Menopause <10 y >10 YSM, >10 YSM, 1.07 (0.96 ‐ 1.20) 1.06 (0.95 ‐ 1.18) >60 y old >60 y old DOPS 0.48 Age 50 y Time Since Menopause 7 mo <10 YSM, <10 YSM, 0.52 (0.29 ‐ 0.96) 0.70 (0.52 ‐ 0.95) <60 y old <60 y old 0.59 RUTH 0.25 0.50 1.0 1.5 0.25 0.50 1.0 1.5 2.0 Age <60 y Relative Risk (95% CI) Relative Risk (95% CI) y = years y = years Grodstein F, et al. Prog Cardiovasc Dis 1995;38:199 ‐ 210. 0.5 1.0 YSM = years ‐ since ‐ menopause YSM = years ‐ since ‐ menopause Salpeter SR, et al. J Gen Intern Med 2006;21:363 ‐ 366. Risk Estimate Schierbeck LL, et al. BMJ 2012; 2012;3456:e6409. Collins P, et al. Circulation 2009;119:922 ‐ 930. Boardman HMP, et al. Cochrane Database of Systemic Reviews 2015, Issue 3:CD002229. DOI: 10.1002/14651858.CD002229.pub4. Boardman HMP, et al. Cochrane Database of Systemic Reviews 2015, Issue 3:CD002229. DOI: 10.1002/14651858.CD002229.pub4. EPAT: Rate of CIMT Change Pathogenic Sequence of Vascular Aging Hodis HN, et al. Ann Intern Med 2001;135:939 ‐ 953. 0.02 Rate of CIMT Change (mm/year) No HRT Placebo Adventitia P = 0.002 MMP ‐ 9 0.015 Estradiol Media Fibrous Cap Fibrous 0.01 Cap Internal Elastic Fibrous P = 0.045 Lamina Cap 0.005 Necrotic Necrotic Core Core P = 0.92 Plaque Plaque Plaque 0 Fatty Streak EPAT = HRT Early & Continued N = 199 N = 77 N = 122 ‐ 0.005 HRT No Lipid Lipid All Subjects Lowering Meds Lowering Meds WELL ‐ HART: Change in Percent Diameter Stenosis Hodis HN, et al. N Engl J Med 2003;349:535 ‐ 545. P=0.66 Change in Percent Diameter 2.80 Stenosis From Baseline WELL ‐ HART = HRT Late 2.40 of Atherosclerosis HRT 2.00 Progression 1.60 Mural Thrombus 1.20 0.80 0.40 Age 35 ‐ 45 years Age 45 ‐ 55 years Age 55 ‐ 65 years Age >65 years 0.00 Placebo Estradiol Estradiol + MPA (n = 59) (n = 53) (n = 54) Hodis HN, et al. N Engl J Med 2003;349:535–545. 2
9/28/2016 Estrogen Inhibits Initiation but not Importance of Timing of Intervention on Progression of Established Lesions in Mice the Effect of Estrogens on Atherogenesis in Nonhuman Primates New Lesions Established Lesions Number of Mice with Lesions Number of Mice with Lesions 10 10 Premenopausal Years Postmenopausal Years Plaque Area 9 9 Ovariectomy (% of Placebo) 8 8 7 7 70% 1,2 1. Healthy diet CEE + atherogenic diet 6 6 5 5 4 4 2. Atherogenic diet CEE + atherogenic diet 50% 3 3 3 2 2 Atherogenic Healthy diet 1 1 3. Healthy diet 0% 4 0 diet + CEE 0 4 10 16 22 28 34 40 4 10 16 22 28 34 40 ~ 6 Year Human Weeks Weeks Equivalent Iliac -E2 Iliac +E2 Carotid -E2 Carotid +E2 Time 1 Clarkson et al. J Clin Endocrinol Metab 1998;83:721. 3 Clarkson et al. J Clin Endocrinol Metab 2001;86:41. Rosenfeld ME, et al. Atherosclerosis 2002;164:251 ‐ 259. 2 Adams et al. Arterioscler Thromb Vasc Biol 1997;17:217. 4 Williams et al. Arterioscler Thromb Vasc Biol 1995;15:827. ELITE – Design ELITE – Trial Outcomes Study design: Single ‐ center, randomized, double ‐ blinded, placebo ‐ controlled trial PrimaryOutcome – Subclinical carotid artery atherosclerosis: Trial factors: Randomized treatment (estradiol, placebo) x time since menopause (<6 years, >10 years) Rate of change in common carotid artery intima ‐ media thickness (measured every 6 months) Subjects: 643 healthy postmenopausal women without preexisting CVD and diabetes mellitus Secondary Outcome – Cognition: Intervention: Oral micronized 17 β‐ estradiol 1 mg/d Change in verbal memory, executive function and global (+ vaginal micronized progesterone gel 45 mg/d x 12 days every month in women with a uterus) cognition tested at 2.5 years and 5.0 years Placebos Follow ‐ up: Every month for the first 6 months and then every 2 months for up to 6 years Hodis HN, et al. N Engl J Med 2016;374:1221 ‐ 1231. Hodis HN, et al. N Engl J Med 2016;374:1221 ‐ 1231. Hodis HN, et al. Menopause 2015;22:391 ‐ 401. Hodis HN, et al. Menopause 2015;22:391 ‐ 401. 3
9/28/2016 Carotid Artery Wall Imaging 2166 screened by telephone Carotid Artery Intima ‐ Media Thickness (CIMT) 5 5 895 screened in 4.5 4.5 clinic 4 4 p trend < 0.01 p trend < 0.01 3.5 3.5 Scanner Relative Risk 3 3 Transducer <6 years since menopause >10 years since menopause 2.5 2.5 643 randomized 2 2 N = 271 N = 372 1.5 1.5 Skin surface 1 1 137 allocated to 134 allocated to 186 allocated to 186 allocated to 0.5 0.5 Estradiol Placebo Estradiol Placebo Jugular vein 0 0 MI, Coronary Death All Cardiovascular Events Common Carotid artery < 0.011 mm/yr 0.018 ‐ 0.034 mm/yr 0.011 ‐ 0.018 mm/yr > 0.034 mm/yr 125 CIMT 123 CIMT 172 CIMT 176 CIMT Far wall carotid artery follow ‐ up follow ‐ up follow ‐ up follow ‐ up Hodis HN, et al. Ann Intern Med 1998;128:262 ‐ 269. Hodis HN, et al. Ann Intern Med 2001;135:939–953. Hodis HN, et al. N Engl J Med 2016;374:1221 ‐ 1231. Hodis HN, et al. Circulation 2002;106:1453–1459. Hodis HN, et al. Menopause 2015;22:391 ‐ 401. Baseline Clinical, Laboratory and Baseline Demographic Characteristics Ultrasound Characteristics <6 Years ‐ Since ‐ Menopause >10 Years ‐ Since ‐ Menopause (n=248) (n=348) Characteristic <6 Years ‐ Since ‐ Menopause >10 Years ‐ Since ‐ Menopause Placebo (123) Active (125) Placebo (176) Active (172) (n=248) (n=348) Variable Time since menopause, years (median, IQR) 3.5 (1.8,4.9) 3.5 (2.0,5.3) 14.1 (11.4,18.1) 14.5 (11.4,18.8) Placebo (123) Active (125) Placebo (176) Active (172) Age, years (median, IQR) 55.4 (52.5,57.8) 55.4 (53.2,57.9) 63.0 (59.9,67.0) 64.3 (60.5,68.6) Carotid artery intima ‐ media thickness, mm 0.75 (0.73,0.76) 1 0.75 (0.73,0.76) 0.79 (0.77,0.80) 0.78 (0.77,0.80) Race or ethnicity, no. (%) Body mass index, kg/m 2 (median, IQR) 26.0 (23.2,29.7) 26.2 (23.3,30.6) 26.4 (23.1,29.6) 27.2 (23.2,31.2) White, non ‐ Hispanic 73 (59.3%) 88 (70.4%) 127 (72.2%) 127 (73.8%) Black, non ‐ Hispanic 14 (11.4%) 7 (5.6%) 14 (8.0%) 17 (9.9%) Systolic blood pressure, mmHg (median, IQR) 115 (106,125) 117 (108,123) 116 (110,126) 120 (112,127) Hispanic 20 (16.3%) 16 (12.8%) 23 (13.1%) 20 (12.4%) Asian 16 (13.0%) 14 (11.2%) 12 (6.8%) 8 (4.7%) Diastolic blood pressure, mmHg (median, IQR) 77 (70,81) 75 (71,80) 73 (69,78) 74 (70,79) Education, no. (%) Less than high school 0 1 (0.8%) 2 (1.1%) 0 Serum lipids (median, IQR) High school or some college 38 (30.9%) 27 (21.6%) 71 (40.3%) 56 (32.6%) LDL cholesterol, mg/dl 134 (115,160) 139 (119,161) 133 (115,155) 131 (112,151) College graduate 85 (69.1%) 97 (77.6%) 103 (58.5%) 116 (67.4%) HDL cholesterol, mg/dl 63 (51,75) 63 (54,77) 66 (55,80) 63 (53,78) Total cholesterol, mg/dl 222 (198,247) 225 (207,245) 223 (206,243) 218 (198,242) Type of menopause, no. (%) Triglycerides, mg/dl 90 (74,129) 95 (65,119) 93 (72,129) 92 (68,133) Natural 120 (97.6%) 119 (95.2%) 144 (81.8%) 146 (84.9%) Surgical 3 (2.4%) 6 (4.8%) 32 (18.2%) 26 (15.1%) IQR = interquartile range 1 Mean (95% CI) IQR = interquartile range Hodis HN, et al. N Engl J Med 2016;374:1221 ‐ 1231. Hodis HN, et al. N Engl J Med 2016;374:1221 ‐ 1231. 4
Recommend
More recommend