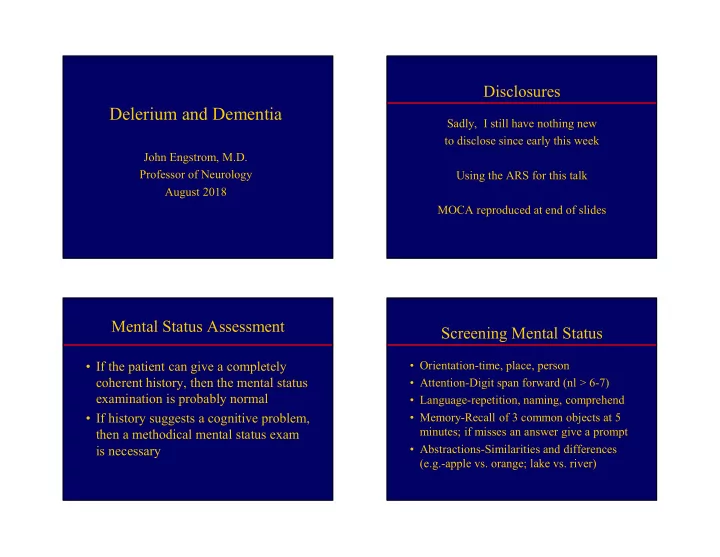
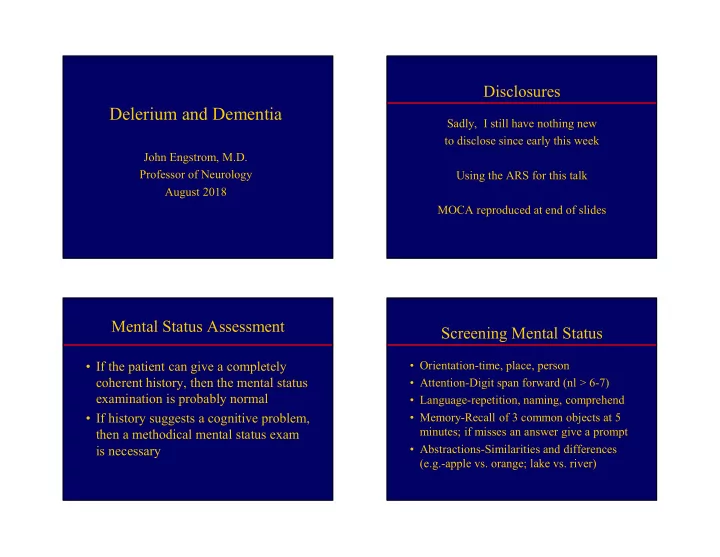
Disclosures Delerium and Dementia Sadly, I still have nothing new to disclose since early this week John Engstrom, M.D. Professor of Neurology Using the ARS for this talk August 2018 MOCA reproduced at end of slides Mental Status Assessment Screening Mental Status • If the patient can give a completely • Orientation-time, place, person coherent history, then the mental status • Attention-Digit span forward (nl > 6-7) examination is probably normal • Language-repetition, naming, comprehend • If history suggests a cognitive problem, • Memory-Recall of 3 common objects at 5 minutes; if misses an answer give a prompt then a methodical mental status exam • Abstractions-Similarities and differences is necessary (e.g.-apple vs. orange; lake vs. river) 1
Q1: Which part of an abnormal mental Screen Attention First status exam negates testing for memory? A. Abstractions • Attention-requires input of numbers, immed 33% recall, and verbal output of numbers B. Attention span 28% – Everyone must remember a numerical sequence C. Orientation 22% – Exceptions: deafness, ESL, no education 17% D. Visual fields • Memory-input of objects, hold memory of objects for five minutes , then verbal recall • Screen attention first (or after orientation) s n s n d n o o a l p i e i t i t s a f c t a n n a l o r e u t i s t i s b n O r i V A e t t A Pathological Basis of Delerium: Delerium-Defining Features Impaired Attention • Inattention-malfunction cerebrum/brainstem • Poor attention-Digit span forward < 6-7 • Arousal and attention centers in the • Subacute onset brainstem (RAS) • Other cognitive abnl (e.g.-disorientation) • Bilateral cerebral regions that receive • Not explained by another neurologic dz sensory inputs, process and interpret information, react to inputs, and result in • Evidence that the delirium is caused by a expressive or motor outputs in response “metabolic” disorder 2
Delerium-Clinical Accompaniments Delerium-Practical Clinical Features • Fluctuation over minutes-hours-lethargy or hyperactivity based on many observations • History provided by family, friends, or co- • Vital signs workers who know the patient well – Tachycardia/hypersympathetic state-infection, – Establish pre-morbid mental baseline substance use, substance withdrawal – Review medications and “substances” – New hypertension/hypotension – Review medical comorbidities – Fever-risk of infection • Initial test of choice if often to call or • Meningismus-Resistance to neck flexion interview someone who knows history • Exam features above normal in dementia Q2: Which neuro exam finding helps Neurologic exam findings that help distinguish delerium from dementia? distinguish delerium from dementia A. Fine, postural tremor • Fine postural tremor-Acute/subacute onset- often sign of hypersympathetic state B. Asterixis 73% • Asterixis-Loss of tone with wrist extension C. Myoclonus – Classic with renal or hepatic failure D. Focal neurol findings – Seen in many metabolic conditions (hemiparesis) 8% 8% 6% 4% • Myoclonus-sudden discharge of motor cells E. All of the above producing an asymmetric jerk-metabolic r s s i u . e o x . v m i n . r o e o b e l s r t c a t s g A o n e l y a d i h r M t n u f t f i o s o l o l l p A r , u e e n n F i l a c o F 3
Delerium-Metabolic Causes/Evaluation-I Delerium-Metab Causes/Evaluation-II Metabolic Causes Laboratory Studies Metabolic Causes Laboratory Studies Hypo/hypernatremia Na Substance use/withdrawal Toxicology screen Alcohol intox/withdrawal Alcohol level Renal failure BUN, Cr Medication overuse/withdrawal Review meds; consider drug level Hypoxia, ischemia PO2 Hypercalcemia, Hyper Mg Calcium, magnesium Hypo/hyperglycemia Glucose Hyperphosphatemia Phosphate Hypo/hyperthyroidism, Thyroid function tests Hepatic Failure LFTs; ammonia Delerium – Common Causes and Pitfalls in the Outpatient Evaluation Assessment of Delerium Infectious Causes Laboratory Studies • The delerium is a post-ictal state and the Sepsis Cultures, CBC, Chest X-Ray, intermittent seizures are not obvious UA – Get more history from observers re poss sz Meningitis Lumbar puncture (LP), Cultures, CBC, CXR, UA – Patient has pre-existing brain dz (e.g.-stroke) Neurologic Causes • The patient is malnourished and has Subarachnoid hemorrhage Head CT, LP thiamine deficiency (e.g.-Wernicke’s) Cerebral infarction Head CT or MRI • Neuro exam in uncooperative patient? Seizures, post-ictal state Consider head CT/MRI, EEG 4
Neuro Exam for Focality in the Delerium Neuro Exam for Focality in the (Uncooperative) Patient Delerium (Uncooperative) Patient • Cranial Nerve Examination • Motor-grade best strength; note asymmetry -Facial asymmetry on command or with grimace – Moves arms/legs symmetrically vs. gravity? -Lower 2/3 face-upper motor neuron – Able to stand with/without assistance? -Entire face-facial nerve or brainstem – Able to walk with/without assistance • Brainstem reflexes – If unable to stand/walk-due to focal weakness, – Pupils-midbrain: asymmetric, reactive? focal sensory loss, or focal leg imbalance – Corneals-pons: asymmetric, reactive? • Sensory-Symmetry of withdrawal of arms – Breathing/pulse-medulla: normal/abnormal or legs to pain stimulus of equal intensity Q3: What is Not Routinely Useful in More Pitfalls in the Outpatient Managing Improving Delerium after Assessment of Delerium Hospital Discharge • Delerium dx as depression in setting of A. Use of anti-psychotic to control somnolence or reduced responsiveness 92% behavior – Use vitals, gen exam, neurologic signs as above B. Use of prescribed eyewear – EEG nl depression, diffusely slow in delerium C. Use of prescribed hearing aids • An undiagnosed neurodegenerative disease D. Frequent reorientation of the patient in is already present (e.g.-AD) a familiar environment 4% 1% 2% 2% E. Encourage falling asleep on a – Slower recovery from delerium/post-ictal state r a . . . . . . . . e g o . . . w p n o e i n e schedule r o t y a e c e i l e t s t i h a a d t o e n h d g – Establish baseline mental function b e e n c i y r b r i l i c i o l s r a p s c e f - e i s r e t r e t n p r g p n a a f e o r f f u u o e o q o e s e e c U n s s r U U F E 5
Non-Pharmacologic Prevention Delerium-Conclusions and Management of Delerium • Especially at hospital discharge to home • If the patient can give a completely coherent history, then the mental status examination • Frequent reorientation of the patient is almost always normal • Using eyeglasses and hearing aids • Initial assessment of suspected delerium • Early PT/mobiliz-restore baseline function should include: • Sleep hygiene – Establish pre-morbid mental baseline – Prevent daytime naps – Rev medication or substance use and disuse – Encourage falling asleep on a schedule – Review medical comorbidities Delerium-Conclusions • Screen attention first • Have your list of screening labs for delerium at the ready • Beware of outpt traps-baseline depression, neurodegen dz, post-ictal state, thiamine def • Non-pharmacologic measures are proven to enhance mental functioning in delerium pts 6
Dementia Goals of Dementia Assessment • Dementia–a decline in cognition interfering with • Establish the presence/absence of dementia daily function and independence • Understand areas of cognitive impairment – No disturbance of consciousness and the severity of the impairment – Best assessed as an outpatient • Understand the functional consequences of • Impairment in at least one cognitive domain: areas of cognitive impairment/preservation – Memory and learning – Language • Determine the likely etiology – Executive function-judgment, planning, reasoning – Social cognition, perceptual-motor function Approach to Patient/Family: Visit One Q4: Which one of the following is important in a dementia history? • Best history from pt and family or sig other • General/neuro exams and limited lab testing 96% A. Recent memory function • May need separate input from others if B. Executive function patient is defensive or argumentative C. Language • Patients often lack insight into the problem D. Assessing impact of cognition on – Denial or excuses-remembering something is safety risks 4% 0% 0% 0% not important anymore or too old for an activity E. All of the above e n n . e o g . v – Social and interpersonal skills preserved early o a n . i i o t t u g c c b n n g o a n c u u e a f f f L o h y e t r v t f o i c o t a m u p l l e c m A e m x i E g t n n i e s c s e e R s s A 7
Recommend
More recommend