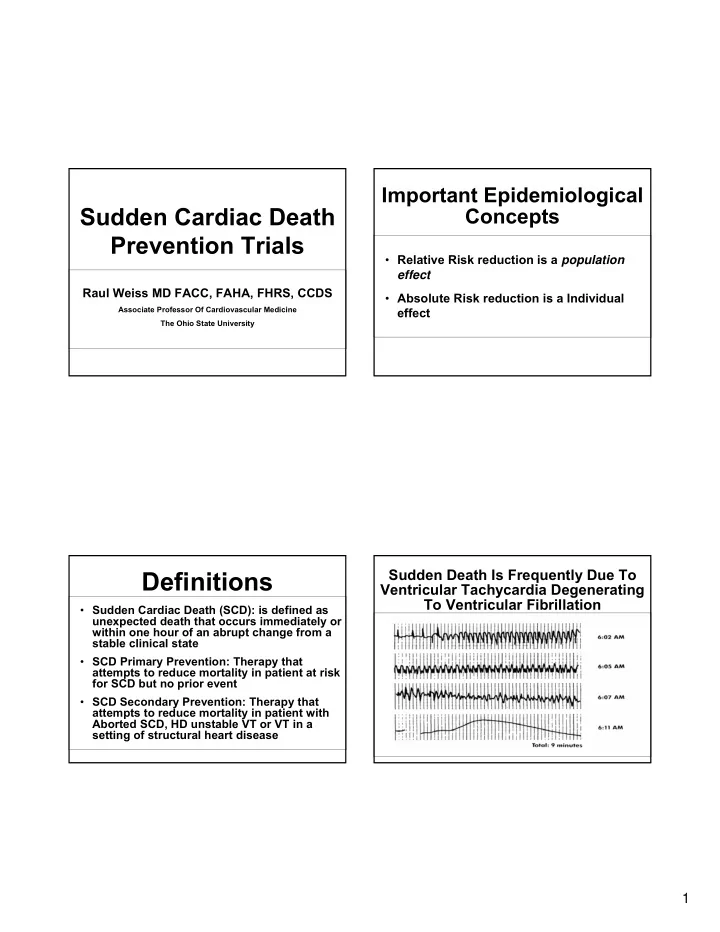
Important Epidemiological Sudden Cardiac Death Concepts Prevention Trials • Relative Risk reduction is a population effect Raul Weiss MD FACC, FAHA, FHRS, CCDS • Absolute Risk reduction is a Individual Associate Professor Of Cardiovascular Medicine effect The Ohio State University Sudden Death Is Frequently Due To Definitions Ventricular Tachycardia Degenerating To Ventricular Fibrillation • Sudden Cardiac Death (SCD): is defined as unexpected death that occurs immediately or within one hour of an abrupt change from a stable clinical state • SCD Primary Prevention: Therapy that attempts to reduce mortality in patient at risk for SCD but no prior event • SCD Secondary Prevention: Therapy that attempts to reduce mortality in patient with Aborted SCD, HD unstable VT or VT in a setting of structural heart disease 1
Incidence of SCD in Specific Populations Magnitude of the Problem and Annual SCD Numbers GROUP General population • U.S. estimates of sudden cardiac death Patients with high 300,000-350,000 derived figure from the coronary-risk profile 70s Patients with previous coronary event Patients with ejection • National center for disease statistics in fraction < 35%, congestive heart failure 2001 estimated a total of 456,000 SCD Patients with previous out-of-hospital cardiac arrest • Oregon/Seattle 2002/4 <200,000 Patients with previous MI, low EF, and VT 0 5 10 15 20 0 100,000 200,000 300,000 25 30 Incidence of Sudden Death No. of Sudden Deaths (% of group) Per Year Myerburg RJ. Circulation .1998;97:1514-1521. Magnitude of the Problem Urgency of Sudden Cardiac Arrest Resuscitation Success vs. Time Septicemia Only after the deaths from ALL cancers are combined does anything Nephritis cause more deaths each year than 100 100 100 Alzheimer’s Disease sudden cardiac arrest . Chance of success 90 90 90 Influenza/pneumonia reduced 7-10% every SCD accounts for greater than half of 80 80 80 Diabetes minute % all cardiac deaths and up to 15% of 70 70 70 Accidents/injuries Success total mortality in the United States 60 60 60 Chronic lower respiratory diseases 50 50 50 Cerebrovascular disease 40 40 40 Other cardiac causes 30 30 30 Sudden cardiac arrest (SCA) 20 20 20 All cancers 10 10 10 0 0 0 1 1 1 2 2 2 3 3 3 4 4 4 5 5 5 6 6 6 7 7 7 8 8 8 9 9 9 0% 5% 10% 15% 20% 25% Time (minutes) National Vital Statistics Report , Vol 49 (11), Oct. 12, 2001 Adapted from text: Cummins RO, 1998. Annals of Emergency Medicine. 18:1269-1275. 2
Survival After Acute MI: Who Out of Hospital Cardiac Arrest is at Risk? Site of Cardiac Arrest - The Maastricht Study 1.0 Work Other 4 20 A Public Place 0.8 31 B C On Street Survivorship 0.6 Home 47 399 D 0.4 N EF VPD ≥ 30% < 10/hr 536 A ≥ 30% ≥ 10/hr B 113 0.2 < 30% 80 < 10/hr C < 30% ≥ 10/hr D 37 Ages 20-75 only 0 1 2 3 Year Vreede-Swagemakers et al. JACC 1997;30:1500-5. Bigger JT. Am J Cardiology. 1986;57:12B. Severity of Heart Failure Time Dependence of Mortality Risk Post-MI: Prediction of Sudden Cardiac Death After Myocardial Modes of Death Infarction in the Beta-Blocking Era NYHA II CHF NYHA III � 700 post-MI patients; ~95% on beta blockers 2 12% CHF Other years after discharge. 26% Other 24% Sudden � The epidemiologic pattern 59% Death Sudden of SCD was different from 64% 15% Death that reported in previous n = 103 studies. n = 103 NYHA IV � Arrhythmia events or CHF SCDs did not concentrate early after the index Other 33% event, but most of them 56% occurred more than 18 Sudden months post-MI. Death 11% n = 27 LANCET. 1999;353:2001-07. Huikuri H, et al. J Am Coll Cardiol 2003; 42: 652-8. 3
Pharmacological CAST-I SCD Primary Prevention Trials Prognosis of Post-MI Patients Treated with Placebo vs. Encainide/Flecainide Post-MI Patients Heart Failure Patients 100 Antiarrhythmic CAST BASIS GESICA Patients without Event (%) Drugs PAT CAMIAT CHF-STAT 95 EMIAT SSSD DIAMOND-CHF Placebo DIAMOND-MI SWORD (n = 743) 90 Beta-Blockers BHAT CIBIS-II USCHFT CAPRICORN COMET MERIT Encainide or COPERNICUS Flecainide (n = 755) 85 ACE Inhibitors SAVE SOLVD P = 0.001 SMILE TRACE 80 0 91 182 273 364 455 Aldosterone RALES Receptor Blockades EPHESUS Days after Randomization Echt DS. N Engl J Med. 1991;324:781-788. CAST-I EMIAT and CAMIAT Trials Objective: Factor EMI AT 1 CAMI AT 2 � Evaluate the effectiveness of Class IC AA drugs (Encainide and Flecainide) (n = 755) compared to placebo Protocol Amiodarone Amiodarone (n = 743) in post-MI patients. vs. placebo vs. placebo Inclusion Criteria: Patient characteristics Poor LV function Frequent ventricular (LVEF < 40%) ectopic activity � MI within 6 days to 2 years, and (VEA; > 10 VPDs/hr) � LVEF > 40% if recruited > 90 days post-MI or < 55% if recruited within 90 days post-MI, and Recruitment 5-21 days post-MI 6-45 days post-MI � > 6 PVCs per hour but no VT > 15 beats or > 120 bpm, and Risk reduction of arrhythmic 35% 48.5% death at 24 months (p = 0.05) (p = 0.016) � PVCs suppressible with Encainide or Flecainide Class IC AA Drug Results: Overall mortality at 24 months No difference No difference � Caused excessive mortality compared to placebo. The study was stopped early. Echt DS. N Engl J Med. 1991;324:781-788. 1 Julian DG. Lancet. 1997;349:667-674. 2 Cairns JA. Lancet. 1997;349:675-682. 4
Pharmacological SCD Primary CHF-STAT Survival Results Prevention Trials SWORD Survival Results 1.0 1.00 .99 0.9 .98 Proportion Event-Free Proportion Surviving Placebo .97 0.8 .96 0.7 .95 .94 0.6 Amiodarone .93 0.5 .92 d -sotalol .91 0.4 .90 Placebo 0.3 .89 .88 0.2 Chi-square = 0.28 .87 Z = -2.75, p = 0.006 p = 0.60 0.1 0.0 0 60 120 180 240 300 0 6 12 18 24 30 36 42 48 54 Time from Randomization (days) Months Patients at Risk Amiodarone 336 260 175 101 33 Placebo 1,572 1,170 874 551 330 Placebo 338 263 178 95 39 d -sotalol 1,549 1,150 844 544 323 Waldo AL. Lancet. 1996;348:7-12. Singh SW. N Engl J Med . 1995;333:77-82. MERIT-HF CHF-STAT Objective and Inclusion Criteria: � Evaluate the effectiveness of Metoprolol | Objective: CR/XL (n = 1,900) compared to placebo (n = 2,001) in heart failure patients � Evaluate the effectiveness of amiodarone � NYHA II, III, or IV, and (n = 336) versus placebo (n = 338) in heart � LVEF < 40% failure patients Results: � Reduced overall mortality by 34% (7.2% vs. 11%) � NYHA Class II, III, or IV, and (p = 0.0062) � EF < 40%, and � Reduced SCD by 41% (4% vs. 6.6%) (p = 0.0002) � > 10 PVCs/hour � Reduced deaths from worsening heart failure by 49% (p = 0.0023) Singh SW. N Engl J Med . 1995;333:77-82. MERIT-HF Study Group. Lancet. 1999;333:2001-2007. 5
MERIT-HF Overall EPHESUS Mortality Results Overall Mortality Results 20 40 RR = 0.66 RR = 0.85 (95% CI, 0.75-0.96) 35 p = 0.0062 (adjusted) Cumulative Incidence (%) p = 0.008 p = 0.00009 (nominal) Placebo Cumulative Mortality (%) 30 15 25 Placebo 20 Metoprolol CR/XL Eplerenone 10 15 10 5 5 0 0 3 6 9 12 15 18 21 24 27 30 33 36 Months since Randomization 0 Patients at Risk 0 3 6 9 12 15 18 21 Placebo 3,313 3,064 2,983 2,830 2,418 1,801 1,213 709 323 99 2 0 0 Eplerenone 3,319 3,125 3,044 2,896 2,463 1,857 1,260 728 336 110 0 0 0 Follow-Up (months) MERIT-HF Study Group. Lancet. 1999;333:2001-2007. Pitt B. N Engl J Med. 2003;348:1309-1321. EPHESUS Sudden EPHESUS Cardiac Death Results Objective: 10 � Evaluate the effectiveness of Eplerenone (n = 3,313) 9 to placebo (n = 3,319) in acute MI patients with left RR = 0.79 (95% CI, 0.64- Placebo Cumulative Incidence (%) 0.97) 8 ventricular dysfunction and heart failure p = 0.03 7 � Acute MI (3-17 days), and Eplerenone 6 � LVEF < 40%, and 5 4 � Evidence of heart failure 3 Eplerenone Results: 2 1 � Reduced overall mortality by 15% (p = 0.008) 0 � Reduced SCD by 21% (p = 0.03) 0 3 6 9 12 15 18 21 24 27 30 33 36 � Reduced the risk of CV death or CV hospitalization Months since Randomization Patients at Risk by 13% (p = 0.002) Eplerenone 3,319 3,125 3,044 2,896 2,463 1,857 1,260 728 336 110 0 0 0 Placebo 3,313 3,064 2,983 2,830 2,418 1,801 1,213 709 323 99 2 0 0 Pitt B. N Engl J Med. 2003;348:1309-1321. Pitt B. N Engl J Med. 2003;348:1309-1321. 6
Recommend
More recommend