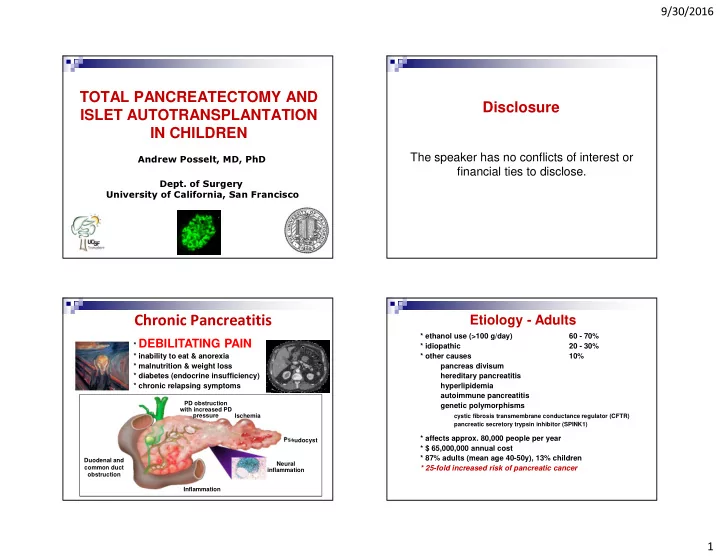
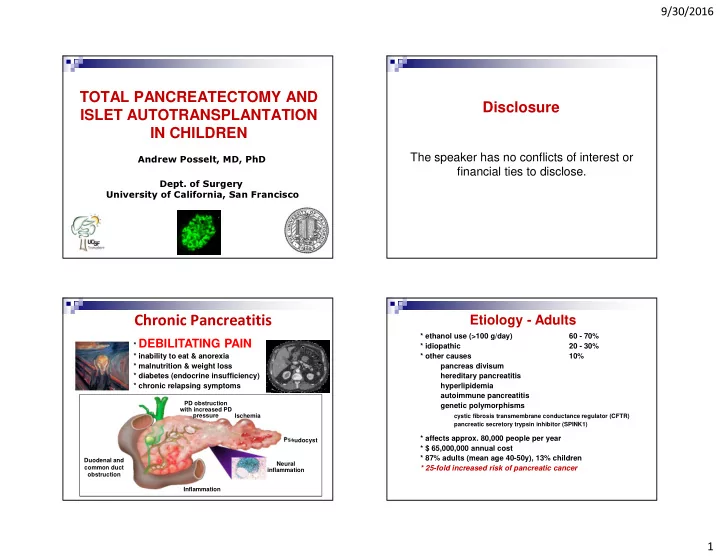
9/30/2016 TOTAL PANCREATECTOMY AND Disclosure ISLET AUTOTRANSPLANTATION IN CHILDREN The speaker has no conflicts of interest or Andrew Posselt, MD, PhD financial ties to disclose. Dept. of Surgery University of California, San Francisco Etiology - Adults Chronic Pancreatitis A * ethanol use (>100 g/day) 60 - 70% * DEBILITATING PAIN * idiopathic 20 - 30% * inability to eat & anorexia * other causes 10% * malnutrition & weight loss pancreas divisum * diabetes (endocrine insufficiency) hereditary pancreatitis * chronic relapsing symptoms hyperlipidemia autoimmune pancreatitis PD obstruction genetic polymorphisms with increased PD pressure Ischemia cystic fibrosis transmembrane conductance regulator (CFTR) pancreatic secretory trypsin inhibitor (SPINK1) * affects approx. 80,000 people per year Pseudocyst * $ 65,000,000 annual cost * 87% adults (mean age 40-50y), 13% children Duodenal and Neural * 25-fold increased risk of pancreatic cancer common duct inflammation obstruction Inflammation 1
9/30/2016 Etiology - Children Treatment Options • Narcotic pain meds, enzyme replacement • Endoscopic therapies 67% - sphincterotomy, stents, dilations • Celiac plexus ablation 33% • Surgical decompression (Puestow, Frey, Beger) or partial resection (Whipple, distal) - NOT effective in most pts • Total Pancreatectomy - Very effective in most pts, but results in brittle diabetes * Mean age: 14 y (35% 5-12 y, 65% 13-19 y) * 44% male, 56% female • Islet Autotransplant restores endocrine * 7-8 y Abdominal pain function after TP (TP/IAT) * 5-6 y Dx of CP * 1-2 y Narcotic use Schwarzenberg, et al., JPeds 2015 TP-IAT at UMN Patient Selection � Painful chronic pancreatitis or disabling acute relapsing pancreatitis refractory to medical/endoscopic therapy � Narcotic dependence and/or significantly impaired quality of life � Imaging/EUS evidence of CP (MRI, MRCP, CT, ERCP) OR 409 pts total 53 children (5-18y) relapsing acute pancreatitis (>3 episodes over 6 mos) OR hereditary pancreatitis w/ Sx � Non-diabetic OR C-peptide positive diabetes � Patient and family accept (and can manage) risk of diabetes and need for lifelong pancreatic enzyme replacement Contraindications: • Active alcohol use (documented abstinence for >6mos) 1.2% in-hospital mortality; 89% (adult) and 98% (child) 5-y survival � • Illegal drug use 90% C-peptide pos., 33% partial function � • Pancreatic cancer (maybe not IPMN) 30% insulin independent at 3 y (25% adults, 55% children) � Pain improved in 85% adults, 94% children (67% pain-free) • Advanced liver, lung, heart disease � 15.9% had complications requiring reoperation (bleeding, anastomotic leaks) • Relative – absent C-peptide � Sutherland, et al., JACS 2012 2
9/30/2016 TP/IAT Cases by State: 1977- 2013 Pediatric TP/IAT Cases by State: 1977- 2016 27: 5-12 yrs WA: 0 48: 13-19 yrs ME MT ND 2 0 4 OR MN VT VT:0 VT:0 1 409 N NY H ID SD NH:0 NH:0 WI M 10 MI MI 7 MN A 2 16 WY MA:3 MA:3 16 17 75 1 RI:1 RI:1 IA PA: 13 NV CT:0 CT:0 CA NE 5 N OH 30 1 M J 1 PA IL IN 132 D D NJ:8 NJ:8 UT 15 15 E 10 0 CO W CA DE:0 DE:0 OH 5 9-18 yrs KS MO 1 8 V VA: 8 14 KY: 3 MD:3 6 8 DC: 0 4-16 yrs NC: 4 14-18 yrs TN: 9 AZ O NM 3 SC: AR 61 K 1 2 33 AL MS Number of Patients GA GA 91 1 4 4 TX TX LA 15+ 15 13 3 11-15 AK 0 FL 6-10 11 1-5 0 0 HI Timing Pros and Cons of TP/IAT in Pediatric CP PROS: Resolution of chronic refractory pain � Earlier is better! • • Improved QOL � Prior to development of central sensitization and opioid-induced • Elimination of pancreatic cancer risk hyperalgesia which can lead to pain recurrence CONS: � Prior to development of diabetes, malignancy • High cost • Prolonged hospital stay � Optimization of islet yield/function • Irreversible operation � Prior to invasive surgical procedures (partial resection, ductal drainage) • Life-long dependence on exogenous enzymes � Early in course of disease to minimize fibrosis • Diabetes and potential need for chronic insulin therapy Absence of counter-regulatory hormones • GI side effects (dysmotility, malabsorption, diarrhea, • malnutrition, etc) 3
9/30/2016 Multi-Disciplinary Team Is A MUST! The Procedure Gastroenterology Nursing ICU Team Endocrinology Patient Pain Management Psychiatry Islet Manufacture Surgery Patient’s OWN islets Social Work No risk of rejection No immunosuppression Durability of Pain Control Durability of Islet Function Genetic/Hereditary Nonhereditary Insulin Requirements HbA1c ** Pancreatitis pain Pain severity VERY FEW pts developed diabetes-related complications Chinnakotla, et al., JACS 2014 Wilson, et al., Ann Surg 2014 4
9/30/2016 TP-IAT Particularly Effective in QOL by SF-36 Assessment - Children Children with CP SF-36 Narcotic Use Insulin Independence Ped Adult Adult Ped Chinnakotla, et al., Ann Surg 2015 Bellin, et al., UMN data School Attendance and Days of Islet Function and Insulin Independence Impaired Activity � 25-40% insulin independent in most large cohorts � Most insulin dependent patients have graft function � Low insulin needs P<0.005 � + C-peptide (nearly 90%) P<0.001 � Benefit of islets, even if on insulin � Stable glycemic control � Avoid “brittle” (labile) diabetes � Absent hypoglycemic episodes Sutherland et al., Transplantation 2008 Sutherland et al., Transplantation 2008 Ahmad et al., JACS 2005 Ahmad et al., JACS 2005 Bellin, et al., UMN data Webb et al., Pancreas 2008 Webb et al., Pancreas 2008 5
9/30/2016 Who Becomes Insulin Independent? Insulin Independence and IEQ/Kg � Predictors: � Islet number (mass/yield) 80% � 100% function, 70% independent with >5000 IE/kg 70% � 83% function, 30% independent with 2501-5000 IE/kg 60% � 59% function, 15% independent with <2500 IE/ kg <2500 � Prior surgery 50% 2500-5000 � Lower yield after surgical drainage/distal pancreatectomy 40% >5000 � Age 30% Allo � Younger patients have higher rates of insulin independence 20% � Other characteristics 10% � duration of disease, islet quality, insulin resistance 0% 6 months 12 months 24 months 36 months Sutherland et al., Transplantation 2008 Sutherland et al., Transplantation 2008 Ahmad et al., JACS 2005 Ahmad et al., JACS 2005 Webb et al., Pancreas 2008 Webb et al., Pancreas 2008 High Likelihood of Insulin Islet Yield and Prior Pancreatic Surgery Independence in Young Children 14000 3795 3647 4000 12000 10000 3500 IE/kg 8000 6000 2654 3000 IEQ/Kg 4000 2000 2500 1973 1883 0 0.0 5.0 10.0 15.0 20.0 2000 Age at Transplant (years) 1500 Insulin Dependent Minimal Insulin Insulin Independent 1000 � Children 5-18 years of age: Baseline Whipple Beger/Frey Distal Puestow � 44% ever achieve insulin independence Sutherland et al., Transplantation 2008 � 85% of children <10 years of age have Ahmad et al., JACS 2005 documented insulin independence Bellin, et al., UMN data Webb et al., Pancreas 2008 6
9/30/2016 UCSF Inpatient Care Algorithm Islet Neogenesis in Children with CP Day 4-5 Day 1 PCA transition to short acting elixir PCA Oral pain meds Start TF/enzymes IV Anti-emetics TF at goal Interconnected duct-like (arrows) Bowel Regimen NG out/GT to gravity, NPO and endocrine structures (arrowheads) Start Lantus, D/C insulin drip Insulin drip surrounded by fibrosis Start Diabetic education Ambulate to chair Consult Endocrine, Pain Svcs Day 6 ADAT Day 2 Start TF education/Discharge class Normal Pancreas PCA CP Pancreas Bowel Regimen TF/enzymes Continue plan, eval for complications IV Anti-emetics Insulin drip Day 7-8 Ambulate x1 Supplement education prn Order PT/OT Eval & Treat Insulin Continue plan, eval for complications Cytokeratins Day 3 Consider transfer to Home/Rehab when following are met: PCA transition basal to long-acting Nuclei TF stable TF/enzymes Adequate water intake to prevent IV depletion/dehydration IV Anti-emetics Diabetes stable, not requiring daily titration of Diabetes Insulin drip Ambulate x3 therapy No surgical concerns Islets separate from ductal issue Narcotic dose stable, < 3 extra IV doses/day Insulin pos. cells surrounded by duct-like structures Soltani,et al Acta Diab 2013 Pediatric TP/IAT at UCSF UCSF Experience • 2004 - 2015: 28 cases 8 Children (2013-2016) • 22 cases since 2014 (50% male, 8 children) Pt DOS Etx Age Weight IEQ IEQ/kg Current Insulin • mean age 38 years (range 4 to 72) 1 3/7/13 CFTR/SPINK 10 32 kg 264,234 8,257 full (has T1DM) • 10 islet isolations for other centers 2 2/10/14 PRSS1 12 41 kg 185,840 4,425 5-10U/d 3 5/7/15 P. Divisum 16 50 kg 432,200 7,582 0 • Etiologies of CP: 4 9/8/15 SPINK 4 17 kg 186,600 10,724 0 5 4/4/16 PRSS1 7 24 kg 207,660 8,652 0 idiopathic/familial 60% 6 5/24/16 PRSS1 10 41 kg 331,420 8,163 0 pancreas divisum 10% 7 5/26/16 CF/SPINK 14 69kg 688,822 9,983 weaning (5mos) 8 8/1/16 CF 16 124kg 187,400 1,551 weaning (2mos) remote alcohol abuse 30% MEAN+SD 11.4 + 4.3 310,547+ 7,412+ biliary disease 0% 176,104 3,028 • Prior pancreatic surgery 4/8 pain-free off narcotics • Puestow procedure 33% 2/8 weaning (intermittent narcotics only) • distal pancreatectomy 25% 2/8 managed in LA (at least 1 weaning) • pancreaticoduodenectomy 8% 7
Recommend
More recommend