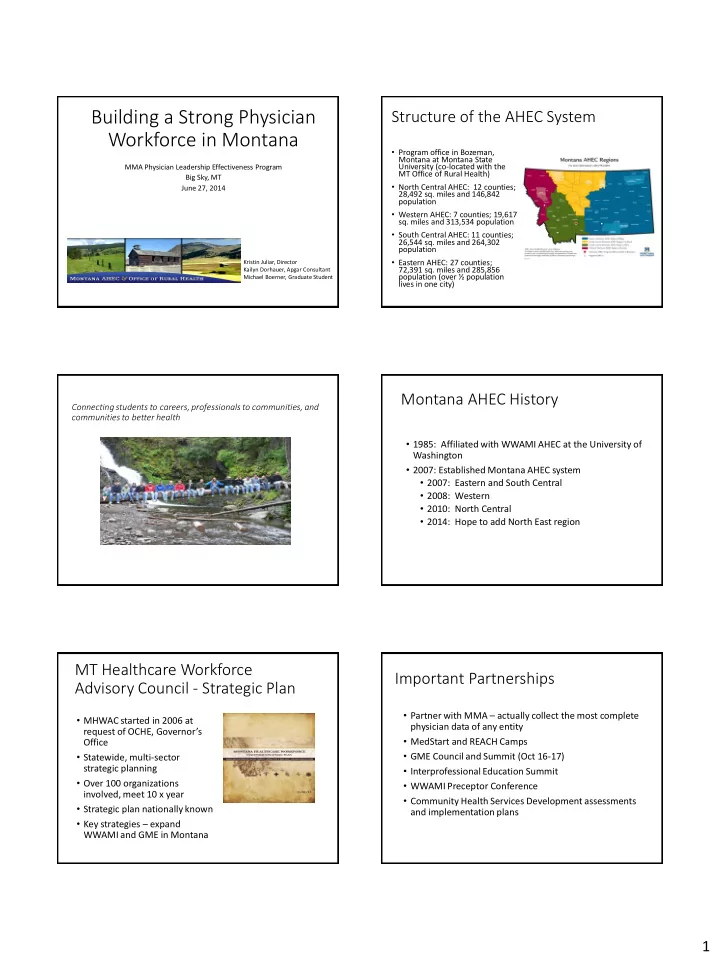
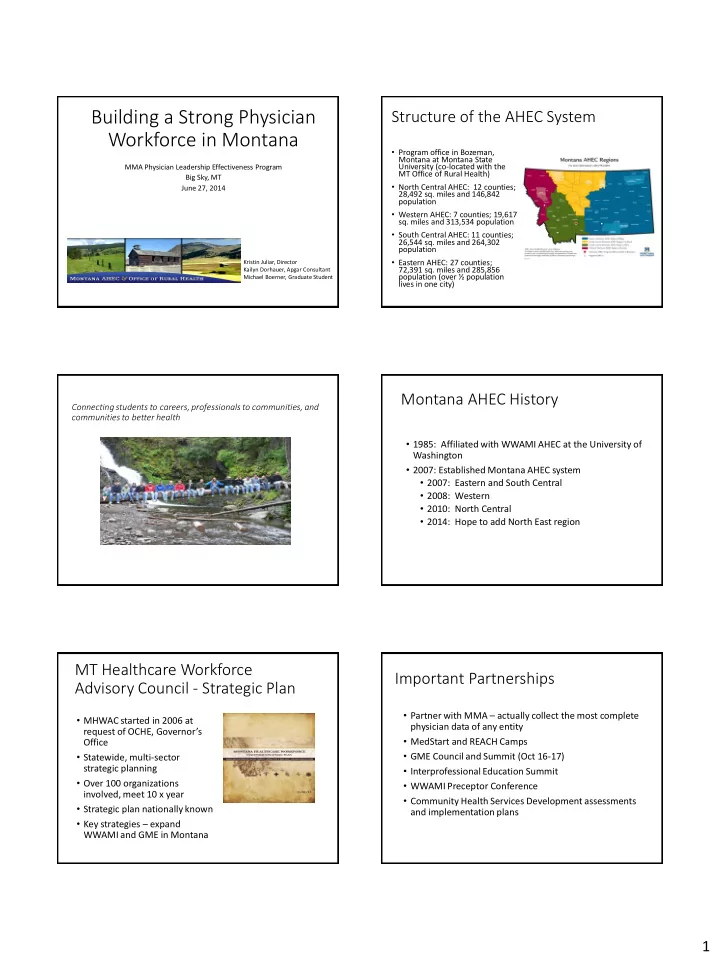
Building a Strong Physician Structure of the AHEC System Workforce in Montana • Program office in Bozeman, Montana at Montana State MMA Physician Leadership Effectiveness Program University (co-located with the MT Office of Rural Health) Big Sky, MT • North Central AHEC: 12 counties; June 27, 2014 28,492 sq. miles and 146,842 population • Western AHEC: 7 counties; 19,617 sq. miles and 313,534 population • South Central AHEC: 11 counties; 26,544 sq. miles and 264,302 population • Eastern AHEC: 27 counties; Kristin Juliar, Director 72,391 sq. miles and 285,856 Kailyn Dorhauer, Apgar Consultant population (over ½ population Michael Boerner, Graduate Student lives in one city) Montana AHEC History Connecting students to careers, professionals to communities, and communities to better health • 1985: Affiliated with WWAMI AHEC at the University of Washington • 2007: Established Montana AHEC system • 2007: Eastern and South Central • 2008: Western • 2010: North Central • 2014: Hope to add North East region MT Healthcare Workforce Important Partnerships Advisory Council - Strategic Plan • Partner with MMA – actually collect the most complete • MHWAC started in 2006 at physician data of any entity request of OCHE, Governor’s • MedStart and REACH Camps Office • GME Council and Summit (Oct 16-17) • Statewide, multi-sector strategic planning • Interprofessional Education Summit • Over 100 organizations • WWAMI Preceptor Conference involved, meet 10 x year • Community Health Services Development assessments • Strategic plan nationally known and implementation plans • Key strategies – expand WWAMI and GME in Montana 1
Nourish and Grow Relationships Workforce Strategic Plan State Government Higher Education • Plan has been reviewed and • Department of Public Health Commissioners’ Office and Human Services, Primary Universities accomplishments Care Office Two-Year Colleges documented. Currently • Commissioner of Securities Tribal Colleges and Insurance - PCMH working to update in 2014. • SWIB/DOLI — Research and Healthcare Reform Analysis Bureau, Licensure • However , based on MHWAC CMMI Projects--Innovation • Office of Public Instruction Frontier Community Health input, the most important (K-12) Integration Project CMS issue that remains to be Associations/Networks addressed is lack of Providers Hospital consistent data collection Professions University – Tribal College and data analysis . CHCs Partnerships Extension Public Health Montana Office of Rural Health • The other half of our office • Works on healthcare infrastructure needs in rural Montana • Conducts assessments with critical access hospitals through a project with MHA and the Montana Frontier Medicine Better Health Project – Community Health Services Development Program • CHSD looks at both health issues and health service needs in critical access hospital communities Community Health Services Implementation Plans Development (CHSD) • Assessing community health needs for over 20 years • MORH has drafted 23 plans for Montana CAHs since January 2013 • Coordinate with hospital’s board and employees • Random sample mail-out surveys • Plans list needs prioritized from CHSD Report • Focus groups • Key-informant interviews • Defines strategies to address specific priorities • CHSD Report – what does our survey/focus group data tell us? • Implementation plans – What are we going to do about • Explains why some priorities may be out of reach it? 2
Commonly Prioritized Needs Top Health Concerns 100% Specialists, Services Needed 100% Avoiding or Delaying Care Due… 95% Interest in Health Education… 83% Primary Care Needed 69% Avoiding or Delaying Care Due… 69% Lack of Financial Options… 52% 0% 20% 40% 60% 80% 100% Addressing Mental Health Needs • 100% of CAHs prioritizing a need to improve mental health services have specified strategies to address it • List mental health resources available in the community • Defer cost of emergent mental health treatment • Involvement with U of M Rural Mental Health Practitioner Program • Creating partnerships with local resources • Advertising counseling services • Addressing alcohol abuse • Improving telepsychiatry Rural Montana's Top Specialist Priorities 0% 20% 40% 60% Dermatology Eye-Care ENT Dental Mental Health 57% 100% of IPs Dermatology 35% prioritize needs for specialists Ophthalmology/Optometry 26% or specialty services 17% Addressing 9% Addressing 17% Addressing 4% Addressing ENT 26% 17% Not Addressing 17% Not Addressing 9% Not Addressing 22% Not Addressing Dental 26% 3
Av Avoiding or De Delaying g Care Hospit itals Addr ddres essin ing Patie ients ts Av Avoid oidin ing or Dela layi ying Care Common Priorities for Montana CAHs Due to Cost Due to Availability Top Health Concerns (Obesity, • Due to Cost – 95% 100% Cancer, Diabetes, etc…) Specialists, Services Needed 100% Avoid/Delay Care Due to Cost 95% Interest in Health Education 83% Classes • Due to Availability – 70% Primary Care Needed 69% Avoiding or Delaying Care Due to 69% 43% Addressing 43% Addressing Wait/Scheduling/Access Lack of Financial Options 52% Not Addressing 26% Not Addressing 52% Awareness 0% 20% 40% 60% 80% 100% Acknowledgements The Community Apgar Project • David Schmitz, MD Associate Director of Rural Family Medicine Family Medicine Residency of Idaho • Ed Baker, PhD Director, Center for Health Policy A Validated Tool for Improving Rural Boise State University Communities’ Recruitment and Retention of Physicians • Funding North Central Montana Area Health Education Center The Community Apgar Questionnaire Purpose of Community Apgar (CAQ) Research Questions aggregated into five classes: • Development and validation of a tool which identifies 1. Geographic and weighs factors important to communities in 2. Economic recruiting and retaining rural family physicians 3. Scope of Practice • Differentially diagnose modifiable factors for strategic 4. Medical Support planning in individual critical access hospitals 5. Hospital and Community Support • Presentation of individual CAQ Scores facilitating • Each class contains ten factors for a total of fifty discussions with key decision makes in each community factors/questions for specific strategic planning and improvements • Three open-ended questions 4
CAQ Class/Factor Examples Process: Year 1 • Geographic Class • Kailyn Dorhauer and Shani Rich travel to 20 CAH • Schools, climate, perception of community, spousal satisfaction communities during summer 2014 • Economic Class • CEO and lead physician interviewed separately and • Loan repayment, income guarantee, revenue flow, competition asked to rate each factor as an advantage (major or minor) or challenge (major or minor) to the • Scope of Practice Class community • Obstetrics, C-sections, ER, endoscopy, nursing home • Each factor also rated by importance (very important, • Medical Support Class important, unimportant, very unimportant) • Nursing workforce, EMS, call coverage, perception of quality • Data is analyzed with peer database • Hospital and Community Support Class • Physical plant and equipment, internet, hospital leadership, EMR Data Analysis Process: Year 1 • Boise State University: values assigned to responses for all factors and analyzed data • Kailyn Dorhauer and Shani Rich present to hospital leadership and Board of Directors • Community Apgar Score • Constructed from the sum of weighed parameters in • Discussion of community data and comparisons with the five classes of the CAQ explanation of differences from peers • Similar to the five dimensions of the neonatal Apgar a • Strategic planning session for improvement of repeatable measure of a community’s assets and capabilities weaknesses and marketing of strengths Advantage/Challenge Importance Major Advantage +2 Very important +4 Minor Advantage +1 Important +3 Minor Challenge -1 Unimportant +2 Major Challenge -2 Very unimportant +1 Process: Year 2 The CAQ Value Proposition • Kailyn and Shani conduct second site evaluation and 2 • Beyond “Expert Opinion” interviews • Hospital CEO and Lead Physician • A new approach to the old problem of • Data is analyzed with peer databases and prior year scores physician recruiting • Present a second time to hospital leadership and Board of • Self-empowering for the community: Directors knowledge as power, not an outside • Discussion of community data and comparisons with explanation of differences from peers and prior year scores “headhunter” • Strategic planning session for improvement of weaknesses • Beyond physician recruitment to community and marketing of strengths improvement • Discussion of effectiveness of strategic plan implementation and the CAQ Program 5
CAH X: Comparative Cumulative Apgar CAH X: Comparative Cumulative Apgar Score Score for Geographic Class CAH X: Comparative Cumulative Apgar Top 10 Advantages- CAH Score for Medical Support Top 10 Challenges- CAH Top 10 Importance- CAH 6
For more information Kristin Juliar, Director 406-994-6003; kjuliar@montana.edu Kailyn Dorhauer 406-994-7709 kailyn.dorhauer@montana.edu Michael Boerner MichaelBoerner@montana.edu 7
Recommend
More recommend