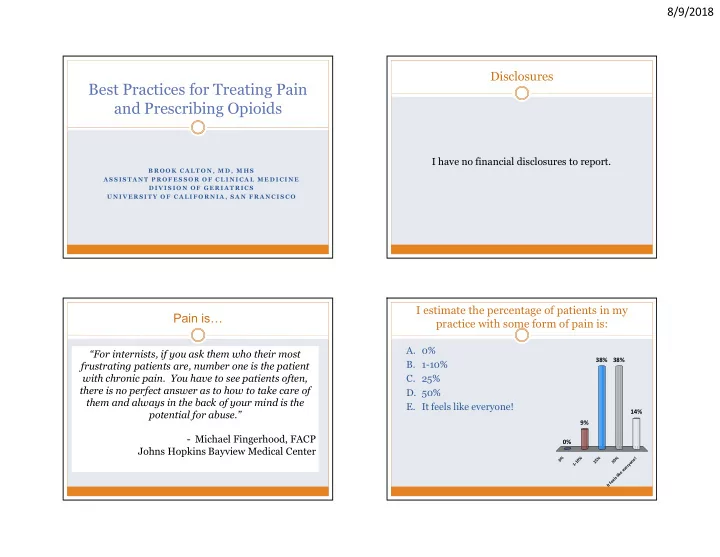
8/9/2018 Disclosures Best Practices for Treating Pain and Prescribing Opioids I have no financial disclosures to report. B R O O K C A L T O N , M D , M H S A S S I S T A N T P R O F E S S O R O F C L I N I C A L M E D I C I N E D I V I S I O N O F G E R I A T R I C S U N I V E R S I TY O F C A L I F O R N I A , S A N F R A N C I S C O I estimate the percentage of patients in my Pain is… practice with some form of pain is: A. 0% “For internists, if you ask them who their most Always a subjective experience 38% 38% B. 1-10% frustrating patients are, number one is the patient As an unpleasant sensation it becomes an with chronic pain. You have to see patients often, C. 25% emotional experience there is no perfect answer as to how to take care of D. 50% A significant stress physically and emotionally them and always in the back of your mind is the E. It feels like everyone! Common - an estimated 11% of Americans potential for abuse.” 14% experience daily pain 9% - Michael Fingerhood, FACP Potentially very frustrating/challenging for medical 0% Johns Hopkins Bayview Medical Center providers 0% 1-10% 25% It feels like everyone! 50% 1
8/9/2018 For me, the hardest thing about managing Managing pain is really hard patients with pain is: A. Patient complexity Highly prevalent B. Managing opioids safely The ultimate bio-psycho-social problem 39% C. Concerns re: federal regulation and Regulatory complexity liability Therapeutic options inadequate D. Lack of community resources 19% 18% 17% Some interventions may exacerbate chronic pain E. Lack of education and training on 8% Patient experience of pain is real pain management But so are addiction, disengagement, diversion y PCPs under-trained & under-resourced y . t l . . i e . . . . x f u . . e g u r a t l s e o p s d m s r e d n a l r o i a o r y c e n p i t t d n i o n o e u t i e f a i g m t n : c a e u i r m P g d a s o e n n c r f a e f o M o c n k k c o c a C a L L Outline Assessing Pain “OPQRST” Assessment of Pain O: Onset Designing a Treatment Plan P: Palliative or precipitating factors Q: Quality of pain Treatment of Nociceptive vs Neuropathic Pain R: Region or radiation of pain Opioid Dosing and Side Effects S: Severity Safe Opioid Prescribing Principles T: Temporal nature Observational signs of distress Quantify the pain 2
8/9/2018 Focus on Function! Designing a Treatment Plan Effect on function > quantitative rating Consider… ADLs, IADLs The Bio-Psycho-Social Model Hobbies, socialization, exercise Concentration, appetite, sleep Co-morbid conditions Mood, energy, relationships Overall health Is the pain… “PEG” Scale: On a scale of 0-10, over the last week: Acute or chronic? What has your average pain been? (0-10) Serious illness-related or not? How much has your pain interfered with your enjoyment of life? (0-10) Nociceptive or neuropathic? How much has your pain interfered with your general activity ? (0-10) The Bio-Psych0-Social Model The Bio-Psych0-Social Model Medications Medical Cannabis (?) Surgery Interventional strategies Dz related mechanisms Exercise, Sleep Bio Bio Biologic mechanisms of Acupuncture psychiatric illness PT/OT Palliative radiation (for CA) Psychotherapy Mindfulness Environmental Relaxation Distress Psycho Social Psycho Social Social support stressors techniques Anger Limiting other Close personal Fear stressors relationships Gatchel, Am Psychol, 2004; Gatchel, Psychol Bull, 2007 Gatchel, Am Psychol, 2004; Gatchel, Psychol Bull, 2007 3
8/9/2018 Co-Morbid Conditions Acute vs. Chronic Pain Months to Years (>3 mos or past Days to weeks time of normal healing) PHQ-9 GAD Single item screeners Neuropathic Pain Nociceptive Pain Caused by stimuli NSAID Risks Damage to or pathology within the nervous system, threaten/provoke tissue damage Examples: MSK conditions, GI bleeding – ulceration, platelet can be central or peripheral. inhibition inflammation, visceral tumor Examples: Diabetes, postherpetic neuralgia, and stroke Renal failure – worse if volume depleted, Always consider non-pharm and hyperCa, kidney, heart, or liver disease Establish diagnosis targeted treatment adjuvants AKA alleviate the compression, remove the offending agent Acetaminophen: <3 gm/day, <2 CHF – 2 to 10-fold risk of hospitalization First line medications: Gabapentin, TCAs, SNRIs, gm/day liver dz; avoid combos Cardiac – ibuprofen > naproxen risk Topical Lidocaine NSAIDS: Good for inflammation and bony-related pain Hypertension – 3/2 point increase • For more severe pain, could consider opioids Feenstra J. Arch Intern Med 2002;162:265 Page J. Arch Intern Med 2000;160:777 CNT Collaboration. Lancet. 2013;382(9894):769 4
8/9/2018 A Few Important Details Opioid Selection Drug PO IV Choose Route 1. Morphine 30 mg 10 mg Choose Medication 2. Hydrocodone 30 mg -- Oxycodone 20 mg -- Choose Dose 3. Hydromorphone 7.5 mg 1.5 mg 4. Choose Frequency Fentanyl See chart 0.1 mg (100 mcg) Patient/Family Ed 5. Route Peak analgesic Dosing 6. Rx Bowel Regimen (Senna to start) effect frequency Monitor and Adjust 7. Oral 60-90 min Q1-4h IV 6-15 min Q15-30min SQ 30 min Q15-30min “Easier to Stay Out of Pain, Than Get Out of Pain!” Opioid Side Effects PRN Dosing ATC Dosing Side effect Time to Tolerance Constipation Never Nausea/vomiting 7-10 days Pruritus 7-10 days Sedation 36-72 hrs Respiratory depression Extremely rare when opioids are dosed appropriately 5
8/9/2018 Opioid Prescribing Over Time Pre-1995: parsimonious with Rx opioids in US 1995-2009: Oxycontin, 5 th VS, patient advocacy groups Opioid Prescribing Over Time Pre-1995: Parsimonious with opioids in US 1995-2009: Oxycontin, 5 th VS, pt advocacy groups 2010-now: 20% of patients with non-cancer pain symptoms or diagnoses receive an opioid rx Opioid rx per capita increased 7% from 2007 to 2012; rates increasing more for FP, IM >420K ER visits related to misuse/abuse in 2011 Great variability across states Dose limits, Payor/Pharm restrictions 6
8/9/2018 (CNCP) Linked to methadone 7
8/9/2018 In the community in which I practice, abuse of Safe Opioid Prescribing Strategies opioid pain medications is: Before prescribing: Not a problem at all A. Weigh the potential benefits/risks 49% A small problem Assess for opioid misuse/abuse B. Set clear expectations! A moderate problem 36% C. A big problem D. When prescribing: 13% Consider key prescribing principles Monitor for effect 2% Review reasons to discontinue l m m m l a e e e t b l l l a b b o o o m r r r p p p e l l e g b l a t i o m a b r p r A s e d a A o t Dowell D. JAMA 2016; 19;315(15):1624-45 o m N A Weigh the Potential Benefits/Risks Potential Benefits Opioids can help provide short-term relief of CNCP There is a role for opioids in management of compared to placebo acute pain and pain during terminal illness. No studies of opioid therapy vs placebo, no opioid For CNCP, opioids could be considered when: therapy, or non-opioid therapy evaluated long-term outcomes (>1 year) like pain, function, or quality of Other alternative therapies have not provided life. sufficient pain relief and Pain is adversely affecting a patient's function and/or quality of life and The potential benefits of opioid therapy outweigh potential harms Furlan. CMAJ 2006; 23;174(11):1589-94. Chapparo LE. Cochrane Database Syst Rev 2013; (8):CD004959 Chou. Annals of Int Med 2015; 162(4):276-86 8
8/9/2018 Assessment of Opioid Misuse and Abuse Potential Risks Constipation Falls and fractures 1,2 Misuse : Using meds different than rx’ed Less likely to return to work Sedation 1,2 Abuse : Using meds to alter consciousness Immune dysfunction 2 Opioid overdose 2 Addiction : Neurobiological disease, 4C’s Decreased GNRH, low Death from overdose 1,2 libido 2 (compulsion, craving, consequences, control) Aberrant use, addiction 2 Hyperalgesia 2 Population Abuse/addiction rate Misuse rate Difficult interactions with ED visits 2 the care providers 2 All pt CNCP 3.27% 11.5% Depression 2 Without past/current 0.19% 0.59% SUD dx Psychosocial problems 2 1 Mixing with other sedating drugs associated with increased risk 2 Higher doses associated with increased risk Fishbain DA. Pain Med 2008; 9(4):444-59 Opioid Misuse/Abuse Risk Assessment Opioid Misuse/Abuse Risk Assessment No standardized approach Single Item Screeners Consider high risk factors • NIDA: “How many times in the past year have you used an illegal drug or used a prescription medication for non-medical History of substance use disorder 2, 4 reasons?” Younger Age 1, 2, 3, 4, 5, 6 Male gender 2, 4 • Formal opioid misuse/abuse risk assessment tools Caucasian/White 1 may add to your assessment Mental Health Disorders 1, 3, 4, 5, 6, 7 Large dose or supply 3, 4, 8 Drug Cravings 7 relation to pain severity 2 1. Dowling et al, 2006. 2. Ives et al, 2006. 3. Edlund et al, 2010. 4. White et al, 2009. 5. Fleming et al, 2007. 6. Reid et al, 2002. 7. Wassan et al, 2007. 8. Dunn et al, 2010. 9
Recommend
More recommend