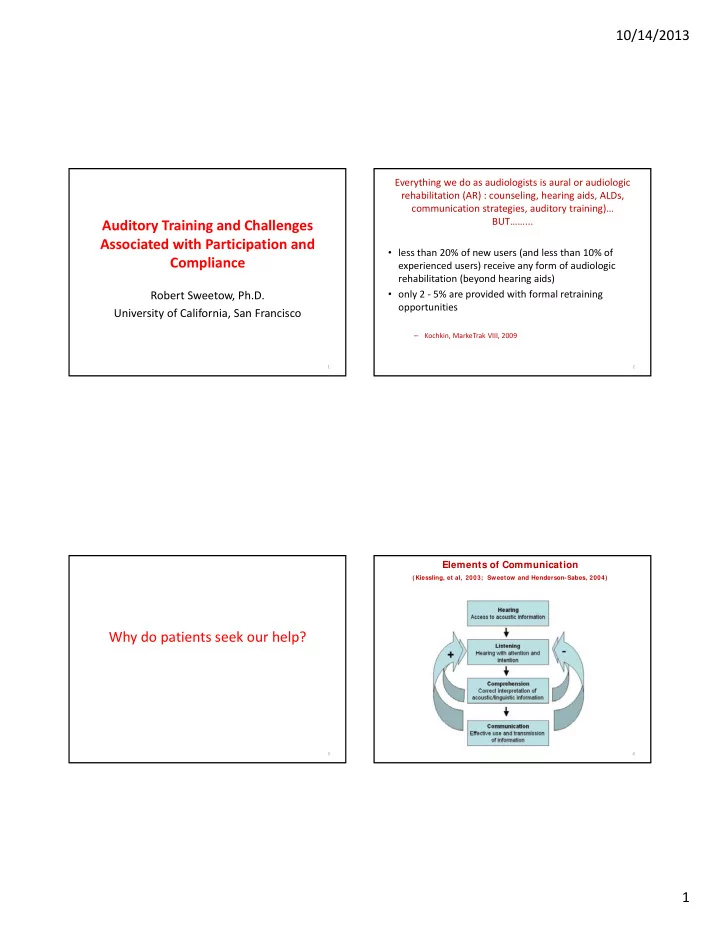
10/14/2013 Everything we do as audiologists is aural or audiologic rehabilitation (AR) : counseling, hearing aids, ALDs, communication strategies, auditory training)… BUT……... Auditory Training and Challenges Associated with Participation and • less than 20% of new users (and less than 10% of Compliance experienced users) receive any form of audiologic rehabilitation (beyond hearing aids) Robert Sweetow, Ph.D. • only 2 ‐ 5% are provided with formal retraining opportunities University of California, San Francisco – Kochkin, MarkeTrak VIII, 2009 1 2 Elements of Communication (Kiessling, et al, 2003; Sweetow and Henderson-Sabes, 2004) Why do patients seek our help? 3 4 1
10/14/2013 The biggest mistake we currently make Potential impediments to achieving mastery of these elements may be……. • Making hearing aids the focus of our • Hearing loss attention, when the focus should • Neural plasticity and progressive be…. neurodegeneration • Enhancing communication • Global cognitive decline • Maladaptive compensatory behaviors • Loss of confidence 5 6 Current speech perception tests…. • Don’t take the contextual nature of Are we really testing conversation into account communication? • Don’t take the interactive nature of conversation into account • Don’t allow access to conversational repair strategies that occur in real life Flynn, 2003 7 8 2
10/14/2013 Communication Needs Assessment Relevant domains for assessment Measures beyond the audiogram that can be used to define residual auditory function. Objective procedures • Communication expectations and needs • QuickSIN • Sentence recognition in noise – BKB ‐ SIN • Tolerance of noise • Hearing in Noise Test (HINT) • Ability to handle rapid speech • Listening in Spatialized Noise Sentences (LiSN ‐ S) • Binaural integration (interference) • Acceptable Noise Levels (ANL) • Cognitive skills (working memory, speed of processing, • Binaural interference executive function) • Dichotic testing • Auditory scene analysis • Listening span (Letter Number Sequencing) • Perceived handicap • TEN • Rapid (compressed) speech test • Confidence / self ‐ efficacy • Speechreading • Dexterity • Dual ‐ tasking • Vision • Need for screening measures 9 10 Communication Needs Assessment Measures beyond the audiogram that can be used to define residual auditory function. Communication Confidence Profile Subjective measures Please circle the number that corresponds most closely with • Hearing Handicap Inventory for the Elderly – Screening HHIE ‐ S your response for each answer. • Communication Scale for Older Adults (CSOA) • Communication Confidence Profile (CCP) or Listening Self If you wear hearing aids, please answer the way that you Efficacy Questionnaire hear WITH your hearing aids. • Self Assessment and Communication partner subjective scales (SAC and SOAC) Combined (objective and subjective) methods Sweetow, R and Sabes J. Hearing Journal: (2010); 63:12 ;17 ‐ 18,20,22,24. • Performance Perceptual Test (PPT) 11 12 3
10/14/2013 1. Are you confident you can understand conversations when you are 7. Are you confident that you can focus on a conversation when other talking with one or two people in your own home? distractions are present? 2. Are you confident in your ability to understand when you are 8. Are you confident that you can understand a person speaking in large conversing with friends in a noisy environment, like a restaurant? 3. In order to hear better, how likely are you to do things like moving rooms like an auditorium or house of worship? closer to the person speaking to you, changing positions, moving to a 9. In a quiet room, are you secure in your ability to understand people quieter area, finding better lighting, etc? with whom you are not familiar? 4. If you are having trouble understanding, how likely are you to ask a person you are speaking with to alter his or her speech by slowing 10. In a noisy environment, are you confident in your ability to down, repeating, or rephrasing? understand people speaking with whom you are not familiar? 5. How sure are you that you are able to tell where sounds are coming from (for example, if more than one person is talking, can you identify 11. Are you confident that you can switch your attention back and forth the location of the person speaking?) between different talkers or sounds? 6. Are you confident that you are able to follow quickly ‐ paced 12. If you are having difficulty understanding a person talking, how likely conversational material? 13 are you to continue to stay engaged in the conversation? 14 CCP interpretation Some facts related to aging • 2/3 of people age 70 and older have hearing loss • Older adults with hearing loss have a 24% higher risk of cognitive impairment • 50+ = Confident • A 25 dB hearing loss equals the reduction in • 40 ‐ 50 = Cautiously certain cognitive performance associated with a 6.8 year age difference • 30 ‐ 39 = Tentative • Could be related to common cause hypothesis (shared neural pathways) , extra resource • Below 29 = Insecure expenditure; isolation from hearing loss Lin (2011, 2013) 15 16 4
10/14/2013 • Imaging studies of word identification in unfavorable signal ‐ to ‐ noise ratios have revealed greater activation of memory and attention brain regions in older adults compared with younger adults ( Neuropsychologia • Older adults with hearing loss and poor 2009;47[3]:693 ‐ 703 ). To compensate for reduced audibility or deficits in temporal processing ( J Neurosci working memory are more susceptible to 2012;32[41]:14156 ‐ 14164 ; J Acoust Soc Am hearing aid distortions from signal ‐ processing 2006;119[4]:2455 ‐ 2466 ), older adults appear to draw more on cognitive resources than younger adults do algorithms, suggesting that cognitive skills ( Ear Hear 2010;31[4]:471 ‐ 479 ). should be taken into account in the hearing • Despite this greater need to rely on cognitive aid fitting. resources, older adults often have a diminished cognitive reserve when trying to communicate in a complex listening environment ( Trends Amplif 2006;10[1]:29 ‐ 59 ). – Arehart, et al; Ear Hear 2013;34[3]:251 ‐ 260 ) 17 18 Montreal Cognitive Assessment So what’s the point? • designed to assist in the detection of mild • Like other diagnostic testing, any single cognitive impairment ( J Am Ger Soc measure (including speech in noise testing) 2005;53[4]:695 ‐ 699 ). may not provide enough additional information to justify the time or cost. • http://www.mocatest.org • However consideration of a combination of objective and subjective measures beyond the audiogram can supply important rehabilitation data. 19 20 5
10/14/2013 Pilot study – what can busy clinical audiologists fit in? • UCSF Request – Minimum of 2 objective and 2 subjective measures Is this practical????? – Keep track of time – Keep track of how additional data impacted therapy plan • Results – 80% received CCP and HHIE/A ‐ S – 70% performed Quick SIN – 10% performed ANL, PPT ‐ DIS, etc. 21 22 However……… Why????? 70% provided usable information • a) not enough time • b) inconvenient above and beyond the “comp • c) don’t believe additional data will help audio” • d) all of the above • e) don’t feel it is important to follow the instructions of the boss 23 24 6
10/14/2013 Assessing Motivation and Readiness Expectations vs. Goals for AR • Expectations have a product orientation • Source : internal vs. external – Patient assumes passive role • Level: – Whatever goes wrong is the professional’s fault handicap perception • Goals have a rehabilitation orientation • desire to rehabilitate – Patient assumes active role – Patient shares in the process • Don’t fit an unmotivated patient 26 25 Ida Institute tools • Circle of change • Line • Decisional Balance Box ……. and don’t forget assessment!!!!!!!!!!!! (Prochaska and DiClemente, 1984) 27 28 7
10/14/2013 Benefit does NOT equal satisfaction! Outcome assessment should relate • Cox (1997) estimated that satisfaction is explicitly to the needs and goals comprised of: determined. • 40% benefit (both psychosocial and acoustic); • 25% personal image; • 19% service and cost; Gatehouse 2003; Cox et al 2000 • and 16% negative features. 29 30 Client Oriented Scale of Improvement How will your patient (and you) assess outcome? COSI • Hearing soft sounds • Louder perception • Self ‐ report questionnaire requiring patient to • Understanding speech in noise list 5 listening situations in which help with • Listening effort (elevators don’t make travel from hearing is required. Post ‐ rehab, the reduction floor 1 to floor 20 more effective, but they do make it in disability and the resulting ability to easier) !!!!! (Irv Hafter) communicate in these situations is quantified. • End of day fatigue • Takes less than 5 minutes of patient time, 2 • Use of new strategies minutes professional time for interpretation • Quality of life • Benefit or satisfaction • RFC 31 32 8
Recommend
More recommend