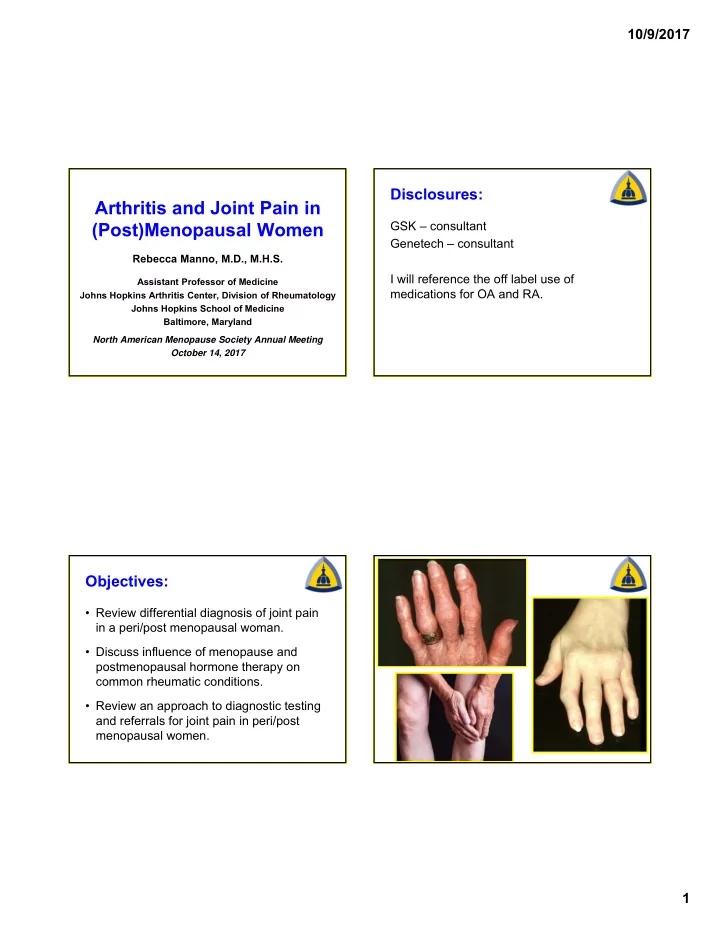
10/9/2017 Disclosures: Arthritis and Joint Pain in (Post)Menopausal Women GSK – consultant Genetech – consultant Rebecca Manno, M.D., M.H.S. I will reference the off label use of Assistant Professor of Medicine medications for OA and RA. Johns Hopkins Arthritis Center, Division of Rheumatology Johns Hopkins School of Medicine Baltimore, Maryland North American Menopause Society Annual Meeting October 14, 2017 Objectives: • Review differential diagnosis of joint pain in a peri/post menopausal woman. • Discuss influence of menopause and postmenopausal hormone therapy on common rheumatic conditions. • Review an approach to diagnostic testing and referrals for joint pain in peri/post menopausal women. 1
10/9/2017 56yo ♀ from Baltimore… • ~ 12 months ago new onset joint symptoms • Different from ‘usual’ aches and pains On any given day in a • Started in her feet, difficult to walk to bathroom in am • Worsening stiffness in hands rheumatology clinic... • Also pain in knees, elbows, and back • She feels achy and stiff. Meds : HCTZ, Naprosyn 220mg daily prn 56yo ♀ from Baltimore… 56yo ♀ from Baltimore… PMHX: Hyperlipidemia, HTN Differential Diagnosis: Last menstrual period age 51. • Osteoarthritis (OA) FamHX: Granddaughter SLE • Crystalline arthritis (gout) SocHX: Lives with husband, 2 kids, 2 dogs. Quit • Systemic autoimmune disease smoking at age 30, occasional whiskey in the evening (and Bailey’s in her coffee). Works as a paralegal in law firm. 2
10/9/2017 Osteoarthritis • ≥ 20 million in the USA • Present in at least 44% Osteoarthritis and postmenopausal ♀ (WHI) • 3x more common among ♀ Estrogen age 45-64 compared to ♂ • Second leading cause of disability in USA • 400,000 TKR and 600,000 THR per year Wright NC, et al. J AM Geriatr Soc 2008;56(9):1736 Srikanth VK, et al. Osteoarthritis Cartilage 2005;13:769 Talsania M, et al. Rheum Dis Clin N Am 2017;43:287 Lawrence R, et al. Arthritis Rheum 1998;41:778 Age-Related Prevalence of OA: ESTROGEN Changes on X-Ray Men Women 80 80 DIP Prevalence of OA (%) Prevalence of OA (%) DIP 60 60 Knee 40 40 Knee 20 20 Hip Hip 0 0 20 40 60 80 20 40 60 80 Age (years) Age (years) Martin ‐ Millan, M et al. Joint Bone Spine 2013;80:368 3
10/9/2017 Osteoarthritis & Estrogen: Human Data Martin ‐ Millan, M et al. Joint Bone Spine 2013;80:368 • Genetic variations in ER genes associated with knee OA in ♀ 1 • WHI: 27% decrease THR; 13% decrease TKR in estrogen-treated group 2 • Nurses’ Health Study: High BMI and age associated with THR; no association with current/past estrogen supplementation 3 1 Riancho JA, et al. Osteoarthritis Cartilage 2010;18:927 2 Cirillo DJ, et al. Arthritis Rheum 2006;54:3194 3 Karlson EW, et al. Am J Med 2003;114:93 56yo ♀ from Baltimore… Talsania M et al. Rheum Dis Clin N Am 2017;287 4
10/9/2017 OA: Symptoms & Signs Distribution of primary OA • Primary OA typically • OA Pain is generally • Joint instability related to use involves variable number of • Bony enlargement joints in characteristic • Pain gets worse during • Restricted movement locations, as shown the day • Crepitus • Minimal morning • Exceptions may occur, but stiffness (<20 min) and • Variable swelling should trigger consideration after inactivity (gelling) and/or instability of secondary causes of OA • Range of motion decreases Causes of secondary OA Beware…night pain… • Dysplastic Differential Diagnosis: • Post inflammatory –chondrodysplasias –epiphyseal dysplasias –infection • Extra articular (bursitis/tendinitis) –congenital hip dislocation –RA/inflammatory arthritis –developmental disorders • Fracture –Legg-Perthes • Endocrine, Metabolic –Leg-length inequality • R/O Malignancy –acromegaly –ochronosis • Posttraumatic • Severe OA –hemochromatosis –acute –crystal • (e.g., fracture through joint) –hyperparathyroidism –repetitive • (e.g., occupational injury) –postoperative • (e.g., meniscectomy) 5
10/9/2017 Is the pain OA? 56yo ♀ from Baltimore… Differential Diagnosis: • “Hip” pain • Knee Pain – Trochanteric bursitis – Patellofemoral syndrome • Osteoarthritis (OA) – PMR – Chondromalacia patella – Iliotibial band syndrome – referred hip – AVN – pes anserine bursitis • Crystalline arthritis (gout) – meralgia paresthetica – AVN – psoas/piriformis syndromes – FM tender points • Systemic autoimmune disease – neuropathic Gout • Overall prevalence ~4% in USA • 5.9% prevalence ♂ • 2% prevalence ♀ Women and Gout • Major risk factors: hyperuricemia, age , BMI (obesity) Zhu Y, et al. Arthritis Rheum 2011;63(10):3136 6
10/9/2017 Gout & Women • Obesity in early-mid adulthood is associated with 2.8 fold increased risk gout among ♀ 1 • Age, not menopause status, was associated with gout 2 • Use of opposed estrogens decreased risk incident gout (OR 0.69, 95% CI 0.56-0.86) ♀ >45yo (w/o renal failure) 3 1 Maynard J, et al. Am J Medicine 2012;125:717 2 Krishnan E, et al. Menopause 2014;21(11):1211 3 Bruderer SG, et al. Menopause 2015;22(12):1335 56yo ♀ from Baltimore… Differential Diagnosis: • Osteoarthritis (OA) • Crystalline arthritis (gout) • Systemic autoimmune disease 7
10/9/2017 Almost all autoimmune/rheumatic Almost all autoimmune/rheumatic diseases are more common in women: diseases are more common in women: ↓ Estrogen & DHEA • SLE/Lupus (SELENA; HRT-SELENA) • Sjogren’s syndrome • Giant cell arteritis/polymyalgia ↓ IFN-gamma ↑ IL1,IL6, TNF α rheumatic • Rheumatoid arthritis RA: Epidemiology RA: Who cares? • If untreated, 20-30% of RA pts become permanently • Prevalence ~ 1% of the general population unable to work within 3 years of diagnosis • Lifetime cost approaches that of cardiovascular • Peak incidence between 35 - 60 years of age diseases • Associated with an increased mortality risk • Incidence 2-4x greater in women than in men (infection risk with disease activity) • Early diagnosis and appropriate therapy reduces joint damage and comorbidities 8
10/9/2017 Early Menopause(<46yo) Premature Mortality in Patients with RA Premature Mortality in Patients with RA 1.0 1.0 Control Women Control Women 0.9 0.9 Control Men Control Men 0.8 0.8 Survival Probability Survival Probability RA Women RA Women 0.7 0.7 RA Men RA Men 0.6 0.6 0.5 0.5 0.4 0.4 0.3 0.3 Major Cause of Excess N = 886 N = 886 0.2 0.2 Deaths is SMR = 3.08 SMR = 3.08 Cardiovascular Disease 0.1 0.1 0.0 0.0 0 5 5 10 10 15 15 20 20 25 25 Years After Entry Into Study Years After Entry Into Study SMR = standardized mortality ratio for patients with RA compared with non-RA controls. SMR = standardized mortality ratio for patients with RA compared with non-RA controls. Wolfe F, et al. Arthritis Rheum . 1994;37:481-494. Wolfe F, et al. Arthritis Rheum . 1994;37:481-494. Pfeifer EC, et al. J Rheum 2014;41(7):1270 The Clinical Spectrum of RA No DIP, CMC, 1 st MTP Early PIP swelling Active with Late-stage some deformity deformities 9
10/9/2017 RA: Clinical Features Joint Involvement in Early RA • SYMPTOMS: – Joint swelling – Joint pain – Joint redness and warmth – SIGNIFICANT Morning Stiffness (>30min) • SIGNS – ARTHRITIS: symmetric, polyarticular (>3 joints) • Symmetry may not be present at disease onset! – MCP/PIP/Wrist/MTP Involvement – “Row” Pattern – Cervical spine – Sparing of T/L spine RA: Laboratory Characteristics RA: Catch the Warning Signs Refer to a rheumatologist if a patient shows any of these symptoms: • ≥ 3 swollen joints (do not have to be symmetric!) • Positive “squeeze” test • Morning stiffness ≥ 30 minutes • Persistence of symptoms > 6 weeks • Positive Anti-CCP/ACPA Squeeze test indicates pain across second to fifth metacarpals (MCP), metatarsals (MTP) 10
Recommend
More recommend