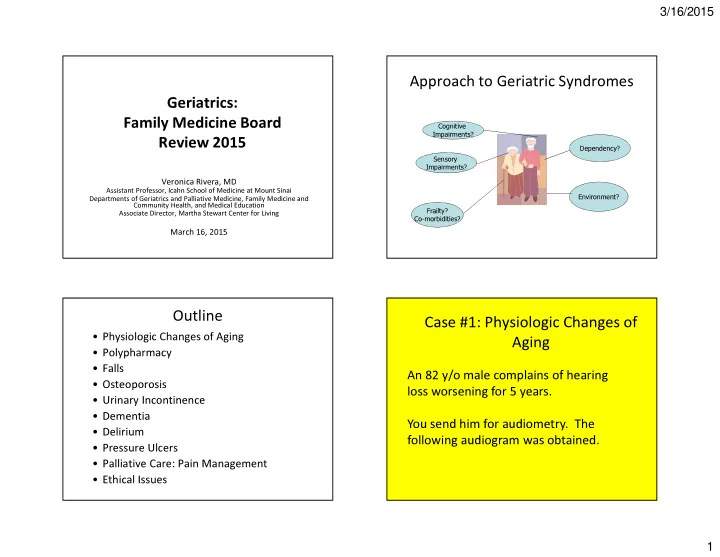
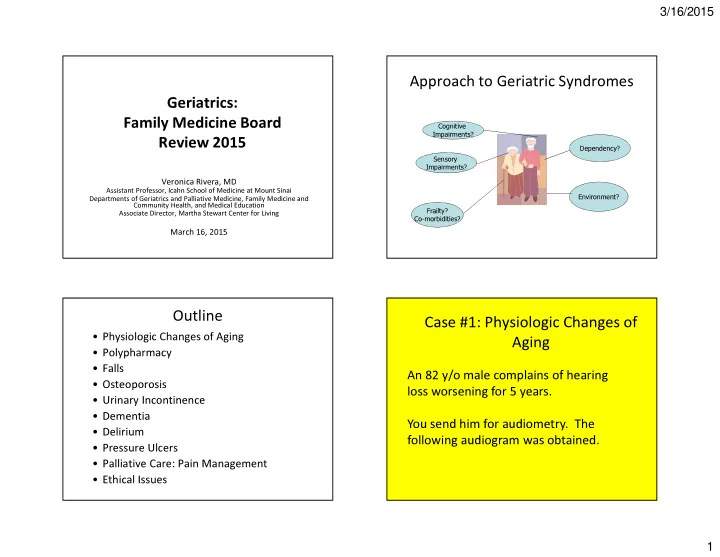
3/16/2015 Approach to Geriatric Syndromes Geriatrics: Family Medicine Board Cognitive Impairments? Review 2015 Dependency? Sensory Impairments? Veronica Rivera, MD Assistant Professor, Icahn School of Medicine at Mount Sinai Environment? Departments of Geriatrics and Palliative Medicine, Family Medicine and Community Health, and Medical Education Frailty? Associate Director, Martha Stewart Center for Living Co-morbidities? March 16, 2015 Outline Case #1: Physiologic Changes of • Physiologic Changes of Aging Aging • Polypharmacy • Falls An 82 y/o male complains of hearing • Osteoporosis loss worsening for 5 years. • Urinary Incontinence • Dementia You send him for audiometry. The • Delirium following audiogram was obtained. • Pressure Ulcers • Palliative Care: Pain Management • Ethical Issues 1
3/16/2015 Sensorineural Hearing Loss • Presbycusis – Age Related hearing loss – Symmetric, high frequency, gradual onset – Difficulty understanding speech in noisy places • Menière's Disease – Low frequency, sensorineural loss fluctuates and progresses. – Episodes of vertigo, aural fullness, tinnitus – Rx: avoidance of triggers; diuretics when diet fails • Excessive noise exposure • Acoustic neuroma (asymmetric) What kind of hearing loss is depicted? • Ototoxic drugs Conductive Hearing Loss Conductive Hearing Loss Obstruction of external •Cerumen auditory canal •Foreign body •Debris for otitis externa Impairment of tympanic •Perforated tympanic membrane function membrane Air/bone gap on •Tympanosclerosis audiogram Middle ear conditions •Otits media with effusion •Otosclerosis •Cholesteatoma Hearing Loss in Older Adults, AAFP. 2012. 2
3/16/2015 Physiologic Changes in Aging: Physiologic Changes in Aging: Sensory Changes • Hearing: • Cardiovascular – Presbycusis (bilateral, high frequency, – Myocardial/vascular stiffness sensorineural) – Increase wax buildup – Decrease heart rate and cardiac output – Stiffening of ossicles and drum – Conduction abnormalities • Decreased taste buds, oral secretions, smell • Pulmonary • Vision: – Decrease vital capacity – Difficulty with glare & dark adaptation – Decreased accommodation – Increase Residual Volume – Decreased acuity – Decreased tear production Physiologic Changes in Aging: Physiologic Changes in Aging: • Skin • Skeletal System – Thins – Decrease in Bone Density – Loss of hair follicles, sweat glands, and melanocytes – Loss of muscle mass – Atrophy of subcutaneous fat – Decrease tendon and ligament elasticity – Loss of elasticity • Renal • Other – Decrease blood flow and GFR – Decreased immunity (Primarily cell mediated) – Decrease ability to concentrate urine – Decreased physiologic reserve and homeostasis – Recovery takes longer 3
3/16/2015 Physiologic Changes in Aging: • Sleep – Decreased sleep efficiency – Decreased total sleep time – Less and earlier REM sleep – Less deep (stage 3 and 4) sleep; more Stage 1 and 2 – More napping, night time awakening, early morning awakening Case #2: Polypharmacy Case #2: Polypharmacy An 80 y.o. woman with CHF, Afib, depression and DM2 presents with several months of intermittent nausea and anorexia • Denies other GI symptoms or recent illnesses, and without vomiting. She takes has not been taking other medications. – digoxin 0.25 mg daily – warfarin sodium 5 mg daily • Other than a 10 lb weight loss (110lbs to 100lbs), her – furosemide 40 mg daily vital signs and exam are normal except for a heart – lisinopril 20 mg daily rate of 55. – glipizide 6 mg daily • Serum creatinine is 1.2 mg/dl (unchange in past 10 – citalopram 20 mg daily years), electrolytes normal, hemoglobin A1C is 7.2%, – occasional acetaminophen. INR is 3.0, and hemoglobin 12.5 g/dl. She has been on these doses for 5 years. 4
3/16/2015 Drugs - Physiologic Changes in Case #2: Polypharmacy Aging: • Absorption : unchanged What physiologic changes best explain her symptoms? • Volume of Distribution : • Water soluble drugs -> more concentrated ( digoxin ) – Decrease body mass � smaller volume of Age related changes in body composition distribution and renal function • Fat soluble drugs -> longer half life (Benzodiazepenes) – Increase in body fat � larger volume of distribution • Metabolism/elimination : • Liver: glucuronidation generally not affected, may have reductions in cytochrome p450 • Renal function may be affected Age related changes in body Drugs - Practical Considerations: composition and physiology DECREASES INCREASES • Pharmacodynamics : • Total Body Mass • Total Body Fat – Older adults may have increased sensitivity to • Liver Mass medications at standard doses: • Creatinine Clearance •Increased sedation with some benzodiazepines •Increased sensitivity to opiates •Urinary retention / delirium with anti- cholinergic drugs (diphenhydramine, tricyclics) • Psychosocial dynamics : adherence may be limited by cognition, dependency, lack of resources 5
3/16/2015 Beers List: Drugs to Avoid (except if…) Drugs - Practical Considerations: Organ System or Rationale Recommend Quality of Strength of TC or Drug Evidence Recommend. Nitrofurantoin Pulmonary tox Avoid long Moderate Strong Alternatives term • Polypharmacy : The risk of drug interactions increases linearly Lack of efficacy suppression; with number of drugs prescribed <60 mL/min avoid if CrCl – 43% of men and 57% of women use 5 or more <60 mL/min prescription/Over the Counter drugs/week Antipsychotics Increase CVA and Avoid unless Moderate Strong – Institutionalized patients are prescribed an average 5-8 (conventional or CV mortality in danger to atypical) dementia self/others and drugs non pharm has – 10-17% of geriatric admissions are for adverse drug events failed – 2002 AMA CSA report Insulin, sliding Hypoglycemia Avoid Moderate Strong scale risk Chlorpropamide Hypoglycemia Avoid High Strong Glyburide risk Beers List: Drugs to Avoid (except if…) Beers List: Drugs to Avoid (except if…) Organ System or Rationale Recommend. Quality Strength of Organ System or Rationale Recommend. Quality of Strength of TC or Drug of Recommend TC or Drug Evidence Recommend. Evidence . Benzodiazepines Risk cognitive Avoid for High Strong Non Risk cognitive Avoid chronic Moderate Strong Short and long effects and injury treatment of Benzodiazepines effects and injury use, >90 days Hypnotics (fall/MVA); same acting (fall/MVA); rare insomnia, use appropriate agitation, or ADE as benzo’s eg benzo delirium withdrawal Estrogens with or Carcinogenic Avoid oral and High Strong Megestrol Minimal effect on Avoid Moderate Strong w/o progestin potential, lack of topical patch. weight; risk of efficacy in Topical cream thrombotic events dementia/CV dz safe and and death prevention effective for vaginal symptoms Metclopramide EPS and TD Avoid, unless Moderate Strong gastroparesis Muscle Relaxants Ineffective at Avoid Moderate Strong tolerated doses, Non-COX NSAIDs, GI bleeding; Avoid chronic Moderate Strong antichol, falls oral Protection w/ PPIs use 6
3/16/2015 Drugs – Pearls for the Boards: Case #3: Falls resulting in a Colles ’ fracture. She has had two other • Ms T is an 80 year old woman who lives alone. She • Don ’ t automatically “ treat ” a new symptom with a new drug • Always put drug effect or drug interaction in the differential just came in to your office for follow up of a fall diagnosis for an elderly patient falls over the past year and a half. She is scared of • Often the answer requires dose adjustment or drug falling again. discontinuation • Older patients with a normal creatinine may have modestly • She has a history of osteoarthritis and impaired renal function anxiety/depressison. • She is on naproxen sodium 500mg BID, sertraline 50mg daily and ativan 1mg BID as needed Epidemiology of Falls Case #3: Falls • 30- 40% of community-dwelling people over Which is the best way to prevent the age of 65 years fall each year future FALLS in this patient? • Increases to about 50% for those 80 years and older • Half are repeat fallers • Over half of those in nursing homes and hospitals will fall each year Tinetti, ME. N Engl J Med 2003 Rubenstein LZ Clin Ger Med 2002 Chang JT et al BMJ 2004 7
Recommend
More recommend