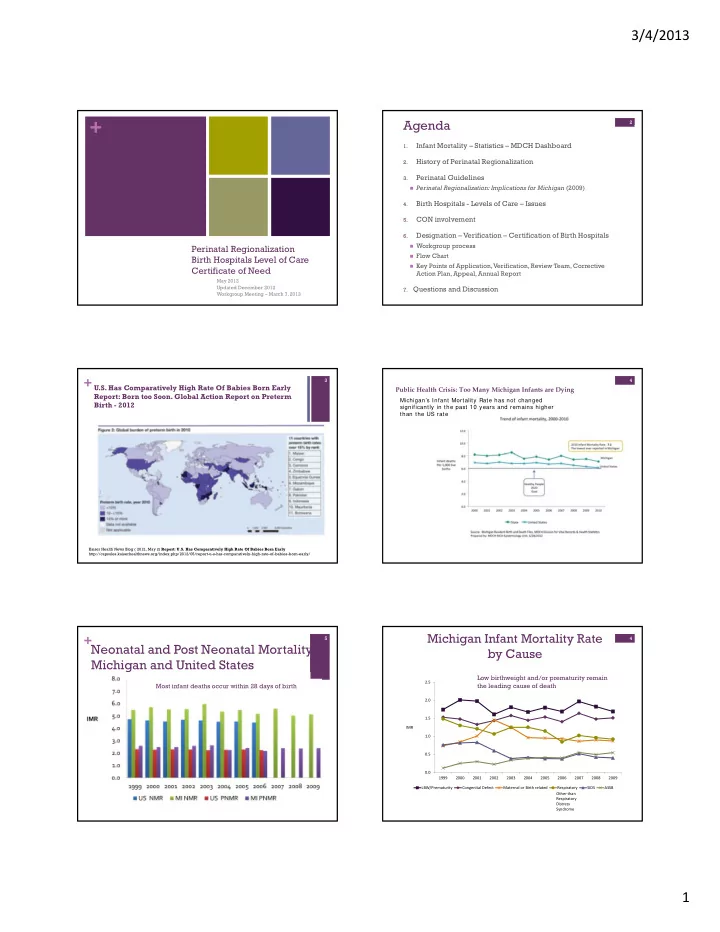
3/4/2013 + Agenda 2 2 Infant Mortality – Statistics – MDCH Dashboard 1. History of Perinatal Regionalization 2. Perinatal Guidelines 3. Perinatal Regionalization: Implications for Michigan (2009) Birth Hospitals - Levels of Care – Issues 4. CON involvement 5. Designation – Verification – Certification of Birth Hospitals 6. Workgroup process Perinatal Regionalization Flow Chart Birth Hospitals Level of Care Key Points of Application, Verification, Review Team, Corrective Certificate of Need Action Plan, Appeal, Annual Report May 2012 Updated December 2012 7. Questions and Discussion Workgroup Meeting – March 7, 2013 + U.S. Has Comparatively High Rate Of Babies Born Early 3 4 Public Health Crisis: Too Many Michigan Infants are Dying Report: Born too Soon. Global Action Report on Preterm Michigan’s Infant Mortality Rate has not changed Birth - 2012 significantly in the past 10 years and remains higher than the US rate Kaiser Health News Blog ( 2012, May 2) Report: U.S. Has Comparatively High Rate Of Babies Born Early http://capsules.kaiserhealthnews.org/index.php/2012/05/report-u-s-has-comparatively-high-rate-of-babies-born-early/ Michigan Infant Mortality Rate + Neonatal and Post Neonatal Mortality 5 4 by Cause Michigan and United States Low birthweight and/or prematurity remain 2.5 Most infant deaths occur within 28 days of birth the leading cause of death 2.0 1.5 IMR 1.0 0.5 0.0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 LBW/Prematurity Congenital Defect Maternal or Birth related Respiratory SIDS ASSB Other than Respiratory Distress Syndrome 6 1
3/4/2013 + Govenor Synyder Dashboard 7 8 Distribution of infant mortality by cause, MI 2010 Low birth weight and/or prematurity remain the leading cause of death Accidents 8.1% Respiratory 6.1% LBW/Prematurity 24.2% Other 23.1% Congenital Defect 22.5% Related to SIDS 5.4% Maternal or Birth Complications 10.5% Source: Michigan Resident Birth and Death Files, MDCH Division for Vital Records & Health Statistics Prepared by: MDCH MCH Epidemiology Unit, 6/28/2012 9 10 Infant Mortality Reduction Plan Infant Mortality Reduction Campaign August 1, 2012 Targeted evidence based strategies to reduce and prevent infant mortality: Implement Regional Perinatal System 1. Promote statewide adoption of policies to eliminate medically 2. unnecessary deliveries before 39 weeks gestation Promote adoption of progesterone protocol for high risk women 3. Promote safer infant sleeping practices to prevent accidental 4. suffocation Expand home-visiting programs to support vulnerable women and 5. infants Support better health status of women and girls 6. Reduce unintended pregnancies 7. Weave the social determinants of health into all targeted strategies to 8. promote reduction of racial and ethnic disparities in infant mortality http://www.michigan.gov/documents/mdch/MichiganIMReductionPlan_UPDATED_395151_7.pdf 11 12 11 Historical Perspective of Literature Review and National Experts Regionalization in Michigan 12 Indicate that states with a regionalized and coordinated perinatal system of care better assure that pregnant women and Development of effective newborn intensive care in the late babies are more likely to deliver in an appropriate hospital 1960s and 1970s setting and receive appropriate services to meet their needs . 1976: NCPH recommended a regionalized system for perinatal care (“Toward improving the Outcomes of Pregnancy”): focused to inpatient care Implemented further by most state health departments He althy Pe o ple 2020 Authority for health department to designate levels of care CH-33 Increase the proportion of very low birth weight (VLBW) MI was contained in Administrative Rules promulgated on infants born at level III hospitals or subspecialty perinatal centers 2/21/76 The MI State Medical Society developed its own guidelines for perinatal care in 1982 – closely paralleled the March of Dimes TIOP I Regionalization crumbled in the 90’s when funding was cut 2
3/4/2013 + Perinatal Guidelines - 2009 + 2012 Release of Perinatal Levels of 13 14 Care Guidelines – AAP/ACOG The Michigan Legislature asked the Department of NOTE: AAP/ACOG have released NEW Perinatal Level of Care Community Health: Guidelines “Convene appropriate stakeholders to determine the Level I efficacy and impact of restoring a statewide coordinated Level II regional perinatal system in Michigan.” Level III (NICU) The Michigan Perinatal Level of Care Guidelines are based on Level IV (NICU) AAP/ACOG Level of Care Guidelines modified to reflect Michigan’s standards. Perinatal Regionalization + Birth Hospitals in Michigan 15 16 TIME DEPENDENT EMERGENCY SYSTEM “ right patient ‐ right care ‐ right time. ” 83 Total (Plus Detroit Children’s NICU) Keweenaw Houghton Time Dependent Ontonagon Emergencies Baraga Gogebic Luce Regions Marquette Alger Chippewa Birth Hospitals In Michigan Iron Schoolcraft Mackinac Dickinson Region 1 Delta by Level of Care Region 2S Emmet 45 Menominee 42 Cheboygan Region 2N Charlevoix Presque Isle 40 1 Montmorency Region 3 Antrim Otsego Leelanau Alpena COLLABORATIVE EFFORT 35 Benzie Grand TraverseKalkaskaCrawford Oscoda Alcona Region 5 Number of Birth Hospitals EMS/Trauma • Iosco Wexford Ogemaw 30 Manistee Missaukee Region 6 Roscommon Stroke • Arenac 25 Clare Huron Region 7 Stemi Mason Lake Osceola Gladwin 22 • Isabella Midland 20 Oceana 20 Perinatal Newaygo Mecosta Bay Region 8 • Sanilac Tuscola Montcalm Pediatrics 15 • Muskegon Gratiot Saginaw Kent St. Clair Genesee Lapeer Ottawa Ionia Clinton Shiawassee 10 Oakland Macomb Livingston Allegan Barry Eaton Ingham Wayne 5 Van Buren Kalamazoo Calhoun Jackson Washtenaw 0 St. Joseph Berrien Level I Level II Level III Cass Branch Hillsdale Lenawee Monroe + Perinatal Guidelines - 2009 + Perinatal Guidelines - 2009 17 18 NICU - Level IIIA, B, C Level I and Level II NOTE: 2012 will have Level III and Level IV Level I (Basic) [Unchanged for 2012] Community-Based Maternal-Newborn Service Level IIIA (Subspecialty) Level III B (Subspecialty) ≥ 35 weeks gestation Perinatal Care Center and Neonatal Perinatal Care Center and Neonatal Intensive Care if uncomplicated births Intensive Care Unit Care Unit with Neonatal Subspecialty Service > 28 weeks gestation and weight > 1,000 gm < 28 weeks gestation and weight < 1,000 gms NOTE: 2012 Guidelines eliminate the A & B – will be Level II or with complex illnesses At least 15 VLBW infants born per year At least 70 VLBW infants per year Level II A (Subspecialty) CPAP and conventional mechanical Level II B (Subspecialty) ventilation High frequency ventilation, Inhaled nitric oxide Community-Based Maternal- Community-Based Maternal- Minor surgery, central line and hernia repair Newborn Service with a Special Pediatric surgery (except cardiac) Newborn Service with a Special Care Nursery Women without significant co-morbidities All maternal conditions Care Nursery > 32 weeks gestation > 32 weeks gestation > 1,500 gm Level III C (Subspecialty) > 1,500 gm Uncomplicated preterm infant Perinatal Care Center or Freestanding Pediatric Hospital with Neonatal with problems that are expected Uncomplicated preterm infant Subspecialty Service to resolve rapidly CPAP and mechanical < 28 weeks gestation and weight < 1,000 Stabilization of sick newborn gms or with complex illnesses ventilation for less than 24 hours infants until transfer only At least 70 VLBW infants per year No surgery No surgery Infants with ECMO or open cardiac surgery All maternal conditions Level II is NOT regulated! 3
Recommend
More recommend