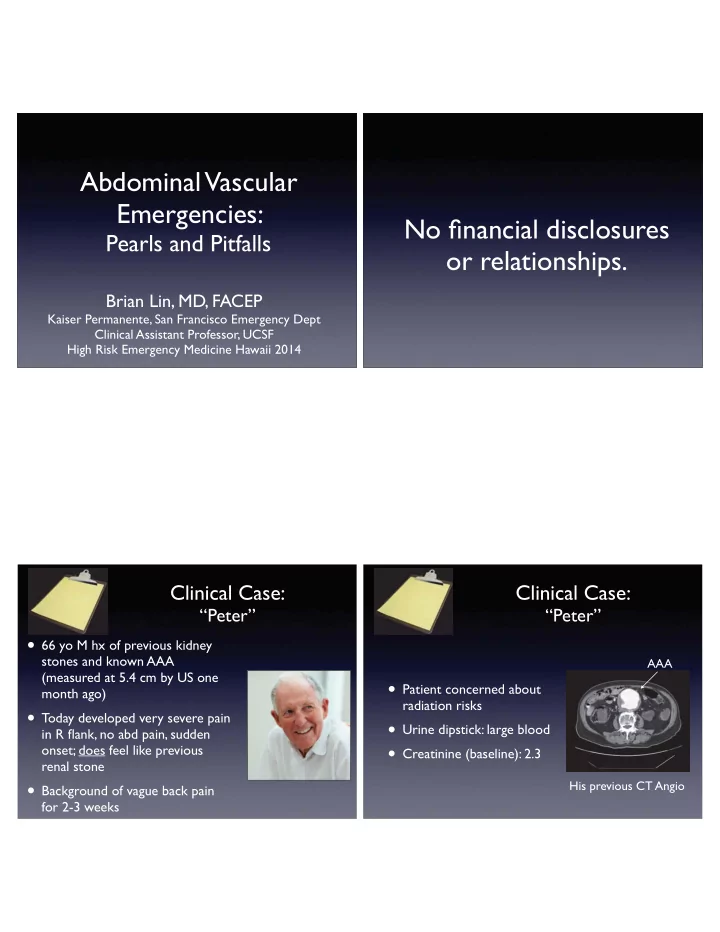
Abdominal Vascular Emergencies: � No fi nancial disclosures Pearls and Pitfalls � or relationships. Brian Lin, MD, FACEP � Kaiser Permanente, San Francisco Emergency Dept � Clinical Assistant Professor, UCSF � High Risk Emergency Medicine Hawaii 2014 Clinical Case: � Clinical Case: � “Peter” “Peter” • 66 yo M hx of previous kidney stones and known AAA AAA (measured at 5.4 cm by US one • Patient concerned about month ago) � radiation risks � • Today developed very severe pain • Urine dipstick: large blood � in R fl ank, no abd pain, sudden • Creatinine (baseline): 2.3 onset; does feel like previous renal stone � • Background of vague back pain His previous CT Angio for 2-3 weeks
Strategy Detection � Decision � Diagnosis � Abdominal Vascular Emergencies (When/How � (ED Treatment � (Imaging) to Test) & Consults) Dx CT angio � Volume + � ~60 yrs + � OR � (Vasc) Surg � Concerning hx US, CT(-) with or � Pulsatile mass AAA Abdominal Aortic � clinical picture � Die Aneurysm (AAA) Lower BP! � Good Hx, (1) CTA � A: Surgery � “Weird” Exam (2) TEE � Aortic Dissection (AD) B, complicated: Consider U/S: take a (Vasc) Surgery � AD Ddimer, US look... B: Medicine � Abd pain Volume, abx, +elderly heparin gtt; � CTA +embolic risk � IR + � AMI +/- lactate (Vasc) Surgery Acute Mesenteric Ischemia (AMI) Goals & Objectives Pearls and Pitfalls � related to: AAA History & Physical • History & Physical � • Serum Biomarkers � AD • Diagnostic Imaging AMI
Physical Exam: � History AAA AAA Abdominal Palpation • Sudden onset • Sensitivity: 76% � epigastric pain � • PPV: 43% � AAA • Flank pain or • Flank pain or • Positive Likelihood back pain � back pain ratio: 15.6 • Syncope [CI 8.6-15.6] JAMA 1999 Contained Rupture Considering AAA? � Take Home Point #1 Look at the legs! AAA Abdominal vascular emergencies don’t always present within the abdomen.
Aortic Dissection History: Pitfall: Positive Likelihood Ratios AD You have to look! Increased Disease Symptom/Finding Probability Tearing/Ripping Pain 10.8x (5.2-22.0) Migrating Pain 7.6x (3.6-16.0) Sudden Chest Pain 2.6x (2.0-3.5) Focal Neuro De fi cit 33.0x (2.0-549.0) JAMA 2002 Weird Presentations AD AD Chest 1998 • Retrospective review of con fi rmed AD cases � • Only 42% had documentation of pain quality, radiation, & onset � dx made 91% of the time � • If all 3 asked: � dx made 49% of the time • If just one omitted:
Malperfusion syndromes Take Home Point #1 AD Stroke syndromes Aortic valve insuf fi ciency Abdominal vascular emergencies don’t Myocardial Infarction always present within the abdomen. Pericardial tamponade Paraplegia Chest, abdominal, or back pain + � Renal failure fi ndings in unrelated or � Intestinal ischemia multiple organ systems = � think aortic dissection Acute Limb Ischemia Clinical Case: � “Paul” � • 69 yo M with HTN, c/o sudden onset sharp Serum Biomarkers chest pain radiating to the abdomen � • EKG: new anterior TWIs Trop 0.00 � • EP considers dissection, but believes it is consider ACS hedges and orders a D-dimer S h while calling medicine admission. ile calling
Biomarkers for AD D-dimer for AD: AD AD Current Evidence D- dimer Am J Cardiol 2011 • 7 studies, 298 pts with AD, 436 without � • Multiple assays; D-dimer cut-off 500 ng/ml � • Basis: observational data, cohort studies � • Sensitivity ~97%, Speci fi city 56%, LR (-) 0.06 • Potential “rule out” test? � • Prognostic value? 3% ? D-dimer for AD: D-dimer for AD: AD AD Biochemical Mechanism What we need to know • False negatives rates in dissection variants/ TF patient subsets � TF D- dimer TF D- dimer D- dimer D- dimer TF • Time of rise, peak, clearance ? � TF D- dimer - dim D- dimer • Prospective studies in undifferentiated CP Intramural Hematoma Aorta
Clinical Case 2: � Clinical Case 2: � “Paul” � “Paul” � • Cardiothoracic Surgery consulted • D-dimer >4000. (7 hrs later) � Results as pt hits • Survives surgery; medicine fl oor discharged home; (2.5 hr turnaround) � readmitted with • Goes to CT: complications & died one week later Type A Dissection Type A Dissection Lactate for Take Home Point #2 Mesenteric Ischemia? AMI Serum biomarkers can help you . � Lactate …they can also hurt you! • Common practice: “rule out” mesenteric ischemia � • Basis: elective surgical pts, case series
Lactate for L-lactate vs D-lactate Mesenteric Ischemia? AMI AMI L-lactate D-lactate D- Lactate • Produced by • Produced by E.coli D- Lactate L-Lactate gut lumen human cells � • Non-speci fi c � bacteria � • More speci fi c � • Elevation not • Common practice: “rule out” mesenteric ischemia � early L-Lactate • Basis: elective surgical pts, case series Biomarker Pitfalls: � Take Home Point #2 Attribution Errors AMI Serum biomarkers can help you. � J Emerg Med 2012 • Amylase elevation (27%) � …they can also hurt you! • LFT elevation (25%) � • Troponin (TnI) elevation (43%)
Strategy Detection � Decision � Diagnosis � (When/How � (ED Treatment � (Imaging) to Test) & Consults) Dx CTA � CTA Volume + � ~60 yrs + � OR � OR OR OR OR OR OR OR OR (Vasc) Surg � Concerning hx US, CT(-) with or � Pulsatile mass AAA clinical picture � p Die Diagnostic Imaging Lower BP! � Good Hx, (1) CTA (1) CTA � A: Surgery � “Weird” Exam (2 (2 (2 (2 (2 (2 (2) T E (2 (2) TEE � EE EE EE EE EE EE EE EE E B, complicated: Consider U/S: take a (Vasc) Surgery � AD Ddimer, US look... B: Medicine � Abd pain Volume, abx, +elderly heparin gtt; � CTA CTA +embolic risk � IR + � AMI +/- lactate (Vasc) Surgery De fi nitive Diagnosis Take Home Point #3 CT angiogram is the test of choice BUT we cannot, and should not, for diagnosis of AAA, aortic CT scan everybody. dissection, and mesenteric ischemia.
Radiation Risk is Real Beyonce says: Number of scans Effective CXR needed to cause radiation dose “If you like it Equivalents a cancer in a (mSv) 60 yo M than you 2 30 14,680 should’ve put CT Head a ring on it.” CT Angiogram 24 220 840 Dissection protocol Smith-Bindman, et al, Arch Int Med 2009 Bedside Ultrasound Brian-say: “If you don’t like it, than you should’ve put an ultrasound on it.”
Abd Aortic US: Identi fi cation AAA Acad Emerg Med 2013 • include Table 3 • in Aorta in in in in in in in in incl in in in n n n cl c ud cl cl cl cl l ud ude Ta ud ud ud ud ud ud ud ud ud ud ud ud ud ud ud ud ud ud ud ud ud ud d d d d T bl Ta Ta Ta bl bl ble 3 bl IVC Vertebral � body Abd Aortic US: Abd Aortic US: Technique Detecting Abnormal AAA AAA Tapers distally >3cm <3cm AortaBifurcation Normal AAA Cephalad Caudal
Right mid axillary view AAA R mid-axillary lateral Liver view increases aortic IVC visualization by 28% Aorta Am J Emerg Med 2013 Abd Aortic US: Ultrasound for AD Don’t forget to look at the RUQ! AAA AD ...worth a look? J Emerg Med 2007 Free fl uid J Emerg Med 2010 Acad Emerg Med 2010
Aortic US Windows Suprasternal Aortic View AD AD • Used to visualize aortic arch � Suprasternal view Subxiphoid view Intra abdominal aorta • May show Type A dissection fl ap Longitudinal abd aorta R midaxillary view RUQ FAST Parasternal cardiac view Suprasternal Aortic View Suprasternal Aortic View AD AD Normal Abnormal Dissection Flap
Abdominal view Take Home Point #3 AD Aorta Longitudinal We cannot, and should not, CT scan everybody. � Consider alternative imaging Dissection Flap strategies, especially ultrasound! Clinical Case 3: � Clinical Case 3: � “Mary” “Mary” • 76 yo F with hx of DM, a fi b, • WBC 14.8K � previous ischemic CVA, hx of right renal artery • Lactate 4.2 � embolism, CKD (cre = 2.3) � • Lipase 492 � • c/o diffuse pain • INR 1.0 � She’s sweating, moaning � • Abd exam: “unimpressive • Cre = 2.3 tenderness”
CT scans, IV contrast, Take Home Point #3 and the beans AMI Emerg Radiol 2010 • In con fi rmed mesenteric We cannot, and should not, ischemia cases: � CT scan everybody.* � • 90% mortality if CT(-) � • 42% mortality if CTA � *…but don’t be afraid to scan those Eur J Vasc Endovasc Surg 2012 who really need it! � • CTA Creatinine bumped, no HD nor mortality Clinical Case: � Clinical Case: � “Peter” “Peter” • Patient placed on monitors, 2 large • CT (-) reveals: 6 mm right bore IVs, labs including Type & Cross. � ureteral stone; AAA stable in size and contour • Abdominal FAST US reveals no free with “no signs to suggest fl uid and patient hemodynamically rupture” � stable. � • “Given this and alternate AAA • Risk/bene fi t ratio involving the diagnosis, we opted not to patient; agree upon CT non-contrast continue with CTA.” Non-contrast CT
Recommend
More recommend