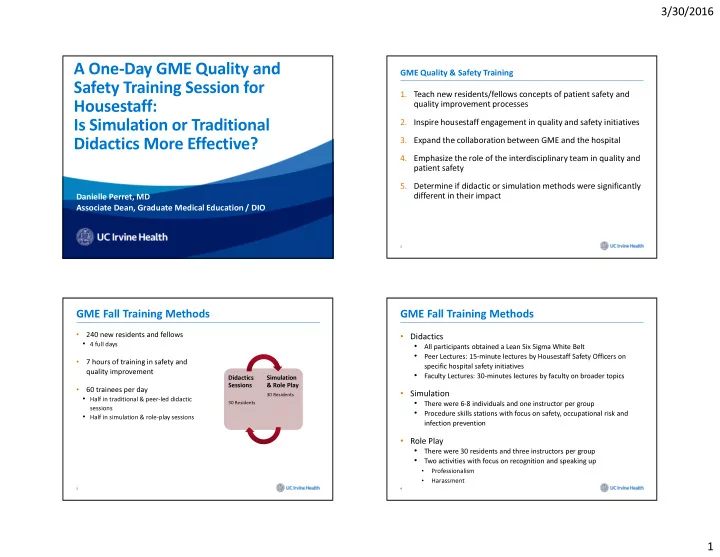
3/30/2016 A One-Day GME Quality and GME Quality & Safety Training Safety Training Session for 1. Teach new residents/fellows concepts of patient safety and quality improvement processes Housestaff: 2. Inspire housestaff engagement in quality and safety initiatives Is Simulation or Traditional 3. Expand the collaboration between GME and the hospital Didactics More Effective? 4. Emphasize the role of the interdisciplinary team in quality and patient safety 5. Determine if didactic or simulation methods were significantly different in their impact Danielle Perret, MD Associate Dean, Graduate Medical Education / DIO 2 GME Fall Training Methods GME Fall Training Methods • • Didactics 240 new residents and fellows • 4 full days • All participants obtained a Lean Six Sigma White Belt • Peer Lectures: 15-minute lectures by Housestaff Safety Officers on • 7 hours of training in safety and specific hospital safety initiatives quality improvement • Faculty Lectures: 30-minutes lectures by faculty on broader topics Didactics Didactics Simulation Simulation Sessions Sessions & Role Play & Role Play • 60 trainees per day • Simulation 30 Residents 30 Residents • Half in traditional & peer-led didactic • 30 Residents 30 Residents There were 6-8 individuals and one instructor per group sessions • • Half in simulation & role-play sessions Procedure skills stations with focus on safety, occupational risk and infection prevention • Role Play • There were 30 residents and three instructors per group • Two activities with focus on recognition and speaking up • Professionalism • Harassment 3 4 1
3/30/2016 GME Fall Training Methods Didactics • Self-assessment questionnaires were completed by each trainee before and after the training using a Likert scale from 1- 5, ranging from “not at all” to “extremely” • attitude about quality and safety efforts • perceived knowledge of safety and quality process initiatives • comfort level with procedures • attitude about targeted interpersonal interactions • 13 question pre- and post-test was added to evaluate knowledge before and after the sessions (2/4 sessions) 5 ‹#› Role-Playing and Simulation Simulation Area ‹#› 8 2
3/30/2016 Arterial Line Station Role Play Station 9 10 Participants Results: Self-Assessment Questionnaires 160 • Self-assessment questionnaires were completed by each 136 140 trainee before and after the training • 100% response rate 120 • Didactics • 100 Residents’ and fellows’ self- assessment scores (“rate your knowledge or skill set”) improved in every didactics category from Pre-Training to 80 Post- Training • Simulation 60 54 • The residents’ and fellows’ self-assessment scores (“rate your comfort level at doing procedures”) improved in every simulation category from 40 29 Pre-Training to Post-Training 20 4 2 0 11 12 PGY1 PGY2 PGY3 PGY4+ Fellow 3
3/30/2016 Didactic Presentations: Self-Assessment Scores Simulation: Self-Assessment Scores ‹#› ‹#› Results: Medical Knowledge Scores Conclusion • • Medical Knowledge In comparing the efficacy of simulation vs. didactic teaching, both were • significant improvement evidently effective (averaging greater than 20% improvement) in increasing • overall change in scores from the pre- to the post-test knowledge, but there was no discernible significant difference between the • 90 +/- 27 to 97 +/- 24 two methods' efficacy • p = 0.024 • A multidisciplinary team of physicians, nurses, administrators, GME and 120.00% medical school leaders developed and delivered a new curriculum 100.00% concerning quality and safety as well as process improvement topics, provided to new housestaff as both didactic and simulation-based teaching. 80.00% PRE Simulation and didactics were equally effective teaching strategies. Trainees 60.00% POST portrayed improved understanding of all topics over the course of the day. 40.00% These sessions resulted in excellent short-term outcomes of success as % change measured by pre- and post-testing of housestaff self-assessments and 20.00% medical knowledge 0.00% Q.1 Q.2 Q.3 Q.4 Q.5 Q.6 Q.7 Q.8 Q.9 Q.10 Q.11 Q.12 Q.13 -20.00% 15 16 4
Recommend
More recommend