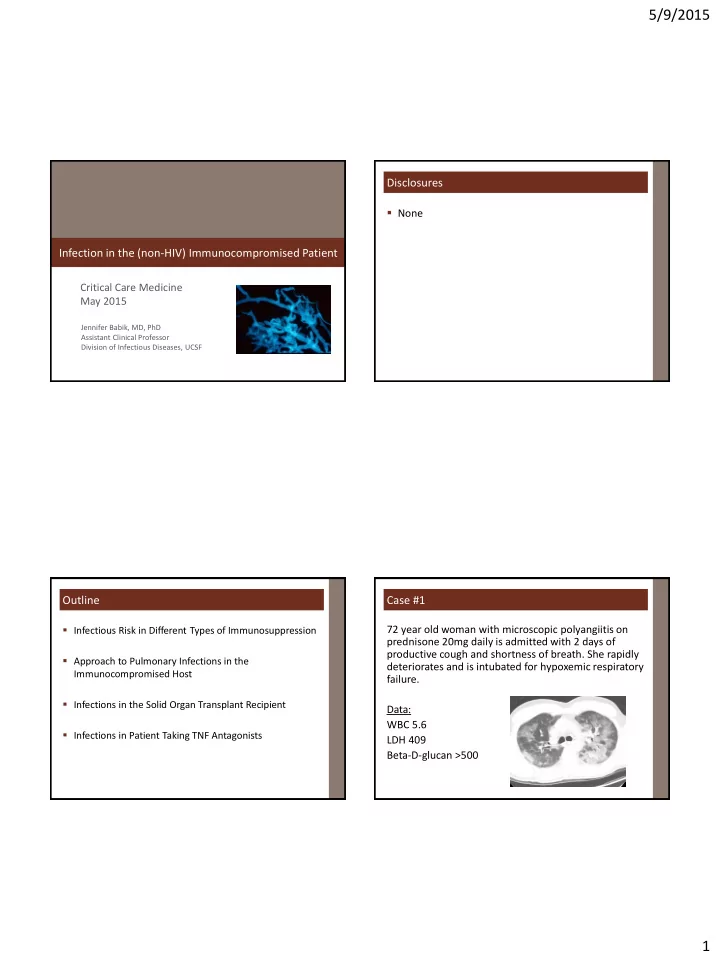
5/9/2015 Disclosures None Infection in the (non-HIV) Immunocompromised Patient Critical Care Medicine May 2015 Jennifer Babik, MD, PhD Assistant Clinical Professor Division of Infectious Diseases, UCSF Outline Case #1 Infectious Risk in Different Types of Immunosuppression 72 year old woman with microscopic polyangiitis on prednisone 20mg daily is admitted with 2 days of productive cough and shortness of breath. She rapidly Approach to Pulmonary Infections in the deteriorates and is intubated for hypoxemic respiratory Immunocompromised Host failure. Infections in the Solid Organ Transplant Recipient Data: WBC 5.6 Infections in Patient Taking TNF Antagonists LDH 409 Beta-D-glucan >500 1
5/9/2015 Your empiric antibiotic regimen should include: General Principles of Immunocompromised Host ID 1. Patients can present without overt signs of infection 1. Ganciclovir (e.g. afebrile, normal WBC count) 2. Voriconazole 2. Patients can get very sick, very fast 3. TMP-SMX 3. Threshold for more aggressive diagnostics (imaging, invasive procedures) and for empiric therapy should be lower 4. Liposomal amphotericin 4. The kind of immunocompromise matters – i.e. what kind of infections is the patient at risk for? Common States of Immunosuppression Can We Quantify Immunosuppression? Common States of Immunosuppression Neutropenia Infectious risk in HIV-negative patients is hard to Hypogammaglobulinemia determine HIV Quantitative CD4 depletion (can measure) Asplenia Non-HIV immunosuppression Qualitative CD4 Cell-mediated immunity dysfunction dysfunction (no reliable way to measure this) HIV Solid organ transplantation Are there surrogate markers we can use? Stem cell transplantation Underlying disorder Autoimmune disorders Immunosuppressive drugs: duration and dosage TNF-alpha inhibition and other biologic agents Other OIs Kowalski, Clin Transplantation, 2003. 2
5/9/2015 Infectious Risk of Different Immune Defects Approach to Pulmonary Infections in ICH What is the degree/cause of immunosuppression? Immune Defect Bacteria TB/ Endemic Molds PCP Herpes HBV NTM mycoses viruses What is the pattern of the pulmonary infiltrates? Neutropenia +++ + + ++ +/- + ++ HypoIgG ++ Asplenia ++ What is the tempo of the pulmonary symptoms? Cell-mediated + ++ ++ +++ +++ +++ +++ immunity TNF-inhibition + +++ +++ + Rituximab +++ STEROIDS Slide courtesy of B Schwartz Pattern of Pulmonary Infiltrates Tempo of Pulmonary Symptoms Segmental/lobar: Segmental/lobar: Common bacterial pathogens Common bacterial pathogens Acute Legionella Legionella Acute Nodules: Nodules: Cryptococcus, Histoplasma, Coccidioides Cryptococcus, Histoplasma, Coccidioides Subacute Aspergillus, Zygomyces Aspergillus, Zygomyces Subacute Nocardia Nocardia Subacute Mycobacteria Mycobacteria Subacute Malignancy Malignancy Subacute Diffuse: Diffuse: PCP PCP Acute** CMV CMV Subacute Respiratory viruses (e.g. influenza, RSV, adenovirus, parainfluenza, Respiratory viruses (e.g. influenza, RSV, adenovirus, parainfluenza, metapneumovirus) metapneumovirus) Acute to Subacute Drug-induced ALI Drug-induced ALI Subacute 3
5/9/2015 PCP in HIV-negative Patients Case #2 68 y/o woman s/p cadaveric HIV-positive HIV-negative renal transplant 5 weeks ago Clinical Subacute presentation (weeks) Acute (<1 week) (CMV D+R-) is brought to the Survival >80% Survival 50-90% ED with progressive shortness Radiology Diffuse bilateral infiltrates Same of breath over 1 week and Beta-D-Glucan 90-95 % sensitive Same sensitivity rapidly requires intubation. 65-90% specific 85-90% specific LDH 92-100% sensitive 64-100% sensitive 25-85% specific Same specificity She had been induced with thymoglobulin and is now BAL Microscopy >90% sensitive 62-85% sensitive (high organism burden) (low organism burden) taking mycophenolate, tacrolimus, and prednisone. de Boer, J Infect 2011. Tasaka, Chest 2007. Oren, Am J Med Sci 2011. Tia, Clin Microbiol Infect 2011. Vogel, Swiss Med Weekly 2011. Tasaka, J Infect Chemother 2012. Sepkowitz, CID 2002. The Most Likely Diagnosis is: Case #2: Diagnosis 1. CMV Lactophenol cotton blue stain on culture KOH stain 2. Aspergillus 3. Rhizopus Gram stain 4. S. aureus 4
5/9/2015 The Effects of Thymoglobulin Last For: How to Approach Infectious Risk Post-Transplant Organ type 1. 1 week Timing after transplant Induction regimen (if within ~1 year of transplant) 2. 3 months Maintenance regimen and doses Augmented immunosuppression because of 3. 6 months rejection? Other OIs? 4. >12 months Timing of Immunosuppression in SOT Classic Timeline of Infections Post-transplant Degree of Immune Suppression OPPORTUNISTIC COMMUNITY ACQUIRED Degree of immunosuppression Risk of Infection Nosocomial, Technical, Donor-derived Opportunistic Infections Community-acquired infections Anastomotic complications Late viral infections or OIs (especially if immunosuppression) Reactivation of latent infections Cdiff Cdiff 1 2 3 4 5 6 7 8 9 10 11 12 Months post-transplant Wiesner and Fung, Liver Transplant 2011. 5
5/9/2015 Types of Immunosuppression in SOT UCSF Examples of Induction/Maintenance Induction Maintenance Rejection Induction Maintenance Steroid Antibody 1. Methylprednisolone 1. Calcineurin inhibitor 1. Methylprednisolone Tacrolimus > Cyclosporine Liver Methylpred None Tacrolimus Mycophenolate 1. +/- Anti-lymphocyte Ab 1. +/- Anti-lymphocyte Ab Prednisone Thymoglobulin 2. Antiproliferative Thymoglobulin (Alemtuzumab) MMF > Azathioprine Renal Methylpred Basiliximab, Thymo, Tacrolimus Alemtuzumab Basiliximab or None Mycophenolate Prednisone 3. Prednisone 2. +/- Others Lung Methylpred Basiliximab >> Tacrolimus Sirolimus Thymoglobulin Mycophenolate 4. Others : Rituximab Prednisone Sirolimus Heart Methylpred Thymoglobulin Tacrolimus Mycophenolate Prednisone Infectious Risk in Solid Organ Transplant Lymphoctye Antibodies for Induction Antithymocyte globulin Basiliximab Immune Defect Bacteria TB/ Endemic Molds PCP Herpes HBV Rabbit polyclonal IgG against T Anti-CD25: inhibits IL-2 binding NTM mycoses viruses and B cells and T cell proliferation Neutropenia +++ + + ++ +/- + ++ Depleting Ab: effect lasts >1 year Non-depleting Ab: effect lasts 4-6 HypoIgG ++ weeks Also used in refractory rejection Asplenia ++ Lower potency, less infectious Increases risk for many infections Cell-mediated risk – used for lower risk (including viral, PCP, fungal) + ++ ++ +++ +++ +++ +++ immunity recipients TNF-inhibition + +++ +++ + Rituximab +++ Slide courtesy of B Schwartz Halloran, NEJM 2004. Issa and Fishman, CID 2009. 6
5/9/2015 Duration of Lymphocyte Depletion: Thymoglobulin Infectious Risk of Maintenance Drugs Most drugs studied together hard to assign individual risk Calcineurin Inhibitors (tacrolimus, cyclosporine): risk viruses (CMV), PCP Antiproliferatives (mycophenolate, azathioprine): risk viruses (CMV, VZV) Prednisone: Dose-dependent risk for wide range of infections Normal Range of ALC The drugs together put SOT recipients at risk for a wide range of infections (bacterial, fungal, viral, parasitic) Halloran, NEJM 2004. Thomas et al, Am J Transplant 2009. Singh, Curr Opin ID 2005. Husain and Singh, CID 2002. Ritter et al, Brennan, Transpl Proc 1999. Transpl ID 2009. Meta-Analysis of Glucocorticoids and Infection Case #3 63 studies in RA patients, significant heterogeneity A 55 y/o man with RA on infliximab and low dose MTX x 9 months presents with 4 weeks of severe fatigue, weight loss, Dose dependent risk: and multiple painful skin lesions. <5mg/day RR 1.37 On admission his vtials are: 5-10mg/day RR 1.93 39˚C, HR 125, BP 85/50, RR20, 10-20mg/day RR 2.97 SaO2 92% RA. He is admitted to the ICU. >20mg/day RR 4.30 He had immigrated to the US from Mexico at the age of 45 and now lives in Fresno. Dixon et al, Arthr Res Ther 2011. 7
5/9/2015 The infliximab puts him at high risk for: Case #3: Diagnosis 1. Tuberculosis 2. Coccidioidomycosis 3. Histoplasmosis Skin biopsy positive for Coccidioides 4. All of the above 1 out of 4 blood cultures positive for Coccidioides Cocci immunodiffusion positive Cocci comp fix titer 1:256 TNF Antagonists TNF Antagonists and Granulomatous Infections the risk of granulomatous infections by ~5 fold: (Embrel) (Remicade) (Humira, Simponi) (Cimzia) TB Histoplasma Coccidioides Agents interfere with new granuloma formation and weaken the integrity of existing granulomas Soluble TNF receptor Anti-TNF Antibodies Wallis, ID Clinics NA 2011. Wallis, ID Clinics NA 2011. 8
Recommend
More recommend