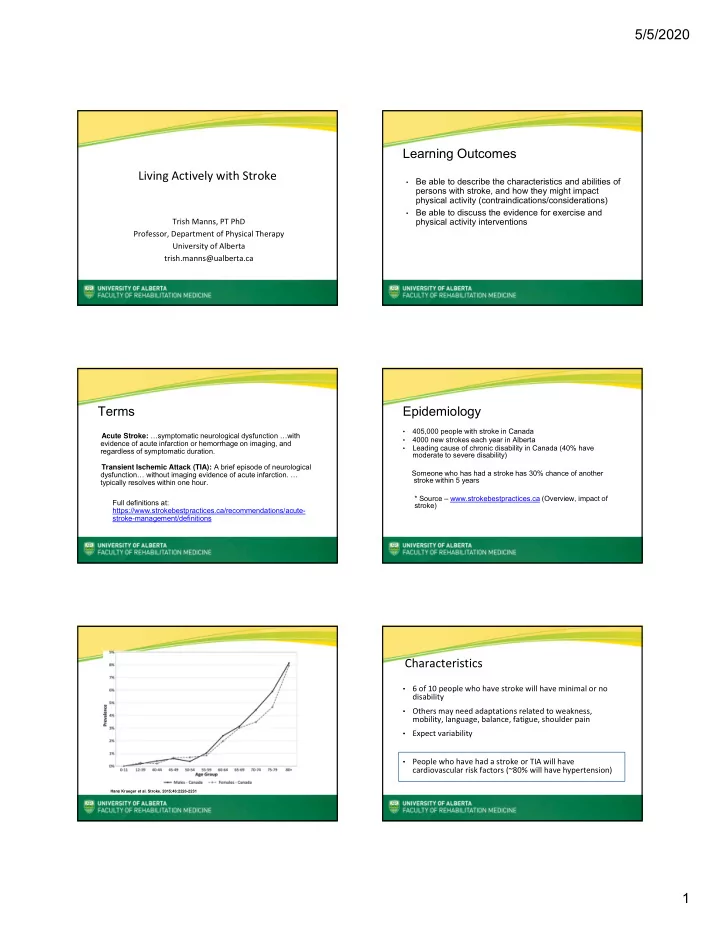
5/5/2020 Learning Outcomes Living Actively with Stroke Be able to describe the characteristics and abilities of • persons with stroke, and how they might impact physical activity (contraindications/considerations) Be able to discuss the evidence for exercise and • physical activity interventions Trish Manns, PT PhD Professor, Department of Physical Therapy University of Alberta trish.manns@ualberta.ca Terms Epidemiology • 405,000 people with stroke in Canada Acute Stroke: …symptomatic neurological dysfunction …with • 4000 new strokes each year in Alberta evidence of acute infarction or hemorrhage on imaging, and • Leading cause of chronic disability in Canada (40% have regardless of symptomatic duration. moderate to severe disability) Transient Ischemic Attack (TIA): A brief episode of neurological Someone who has had a stroke has 30% chance of another dysfunction… without imaging evidence of acute infarction. … stroke within 5 years typically resolves within one hour. * Source – www.strokebestpractices.ca (Overview, impact of Full definitions at: stroke) https://www.strokebestpractices.ca/recommendations/acute- stroke-management/definitions Characteristics • 6 of 10 people who have stroke will have minimal or no disability • Others may need adaptations related to weakness, mobility, language, balance, fatigue, shoulder pain • Expect variability • People who have had a stroke or TIA will have cardiovascular risk factors (~80% will have hypertension) Hans Krueger et al. Stroke. 2015;46:2226-2231 1
5/5/2020 Shoulder Why Exercise and Physical Activity? From Evidence Based Review of Stroke Rehabilitation (ebrsr.com). Chapter 11 Hemiplegic Shoulder Pain and Complex Regional Pain Syndrome Maintain or add to improvements Improve capacity for everyday activity From Rimmer, J. (2012). Getting beyond the plateau: bridging the gap between rehabilitation and community based exercise. PM R, 4; 857-861 Ivey FM, Hafer-Macko CE, Macko RF. Exercise rehabilitation after stroke. NeuroRx 2006; 3(4): 439-50. Evidence – specific to aerobic training Best Practices – Aerobic Training • Exercise capacity (Level of Evidence A) • Balance/mobility (Level of Evidence A) • Vascular risk reduction (Level of Evidence B) Physical activity - bodily movement, results in energy expenditure https://www.canadianstroke.ca/en/news/2019-update-aerobics- Exercise - planned, structured (recurrent) guidelines-now-available Reference: New Aerobics 2019 update https://www.canadianstroke.ca/en/news/2019 ‐ update ‐ aerobics ‐ guidelines ‐ now ‐ available 2
5/5/2020 Screening? Who? Stress test? Examples of symptom limiting screening tests in the Aerobics Update (page 24). https://www.canadianstroke.ca/en/news/2019-update- https://www.canadianstroke.ca/en/news/2019-update- aerobics-guidelines-now-available aerobics-guidelines-now-available Best Practice Recommendations in a Nutshell Strength Training • Mode of exercise – large muscle groups (cycle, NuStep, • Improves strength! Use similar principles as with walking) persons without stroke (overload, repetition) • How long? At least 8 weeks • Can do bilateral • Training for function • Freq/Duration? 3 days per week, 20 minutes per session • Monitor shoulder • Intensity Considerations • Strength training on stronger side is a possibility • No stress test, no/limited experience with exercise – start (useful when one side has weakness that makes it low/light (<40% heart rate reserve) difficult to train) • If using heart rate, people on beta blockers will have blunted heart rate responses Strength training guidelines can be found in: Billinger, S. A., Arena, R., Bernhardt, J., Eng, J. J., Franklin, B. A., Johnson, C. M., . . . Tang, A. (2014). Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American heart association/American stroke association. Stroke; a journal of cerebral circulation, 45 (8), 2532-2553. • interval Contraindications/Precautions Monitoring ● Blood pressure Unstable blood pressure ● Initial testing Criteria for Stopping Exercise ● Pre and post ● Heart rate ● Systolic BP>200 mmHG ● Continuous ● Diastolic BP change by>10mmHg in either direction ● SBP drop by >10mmHg while exercising ● Others ● Onset of angina, poor perfusion, HR at target, abnormal arrhythmia, increasing CNS symptoms, severe SOB * Criteria listed on Sub Max Exercise Test form from Fanning Centre Used with Permission from Liz Reimer, Vernon Fanning Centre Calgary 3
5/5/2020 Think Big Picture Physical Activity? Tremblay, M. S., Aubert, S., Barnes, J. D., Saunders, T. J., Carson, V., Latimer-Cheung, A. E., . . . Participants, S. T. C. P. (2017). Sedentary Behavior Research Network (SBRN) - Terminology Consensus Project process and outcome. The international journal of behavioral nutrition and physical activity, 14(1), 75. Changing behaviour one day at a time Discussion/Conclusions • Changing behaviour is what matters Transitioning from health care system to community • • Many people with stroke will • Strong evidence that exercise and physical activity are have little experience with beneficial for persons with stroke activity ‐ start with activity that will allow success • Whole day activity important • Breaking up sitting • Implications for everyday activity Questions? Contact information: trish.manns@ualberta.ca 4
Recommend
More recommend