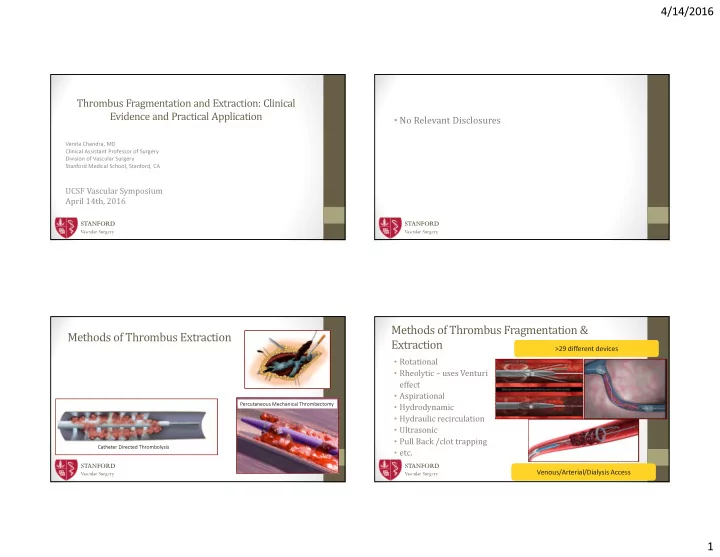
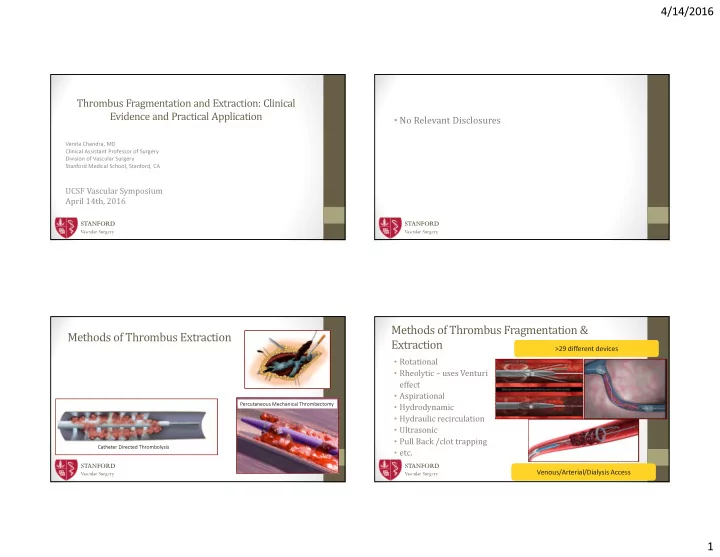
4/14/2016 Thrombus Fragmentation and Extraction: Clinical Evidence and Practical Application • No Relevant Disclosures Venita Chandra, MD Clinical Assistant Professor of Surgery Division of Vascular Surgery Stanford Medical School, Stanford, CA UCSF Vascular Symposium April 14th, 2016 STANFORD STANFORD Vascular Surgery Vascular Surgery Methods of Thrombus Fragmentation & Methods of Thrombus Extraction Extraction >29 different devices >29 different devices • Rotational • Rheolytic – uses Venturi effect • Aspirational Percutaneous Mechanical Thrombectomy • Hydrodynamic • Hydraulic recirculation • Ultrasonic • Pull Back /clot trapping Catheter Directed Thrombolysis • etc. STANFORD STANFORD Venous/Arterial/Dialysis Access Venous/Arterial/Dialysis Access Vascular Surgery Vascular Surgery 1
4/14/2016 Trellis TM* Trellis TM • Pros: limited systemic leakage of thrombolytics, potentially less embolization • Dispersion wire is • Dispersion wire is • Cons: limited in size sinusoidal shape, sinusoidal shape, connected to connected to oscillation drive oscillation drive • Infusion port • Infusion port • Aspiration Port • Aspiration Port • Compliant occlusion • Compliant occlusion STANFORD STANFORD balloons balloons Vascular Surgery * Bacchus Vascular, Santa Clara, CA Vascular Surgery AngioJet TM Catheter* Case- Angiojet • Clotted Brachial-Axial AV graft • Technique • Access both retrograde/antegrade • Infuse TpA through Angiojet Catheter on Power pulse mode Hypotube and jet body • Rheolytic Thrombectomy • Rheolytic Thrombectomy • Wait 20-30 minutes • Jet flow of saline creates • Jet flow of saline creates low pressure zone (Venturi low pressure zone (Venturi Effect) Effect) • Low pressure: • Low pressure: • Thrombus • Thrombus fragmentation fragmentation STANFORD • Evacuation • Evacuation STANFORD Vascular Surgery Vascular Surgery * Boston Scientific, Marlborough, MA 2
4/14/2016 • After Power Pulse • After Power Pulse AngioJet TM Catheter • Pros: • Cons: • Less endothelial damage • Cost • Pharmacomechanical option • Hemolysis • Retrograde sheath • Retrograde sheath • Antegrade sheath • Antegrade sheath • Hematuria • Arterial and venous uses • Hyperkalemia • variety of sizes • Bradycardia STANFORD STANFORD • After Thrombectomy • After Thrombectomy Vascular Surgery Vascular Surgery Penumbra Catheter* Penumbra TM • Pros: • Cons: • No Thrombolysis • Risk of blood loss • Extremely trackable • Limitation of catheter sizes • Arterial and venous uses • Large lumen • Large lumen aspiration aspiration • Separator Tip • Separator Tip STANFORD STANFORD Vascular Surgery Vascular Surgery * Penumbra, Alameda, CA 3
4/14/2016 Results of PMT Conclusions • Safety & Feasibility Studies of various devices/Case • Numerous options for PMT Series/Retrospective Reviews • Arterial • Appear to associated with less thrombolytics, less treatment • Technical success: 70-90% time (less ICU stay) and potentially less hospital costs • AV access: compared to CDT • Limited quality data to guide treatment • Technical success: 76-91% • DVT • Clinical decisions: • Technical success: 28.5-100% • Experience/Comfort level • CDT + PMT • Case by case Similar outcomes, shorter hospital stays and less thrombolytics Similar outcomes, shorter hospital stays and less thrombolytics • CDT vs. PMT with PMT* with PMT* STANFORD STANFORD *Kim et. al. Cardiovasc Intervent Radiol (2006) Vascular Surgery Vascular Surgery *Lin et. al. Am Journal of Surgery 2006 PEARL Registry Results Venous 1.4 hrs • 58.5% had 100% clot burden n=329 RT only reduction 4% • 96% had >50% clot burden 2 hrs PCDT reduction Thank You! PCDT + 35% • No significant difference in terms of CDT 52% CDT clot burden reduction vascular.stanford.edu 9% 41 hrs • Significant differences in treatment 22 hrs time STANFORD STANFORD Vascular Surgery Vascular Surgery Garcia, JVIR June 2015, volume 26, Issue 6, pages 777-785 4
4/14/2016 PEARL Registry- Arterial Comparison of outcomes by treatment • n=283, 48% PMT+CDT, 52% PMT only • Procedures were shorter in the PMT only group (1.6 hrs vs. 23.0 hrs) compared to the PMT+CDT group (p<0.001) • Increased rate of stenting in PMT only group • NOT RCT • NOT RCT • Just a registry!! • Just a registry!! STANFORD STANFORD Vascular Surgery Vascular Surgery Daniel A. Leung et al. J Endovasc Ther 2015;22:546-557 Penumbra Case Penumbra Case: Distal • Complicated diabetic, numerous prior interventions for CLI anastomosis of occluded graft over many years • Hoping for limb • Hoping for limb • Infected SFA Viabahns after bout of sepsis salvage salvage • Partial resection of SFA Viabahns, and cadaveric fem-PT bypass • Did not want • Did not want • Occlusion of cadaveric bypass re-opened with CDT thrombolysis thrombolysis • Pseudoaneurysm/degeneration of bypass treated with covered Occluded remnant stent native SFA • Occlusion of bypass treated with CDT, complicated by bleeding Single disease stent vessel runoff Occluded stent • Presents with re-occluded bypass, rest pain and tissue loss (PT) in cadaveric bypass graft STANFORD STANFORD Vascular Surgery Vascular Surgery 5
4/14/2016 Penumbra Case After passage of After balloon penumbra angioplasty catheter STANFORD Vascular Surgery 6
Recommend
More recommend