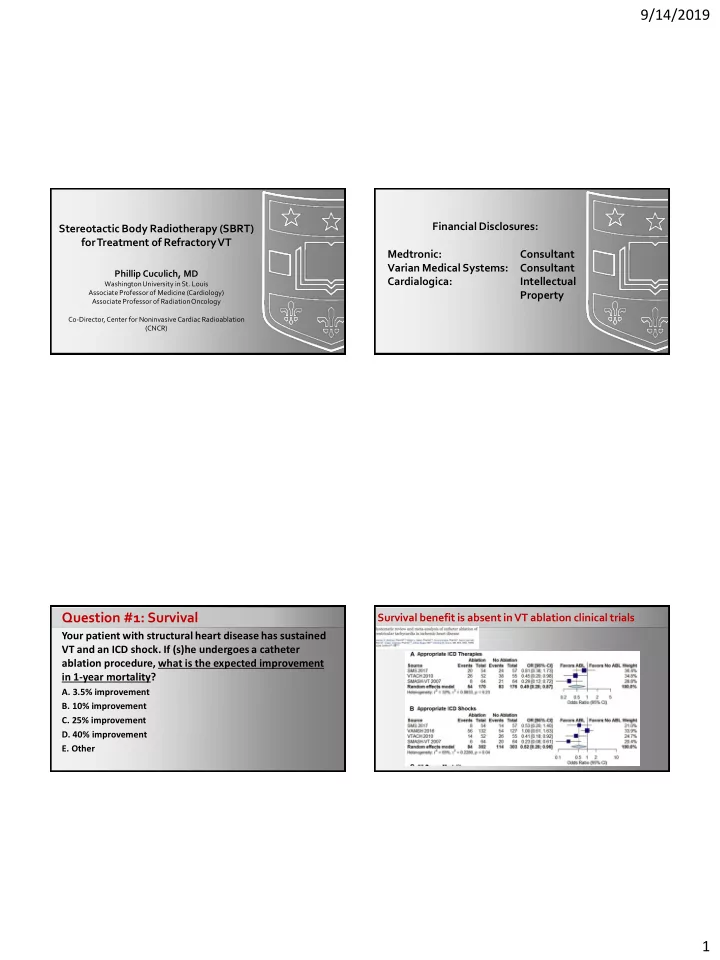
9/14/2019 Financial Disclosures: Stereotactic Body Radiotherapy (SBRT) for Treatment of Refractory VT Medtronic: Consultant Varian Medical Systems: Consultant Phillip Cuculich, MD Cardialogica: Intellectual Washington University in St. Louis Associate Professor of Medicine (Cardiology) Property Associate Professor of Radiation Oncology Co-Director, Center for Noninvasive Cardiac Radioablation (CNCR) Question #1: Survival Survival benefit is absent in VT ablation clinical trials Your patient with structural heart disease has sustained VT and an ICD shock. If (s)he undergoes a catheter ablation procedure, what is the expected improvement in 1-year mortality? A. 3.5% improvement B. 10% improvement C. 25% improvement D. 40% improvement E. Other 1
9/14/2019 Survival benefit is absent in VT ablation clinical trials “Outcomes” associated with clinical & substrate features 31-day mortality for all structural VT catheter ablation: 5% (1 in 20 die) Need More Comprehensive Treatment Stereotactic Body Radiotherapy (SBRT) Surgery SBRT Need it to be LESS risky 2
9/14/2019 Assumption: The EP effect is closely related to Radiotherapy induces fibrosis (dose-dependent) Imaging cell death & fibrosis NIPS Patient selection Imaging / Simulation Workup / Targeting Doses from 25 Gy/1 – 50 Gy/1 • 25 Gy minimum dose to produce electrophysiologic effect by 3 mo • 3-6 mo transmural fibrosis (25-32.5 Gy?) • No clear toxicity in non-target heart or overall heart function Maguire et al . Cureus, 2011, Sharma, et al., Heart Rhythm, 2010; Song, et al., Heart Rhythm, 2014; Wong et al , The CyberKnife Society Meeting Segmentation Treatment Planning Delivery 2008; Blanck, et al, Int J Radiat Oncol Biol Phys, 2014; Lehmann et al, Circ Arrhythm Electrophysiol, 2015 Noninvasive Cardiac Radioablation Imaging NIPS Patient selection Imaging / Simulation Workup / Targeting Segmentation Treatment Planning Delivery 3
9/14/2019 5 patients recurrent VT treated in 2015 (published 2017) Arrhythmogenic scar targeted by combining anatomic imaging and ECGI SBRT delivered to target, 25Gy/1 (no fiducial needed) Mean noninvasive ablation time 14 min (11-18) 3 month pre treatment = 6577 6 week blanking = 680 Next 10.5 months = 4 10 patients recurrent VT treated in 2014-2017 19 patients recurrent VT treated in 2017-2018 ( NCT02919618, published 2018) (published 2019) Arrhythmogenic scar targeted by combining anatomic Arrhythmogenic scar targeted with invasive CARTO maps imaging and ECGI SBRT delivered to target, 25Gy/1 (ICD lead as fiducial) SBRT delivered to target, 25Gy/1 (no fiducial needed) Mean noninvasive ablation time 68 min (45-80) Mean noninvasive ablation time 15 min (5-32) • Baseline characteristics Median Age = 66 y/o (49-81) VT storm (52.6%) PVC cardiomyopathy (10.5%) 89.5% Male 89.5% Caucasian Meds >1 AAD (57.9%) Ischemic (57.9%) >300 mg amio (57.9%) NHYA Class III (52.6%), IV (21.1%) Median LVEF = 25% (15-58) 4
9/14/2019 19 patients recurrent VT treated in 2017-2018 19 patients recurrent VT treated in 2017-2018 ( NCT02919618, published 2018) ( NCT02919618, published 2018) Arrhythmogenic scar targeted by combining anatomic Arrhythmogenic scar targeted by combining anatomic imaging and ECGI imaging and ECGI SBRT delivered to target, 25Gy, 1 fraction SBRT delivered to target, 25Gy, 1 fraction Mean noninvasive ablation time 15 min (5-32) Mean noninvasive ablation time 15 min (5-32) • Primary Endpoint: Any G5/G4/Hospitalized G3 18 of 19 (94%) possibly/probably/definitely related to treatment within patients met primary 90 days: endpoint of reduction in VT burden Median 3 • n=2 (10.5%) Median 119 ICD shocks decreased • Possible : Grade 3 heart failure admission (day 65) p < 0.001 from 4 to 0 (p = 0.002) – treated with diuretics • Probable : Grade 3 pericarditis (day 80) Anti-tachycardia pacing decreased from 81 to 3 – resolved with prednisone (p = 0.001) 6 months BEFORE 6 week BLANKING 4.5 months AFTER • Unlikely: One patient death in first 90 days (day 17) 1778 VT episodes 149 VT episodes 111 VT episodes – accidental, not related to treatment Secondary Endpoints: 19 patients recurrent VT treated in 2017-2018 ( NCT02919618, published 2018) Arrhythmogenic scar targeted by combining anatomic Medication Usage and Quality of Life imaging and ECGI SBRT delivered to target, 25Gy, 1 fraction Mean noninvasive ablation time 15 min (5-32) 35 30 Class I Agents 25 20 Class III Agents 15 Low-Dose 10 Amiodarone Nine SF-36 modules: High-Dose 5 Amiodarone 5 improved 0 4 maintained Baseline 6 Months 0 worsened 5
9/14/2019 Question #2: Next Steps These results for noninvasive ablation look encouraging. What should we do next? A. Isn’t radiation dangerous? You need to understand the biology of how Where do we go from here? radiation affects the heart better – do more animal studies B. Wait, how do you treat a moving target? Figure out the motion management first. Next steps … C. Whoa, how do you know where to ablate if you didn’t use catheters? Figure out the targeting first. D. Radiation can have lasting, late effects. Follow your treated patients for 25 years, then revisit. E. Giddy- up! Let’s do a RCT! Center for Noninvasive Cardiac Radioablation (CNCR) Biology Clinical Population Imaging Process How to determine critical How can we improve & arrhythmia sites? standardize the processes? Longer T erm Results from a Phase I/II Study of EP- Motion Scar architecture guided Noninvasive Cardiac Radioablationfor management Metabolism How is SBRT How should SBRT Can SBRT extend Treatment of Ventricular T achycardia (ENCORE-VT) Automation of Electrical antiarrhythmic? be delivered? access to care? feature analysis In silico Augmented modeling Global Registry Murine (SAARP) ENCORE-VT decision tools C. G. Robinson , P. Samson, K. M. S. Moore, G. D. Hugo, N. Knutson, S. Augmented Democratize VT Mutic, S. M. Goddu, D. H. Cooper, M. Faddis, A. Noheria, T. W. Smith, P. K. Human explant ENCORE-MULTI Scalable & targeting tools Ablation Sharable Woodard, R. J. Gropler, D. E. Hallahan, Y. Rudy, and P. S. Cuculich ENCORE-RCT Washington University School of Medicine in St. Louis 6
9/14/2019 Pha hase II – Effic ficacy Ov Over Tim ime CONFIDENTIAL MRI guidance Per-Patient VT Episodes by 6-month time periods 120 95.5 100 VT Episodes 80 60 Median VT burden 40 20 3.5 1 0 NIH 1 R01 HL148210-01 3.5 0 “Novel imaging and treatment 6 mo PRE 0-6 mo 6-12 mo 12-18 mo 18-24 mo technologies for image-guided noninvasive At risk 18 18 17 14 12 stereotactic cardiac radiosurgery.” (PI: Yang/Gach) CNCR Outreach: Helping Patients Together Towards quality and reproducibility Targeting Collaborative Sciences Award (PI: Robinson/ Cuculich) End-to-end testing Plan quality / Plan automation Clinical Decision Support Tools 7
9/14/2019 Global impact Next Steps: Symposium for Noninvasive Radioablation Key takeaways. . . Caution Moving the field forward together: Clinical trials (avoid hype & bias, Center for Noninvasive choose appropriate endpoints) Cardiac Radioablation (CNCR) Contact: Kaitlin Moore Accessibility (CNCR) (314) 273-0830 sites.wustl.edu/cncr/ Mutual learning Take a picture to be directed to the Center for Noninvasive Cardiac Radioablation 8
9/14/2019 Quality and reproducibility Intensity of tissue damage: • DNA (ds breaks) Direct • RNA, mitochondria Survival Dose (higher dose=greater injury) tissue proteins, lipids effects • Damage response Vs. • Meta-analysis of 8 Speed of dose delivered (faster delivery=more injurious effect) 1.74 X Function cooperative RT studies • Inflammation / Off- Fibrosis (TGF-B) Size of exposed body (the Mortality target • Median 32% rate of bigger part of the body, the more • Vascular effects effects Tumor severe injury) protocol deviations • “ Bystander effect" Vs. • Protocol deviations Sensitivity of tissue to radiation associated with “Normal” • Local Age, Health status, Genetic 1.79 Immune X ~2x increased risk of • Systemic differences treatment failure and Recurrence overall mortality Seconds to minutes Days to weeks Months to years Ohri et al (JCNI, 2013) 9
Recommend
More recommend