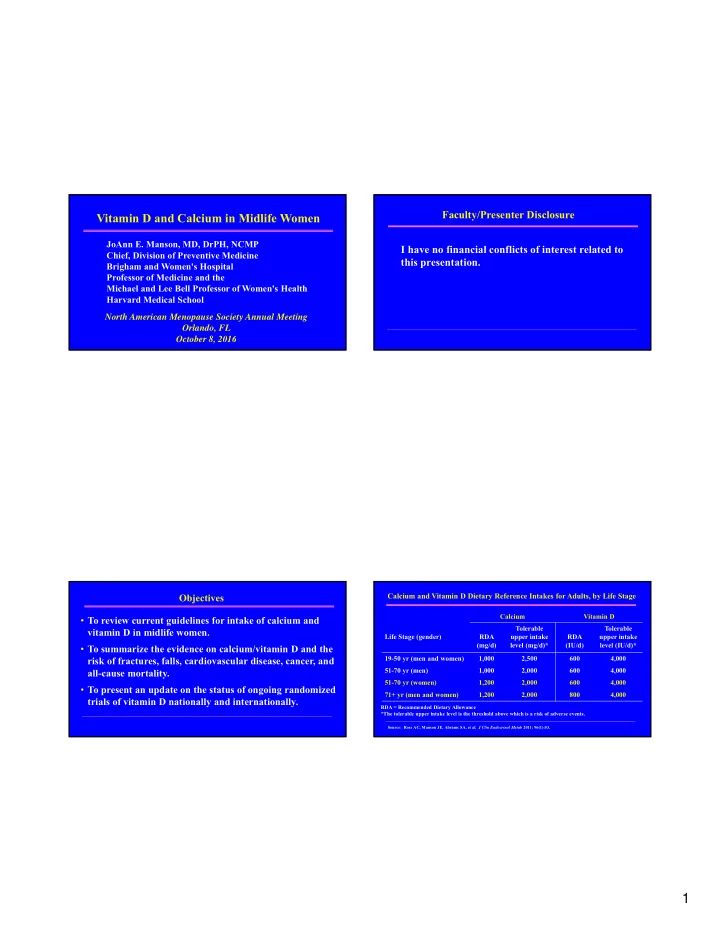
Faculty/Presenter Disclosure Vitamin D and Calcium in Midlife Women JoAnn E. Manson, MD, DrPH, NCMP I have no financial conflicts of interest related to Chief, Division of Preventive Medicine this presentation. Brigham and Women's Hospital Professor of Medicine and the Michael and Lee Bell Professor of Women's Health Harvard Medical School North American Menopause Society Annual Meeting Orlando, FL October 8, 2016 Calcium and Vitamin D Dietary Reference Intakes for Adults, by Life Stage Objectives Calcium Vitamin D • To review current guidelines for intake of calcium and Tolerable Tolerable vitamin D in midlife women. Life Stage (gender) RDA upper intake RDA upper intake (mg/d) level (mg/d)* (IU/d) level (IU/d)* • To summarize the evidence on calcium/vitamin D and the 19-50 yr (men and women) 1,000 2,500 600 4,000 risk of fractures, falls, cardiovascular disease, cancer, and 51-70 yr (men) 1,000 2,000 600 4,000 all-cause mortality. 51-70 yr (women) 1,200 2,000 600 4,000 • To present an update on the status of ongoing randomized 71+ yr (men and women) 1,200 2,000 800 4,000 trials of vitamin D nationally and internationally. RDA = Recommended Dietary Allowance *The tolerable upper intake level is the threshold above which is a risk of adverse events. Source: Ross AC, Manson JE, Abrams SA, et al. J Clin Endocrinol Metab 2011; 96(1):53. 1
Osteoporosis : Public Health Impact WHI Calcium/Vitamin D (Ca/D) Trial Design: Double Blind • At age 50, lifetime risk of fracture is N=36,282 women Intervention • 1:2 women (CaD supplement) • 1:5 men • 1000 mg elemental calcium as (50%) calcium carbonate and 400 IU • Affects 10 million Americans vitamin D 3 Randomization • 8 million women • 2 million men (50%) Control • 2 million fractures yearly (Placebo) (more common in women than MI, stroke, and breast cancer combined) NOF Fast Facts, www.nof.org Burge R, et al. J Bone Miner Res 2007; 22:465-475. Calcium/Vitamin D Supplementation and Bone Mineral Density Results Risk of Hip Fracture: WHI 20 Ca/D Group Greater preservation in total hip BMD N = 199 Placebo Group Rate of Hip Fracture N = 175 Average differences between CaD and placebo groups: (Cases/10,000/Yr) 15 HR = 0.88 • 0.59% at year 3 (95% CI, 0.72-1.08) 10 P = 0.23 • 0.86% at year 6 (n=374 cases) 5 • 1.01% at year 9 0 Ca/D Group Placebo Group Source: Jackson RD, et al. NEJM 2006; 354:669-83. Source: Jackson RD, et al. NEJM 2006; 354:669-83. 2
Calcium/Vitamin D and Risk of Hip Fracture, Stratified by Additional Fracture Findings Baseline Intake of Supplemental and Dietary Calcium 2.0 Hip Fracture – Adherent Women • 29% fewer hip fractures in CaD 0.005 0.010 0.015 0.020 0.025 1.8 than placebo (HR 0.71; 95% CI CaD Cumulative Hazard 1.5 0.52-0.97) in adherent women Placebo 1.3 (>80% of study pills) Hazard Ratio 1.22 HR = 0.71 1.0 (95% CI, 0.52-0.97) • 21% fewer hip fractures among P-value = 0.03 0.87 0.8 women ≥ 60 years 0.70 (HR 0.79; 95% CI 0.64-0.98; p for 0.5 * interaction by age = 0.05) Time (years) 0.3 0.0 * p <0.05 0 1 2 3 4 5 6 7 8 0.0 Nonusers <500 mg/d 500+ mg/d Baseline Use of Calcium Supplements Source: Jackson RD, et al. NEJM 2006; 354:669-83. Source: Jackson RD, et al. NEJM 2006; 354:669-83. Calcium/Vitamin D and Fractures: Randomized Trials National Osteoporosis Foundation: Meta-Analysis of Calcium/D Studies DIPART Meta-analysis (n=68,500 pts; 7 trials) All Fractures • Any Fracture All Trials 0.95 (0.90, 1.00) Ca+ D Trials 0.92 (0.86, 0.99) D alone Trials 1.01 (0.92, 1.12) • Hip Fracture Hip Fractures All Trials 0.97 (0.86, 1.10) Ca+ D Trials 0.84 (0.70, 1.01) D alone Trials 1.09 (0.92, 1.29) *No vitamin D dose effect comparing 400 IU and 800 IU.* The DIPART Group. BMJ 2010; 340:b5463. Source: Weaver CM, et al. Osteoporos Int 2016; 27:367-376. 3
Dietary Calcium Intake and Health Outcomes WHI Calcium/D Trial (2006) Primary Endpoints HR (95% CI) Australian cohort age 40-69 Hip fracture 0.88 (0.72,1.08) Recruited 1990-1994 Adherent 0.71 (0.52,0.97) 12 years follow-up Secondary Endpoints HR (95% CI) Dietary Calcium Colorectal cancer 1.08 (0.86,1.34) Breast cancer 0.96 (0.85,1.09) Q1 473 mg/d All cancers 0.98 (0.90,1.05) Q2 686 mg/d Stroke 0.95 (0.82,1.10) Q3 903 mg/d MI or CHD death 1.04 (0.92,1.18) Q4 1348 mg/d Total mortality 0.91 (0.83,1.01) Source: Jackson RD, et al. NEJM 2006; 354:669-83. Source: Khan B, et al. J Bone Miner Res 2015; 30:1758-1766. Effect of Calcium/D on CVD Events: Based on Data from Two RCT of Ca/D What Are Skeletal Health Indicators for Vitamin D? and the WHI Ca/D Study Participants Not Taking Personal Calcium Supplements at Baseline Conceptualization of integrated bone health outcomes and vitamin D exposure Source: IOM: DRIs for calcium and vitamin D. National Academies Press, 2011. Source: Bolland MJ, et al. BMJ 2011:342:d2040. 4
Risk Factors for Low Vitamin D Levels Vitamin D and Risk of Falling • Older age Meta-Analysis Living in the North • Avoidance of sun • Dark skin pigmentation • Obesity • 31% decrease Low intake • in fall risk Genetic factors • Various medical conditions • Source: Bischoff-Ferrari HA, et al. JAMA 2004;291:1999-2006. Meta-Analysis of Vitamin D Supplementation and CVD: Institute of Medicine (IOM) Committee’s Conclusion Secondary Analyses from Randomized Clinical Trials on Vitamin D and CVD, Cancer, and Other Nonskeletal Outcomes 51 eligible trials: Endpoint HR (95% CI) P-Value Evidence for an association with nonskeletal outcomes is: Myocardial Infarction 1.02 (0.93-1.13) 0.64 • Inconsistent. Stroke 1.05 (0.88-1.25) 0.59 • Inconclusive as to causality. All-Cause Mortality 0.96 (0.93-1.00) 0.08 • Not yet sufficient to inform dietary guidelines. No significant changes in lipids, glucose, BP (systolic or diastolic). Source: IOM: DRIs for Calcium and Vitamin D, National Academies Press, 2011. Source: Elamin MB, et al. JCEM 2011; 96:1931-42. 5
Potential Sources of Confounding in the Relationship between Serum 25(OH) Vitamin D and Health Outcomes Poor Nutrition: Low Low Sun Exposure Dietary Intake of Vitamin D Low 25(OH)D Obesity Low Physical Activity ? CVD, type 2 diabetes, and cancer Source: Powe CE, et al. N Engl J Med 2013; 369:1991-2000. Ongoing Large-Scale Randomized Trials (N ≥ 10,000) of Vitamin D Supplementation Worldwide* Vitamin D Potential Indicators for Excess Intake T rial Sample Age Treatment Vitamin D Primary Location Size+ Range Duration Intervention Endpoints • Hypercalcemia; hypercalciuria VITamin D and 25,874 ≥ 50 M 5 yrs 2000 IU/d Cancer; OmegA-3 TriaL ≥ 55 F (oral) CVD (VITAL) USA • Emerging evidence for all-cause mortality, cancer, D-Health 20,000 ≥ 60 5 yrs 60,000 IU/ Total CVD, falls and fractures at high exposures Australia month; mortality; (oral) cancer Vitamin D and 20,000 ≥ 65 5 yrs 100,000 IU/ Total Longevity month (oral) mortality; (VIDAL) UK# cancer *Several moderate-size randomized trials (2,000 - <10,000 participants) also are in progress in the US and worldwide. #In pilot phase. CVD denoted cardiovascular disease. 6
The VIT amin D and Omeg A -3 Tria L ( VITAL ): Design Acknowledgements 25,874 Initially Healthy Men and Women (Men >50 yrs; Women >55 yrs) Jane Cauley, DrPH Nelson Watts, MD Vitamin D 3 Placebo (2000 IU/d); N=12,937 N=12,937 Rebecca Jackson, MD Philomena Quinn EPA+DHA Placebo EPA+DHA Placebo Researchers, staff, participants (1 gm/d); N=6469 N=6468 (1 gm/d); N=6468 N=6469 in these studies Mean Treatment Period = 5.0 years Many others 5107 African Americans Blood collection in ~16,953, follow-up bloods in ~6000 Primary Outcomes: Cancer (total) and CVD (MI, stroke, CVD death) Adapted from: Manson JE, Bassuk SS, Lee I-M, et al. Cont Clinical Trials, 2011. Calcium and Vitamin D Summary • Adequate calcium and vitamin D (along with weight-bearing exercise) are necessary for optimal bone health. • Total calcium intake of 1200 mg/d is recommended in midlife women; supplementation >1000 mg/d is rarely needed. • Vitamin D 1000-2000 IU/d is reasonable supplement for most midlife women. • For higher-risk patients, measure 25-OH D, with a target blood level ≥ 30 ng/dl (75 nmol/L). • More is not necessarily better! Thank you! 7
Recommend
More recommend