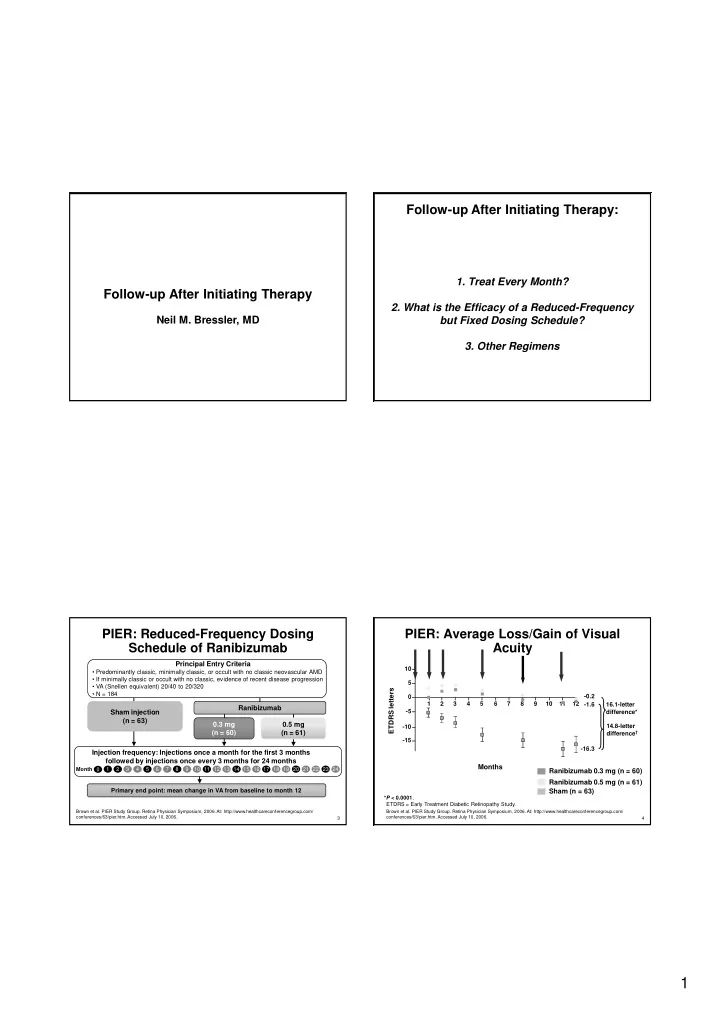
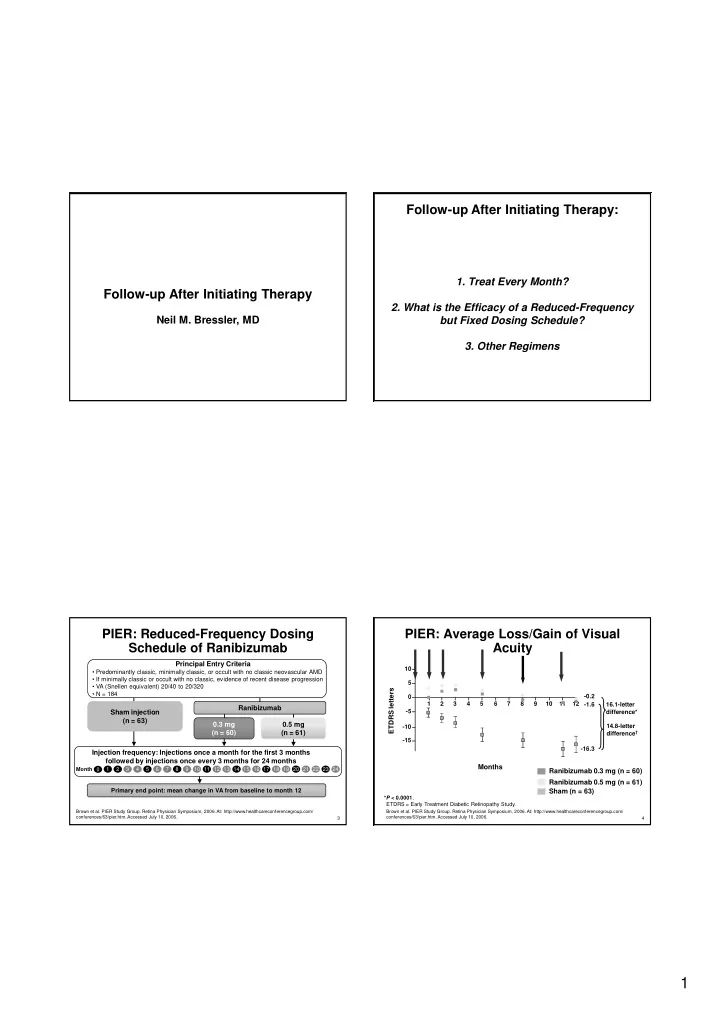
Follow-up After Initiating Therapy: 1. Treat Every Month? Follow-up After Initiating Therapy 2. What is the Efficacy of a Reduced-Frequency Neil M. Bressler, MD but Fixed Dosing Schedule? 3. Other Regimens PIER: Reduced-Frequency Dosing PIER: Average Loss/Gain of Visual Schedule of Ranibizumab Acuity Principal Entry Criteria 10 • Predominantly classic, minimally classic, or occult with no classic neovascular AMD • If minimally classic or occult with no classic, evidence of recent disease progression 5 • VA (Snellen equivalent) 20/40 to 20/320 ETDRS letters • N = 184 0 -0.2 1 2 3 4 5 6 7 8 9 10 11 12 -1.6 16.1-letter Ranibizumab -5 Sham injection difference* (n = 63) 0.3 mg 0.5 mg 14.8-letter -10 (n = 60) (n = 61) difference † -15 -16.3 Injection frequency: Injections once a month for the first 3 months followed by injections once every 3 months for 24 months Months Month 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 0 Ranibizumab 0.3 mg (n = 60) Ranibizumab 0.5 mg (n = 61) Primary end point: mean change in VA from baseline to month 12 Sham (n = 63) * P < 0.0001 . ETDRS = Early Treatment Diabetic Retinopathy Study. Brown et al. PIER Study Group. Retina Physician Symposium, 2006. At: http://www.healthcareconferencegroup.com/ Brown et al. PIER Study Group. Retina Physician Symposium, 2006. At: http://www.healthcareconferencegroup.com/ conferences/63/pier.htm. Accessed July 10, 2006. conferences/63/pier.htm. Accessed July 10, 2006. 3 4 1
PIER: ≥ 15-Letter Gain From Baseline PIER: Loss of < 15 Letters From Baseline at 12 Months at Month 12 * * 100 % of patients % of subjects 80 60 40 † 13% 12%* 20 10% Ranibizumab Ranibizumab Sham 0.3 mg 0.5 mg injection 0 (n = 60) (n = 61) (n = 63) Sham Ranibizumab Ranibizumab (n=63) 0.3 mg 0.5 mg * P < 0.0001 vs sham injection. (n=60) (n=61) Brown et al. PIER Study Group. Retina Physician Symposium, 2006. At: http://www.healthcareconferencegroup.com/ conferences/63/pier.htm. Accessed July 10, 2006. 5 6 *P =0.87; † P =0.71 vs sham. PIER: Adverse Events PIER: Conclusion 12 Month Data Adverse ocular events occurring more frequently Reduced-frequency dosing schedule with ranibizumab vs sham injection not serious reduced risk of vision loss but did not – Conjunctival hemorrhage increase chance of vision gain vs sham – Eye pain – Increased intraocular pressure Unknown if reduced frequency dosing No reported cases of endophthalmitis, serious schedule is inferior to monthly schedule intraocular inflammation, or other ocular serious without direct comparison of these adverse events treatment regimens No myocardial infarctions or cerebral vascular events were observed Brown et al. PIER Study Group. Retina Physician Symposium, 2006. Brown et al. PIER Study Group. Retina Physician Symposium, 2006. At: http://www.healthcareconferencegroup.com/ At: http://www.healthcareconferencegroup.com/conferences/63/pier.htm. Accessed July 10, 2006. conferences/63/pier.htm. Accessed July 10, 2006. 7 8 2
PIER: Mean Change in Dosing Intervals When Treating Central Foveal Thickness ( μ m) Neovascular AMD: 100 Mean (±SE) change from baseline in 75 Central fovea thickness ( μ m) 50 25 Monthly? Less Frequently? 0 -29 -25 Sham Total (n=40) Dependent on Imaging? -50 -75 -100 -123 0.5 mg ranibizumab (n=41) -125 0.3 mg ranibizumab (n=37) -126 -150 -175 1 2 3 5 8 12 Month 9 LOCF was used for missing data. No OCT scans in Year 2. 10 PIER: Average Loss/Gain of Visual Acuity PIER: Average Loss/Gain of Mean Change in Central Foveal Thickness ( μ m) Visual Acuity 10 100 100 5 75 75 Mean (±SE) change from baseline in ETDRS letters 10 Central fovea thickness ( ?m) 50 50 0 -0.2 5 25 25 ETDRS letters 1 2 3 4 5 6 7 8 9 10 11 12 -1.6 16.1-letter -0.2 0 0 0 1 2 3 4 5 6 7 8 9 10 11 12 -1.6 16.1-letter -5 -25 -25 -29 -29 difference* Sham Total (n=40) -5 difference* -50 -50 -10 14.8-letter -75 -75 difference † -10 14.8-letter -15 -100 -100 -123 -123 difference † -16.3 0.5 mg ranibizumab (n=41) -125 -125 -126 -126 0.3 mg ranibizumab (n=37) -15 -150 -150 Months Ranibizumab 0.3 mg (n = 60) -16.3 -175 -175 1 1 2 2 3 3 5 5 8 8 12 12 Ranibizumab 0.5 mg (n = 61) Month Month Sham (n = 63) * P < 0.0001 . ETDRS = Early Treatment Diabetic Retinopathy Study. Months LOCF was used for missing data. No OCT scans in Year 2. Brown et al. PIER Study Group. Retina Physician Symposium, 2006. At: http:// www.healthcareconferencegroup.com / Ranibizumab 0.3 mg (n = 60) conferences/63/pier.htm. Accessed July 10, 2006. Ranibizumab 0.5 mg (n = 61) Sham (n = 63) * P < 0.0001 . ETDRS = Early Treatment Diabetic Retinopathy Study. Brown et al. PIER Study Group. Retina Physician Symposium, 2006 At: http://www.healthcareconferencegroup.com/conferences/63/pier.htm. Accessed July 10, 2006. 11 12 3
Other Questions When Considering Management of Patient and Physician Treatment Based on Imaging Expectations of AMD Therapy Likelihood of at least moderate vision What about results for 40 subjects in improvement with treatment → not a majority PrONTO? – unknown if results are non-inferior to at this time monthly or PIER regimen, several rules used to determine additional treatment Likelihood of at least moderate vision (regular OCTs, periodic FA, VA, improvement without treatment → rare combination of attributes) Risk of moderate or severe vision loss with treatment → rare but not zero What about fluorescein angiography? – case series show new fluorescein leakage in absence of detection of new Risk of moderate or severe vision loss without thickening or subretinal fluid on OCT treatment → common 13 14 Management of Patient and Physician Empiric Use of Bevacizumab in AMD: Expectations of AMD Therapy Safety Considerations Serious injection- related risks → rare, but Safety and efficacy in AMD not evaluated in randomized clinical trial setting, so strength of not zero evidence weaker than ranibizumab 1-5 Other injection- related risks → common No long-term follow-up has been reported Rare systemic or other long term risks → Systemic side effects in patients with colon unknown cancer include gastrointestinal perforations, hemorrhage, thromboembolic events, Need for multiple treatments if CNV treatment hypertension, and proteinuria 6 initiated with unknown date of completion of – Unknown relationship to intravitreal treatments injections Costs vs benefit 1. Rich et al. Retina . 2006;26:495; 2. Avery et al. Ophthalmology . 2006;113:363; 3. Spaide et al. Retina . 2006;26:383. 15 16 4. Yoganathon et al Retina; 2006:26:994; 5. Shahar et al. Retina . 2006;26:262; 6. Avastin (bevacizumab) PI. 4
Empiric Use of Bevacizumab in AMD: Does Anyone Know if Bevacizumab is Non-Inferior to Ranibizumab? Safety Considerations What is a Non-Inferiority Trial? (EMEA, 27 July 2005) However, clinical case series suggest that short Pre-specify/SET a margin of non-inferiority (delta) in term effects seem similar to ranibizumab and the protocol. superior to PDT or pegaptanib What difference in outcome are you willing to give up- and accept as non-inferior? Unknown if bevacizumab is almost as good as (non-inferior to) ranibizumab, somewhat worse, or – The choice of the delta must be justified on clinical and somewhat better for efficacy or safety statistical grounds. – It always needs to be tailored specifically to the particular New challenge: should we use ranibizumab or clinical context and no rule can be provided that covers all bevacizumab if both are available and no economic clinical situations. difference to patient 17 18 Challenges for Non-inferiority Studies Does Anyone Know if Bevacizumab is Non-Inferior to Ranibizumab? Testing of the new drug (eg, bevacizumab) What is a Non-Inferiority Trial? would need to mirror the original testing of the (EMEA, 27 July 2005) Standard drug (eg ranibizumab) – Trial endpoint, design, subject population Run the study, construct a 2-sided 95% Constancy is required to try and ensure new confidence interval for the true difference trial outcome of standard treatment is similar to between the agents. outcome in original study – If ranibizumab outcomes in non-inferiority The interval must lie entirely on the positive study are not like ranibizumab outcomes in MARINA and ANCHOR, then you may be side of the non-inferiority margin. sacrificing even more efficacy than you were willing to when you set your margin. 19 20 5
Recommend
More recommend