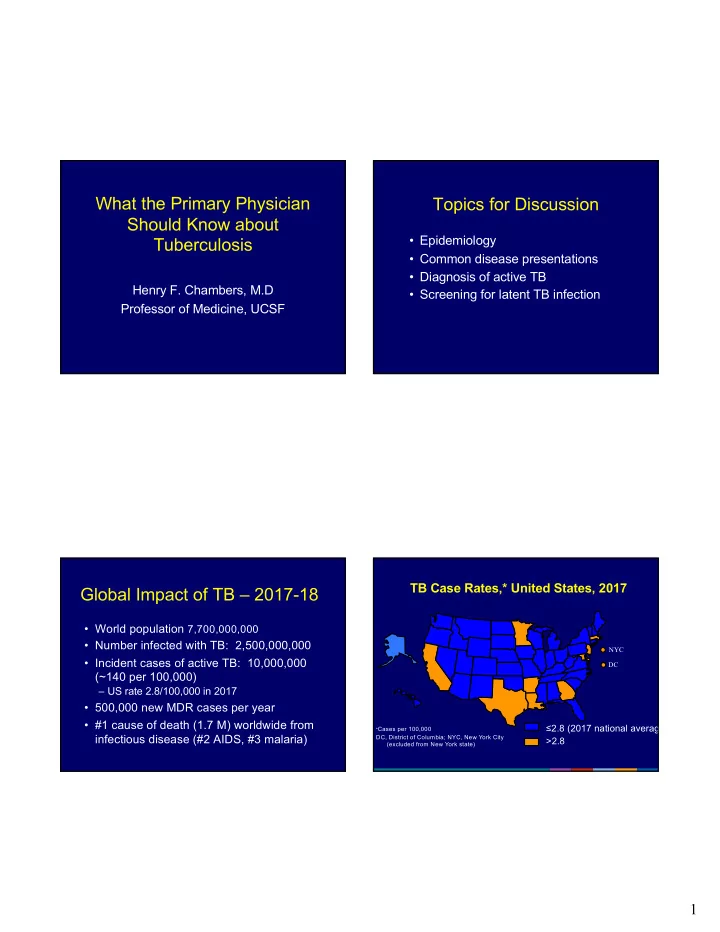
What the Primary Physician Topics for Discussion Should Know about • Epidemiology Tuberculosis • Common disease presentations • Diagnosis of active TB Henry F. Chambers, M.D • Screening for latent TB infection Professor of Medicine, UCSF TB Case Rates,* United States, 2017 Global Impact of TB – 2017-18 • World population 7,700,000,000 • Number infected with TB: 2,500,000,000 NYC • Incident cases of active TB: 10,000,000 DC (~140 per 100,000) – US rate 2.8/100,000 in 2017 • 500,000 new MDR cases per year • #1 cause of death (1.7 M) worldwide from ≤2.8 (2017 national average) * Cases per 100,000 infectious disease (#2 AIDS, #3 malaria) DC, District of Columbia; NYC, New York City >2.8 (excluded from New York state) 1
TB Cases and Rates Among U.S.-Born versus Demographic Groups with Non-U.S.–Born Persons, United States, 1993– 2017 Higher Rates of TB 30,000 40 U.S.-born Cases 35 Cases per 100,000 Non-U.S.–born Cases 25,000 • Foreign-born other than Western Europe 30 U.S.-born Rate No. of cases 20,000 Non-U.S.–born Rate 25 • Incarcerated persons 15,000 20 • Homeless, marginally housed 15 10,000 • HIV positive 10 5,000 5 0 0 1993 1995 1997 1999 2001 2003 2005 2007 2009 2011 2013 2015 2017 Year Case Presentation Active Tuberculosis • 63 y/o inmate transferred from jail for r/o TB • No fever, cough, weight loss • Pulmonary tuberculosis: 85% of all cases • 12 mm + PPD, HIV negative • The infectious form of the disease • Prior work-up • Clinical suspicion based on – 2/2007: AFB smear/culture neg x3 – 4/2011: AFB smear/culture neg x3 – Signs, symptoms, setting – 8/2011: AFB smear/culture neg x3 – Chest x-ray – 3/2016: AFB smear/culture neg x1 – 9/2016: AFB smear/culture neg x4 2
What is your estimate of the likelihood of active TB in this case? 1. 75% or higher 2. 50-75% 3. 25-50% 4. 5-25% 5. < 5% CXR: LUL nodular infiltrate, slight volume loss, maybe slightly worse since prior film Work-Up What is your revised estimate of the likelihood of active TB in this case? • CXR: LUL nodular infiltrate, slight 1. 75% or higher volume loss, maybe slightly worse since 2. 50-75% prior film? 3. 25-50% • Sputum examination 4. 5-25% – Routine: OF on culture and Gram-stain – AFB x2 and BAL x1: no AFB 5. < 5% – GenProbe Amplified MTD test: negative 3
Diagnosis of TB Xpert MTB/RIF Test Performance – Performance of Diagnostic Tests Pulmonary TB for Pulmonary TB Sensitivity Specificity Sensitivity Specificity Smear pos. TB 95-98% AFB smear 60% 99% 99% NAAT* 85% 99% Smear neg. TB* 70-90% Culture 90% 99% Rifampin “R” 98-99% 99-100% PPD (or QTF) 60% 10% * Lower value for single specimen, higher for 3 specimens *NAAT = Nucleic Acid Amplification Test 4
When to Use NAAT for TB Diagnosis in Addition to Culture Organism Burden in TB Suspected pulmonary tuberculosis 10 6 - 10 7 cfu/g Cavitary TB Suspected tuberculous lymphadenitis 10 4 - 10 5 cfu/g Pulmonary infiltrate Suspected tuberculous meningitis 10 2 - 10 4 cfu/g Lymphadenopathy Children (nasophyngeal aspirate) Performance of NAAT for Diagnosis of Pulmonary TB Detection Thresholds of Tests Pre-test PPV NPV for TB Diagnosis probability 90% 100% 43% 10 4 - 10 5 cfu/ml Positive smear 75% 98% 69% 10 1 - 10 2 cfu/ml Positive NAAT 50% 96% 87% 10 1 cfu/ml Positive culture 25% 91% 95% 5% 57% 99% 5
Clinical Course • Patient was discharged back to jail • Treatment for tuberculosis withheld Extrapulmonary TB pending results of work-up • 16 days after discharge, one sputum culture and the BAL specimen were reported positive for Mtb! Sites of TB Infection 120 100 Extrapulmonar y Pulmonary 80 Other Percent Bone/jt 60 Miliar y 40 GU Pleural 20 Lymphatic 0 All cases Expul 6
Differential Dx of Cervical Adenitis • Tuberculosis • Non-tuberculous mycobacterial infection • Kikuchi-Fujimoto’s syndrome (histiocytic necrotizing lymphadenitis) • Staph or strep infection • Cat scratch • Lymphoma, other malignancy • Other: syphilis, HIV, tularemia, listeria, plague Tuberculous Adenitis Work-up of Suspected TB Adenitis • Tuberculin test • Clinically presentation not distinctive • Check HIV serology • Constitutional symptoms not usually present • Chest x-ray to r/o pulmonary • Seen in children, young adults > adults • Get tissue for histopathology, culture, and • PPD + in 75-80% NAAT • Chest x-ray abnormality (15-20%) favors MTB 7
Performance of NAAT for Diagnosis of TB Adenitis Extrapulmonary TB • Tissue is the issue Sensitivity Specificity – to exclude other etiologies Lymphadenitis 90% 92% – for sensitivity testing • FNA Meningitis 53% 100% – Characteristic granulomas in 80% – Culture + in 40-70% Pleural 30% 100% – Smear + < 50% Peritoneal 32% 100% • Biopsy: partial vs. total excision Tedesse, et al. Clin Microbiol Infect 2018 Dec 21. Cochrane Data base Syst Rev. 2018 Aug 27;8:CD012768 When to Use NAAT for TB Treatment of TB Cervical Adenitis Diagnosis in Addition to Culture • Responsive to medical therapy alone • If excisional surgery performed, Suspected pulmonary tuberculosis medical therapy still must be given Suspected tuberculous lymphadenitis • Paradoxical “worsening” can occur; Suspected tuberculous meningitis needle aspiration effective Children (nasophyngeal aspirate) management • Sinus track formation, non-healing wounds may benefit from surgery 8
Principles of Therapy Similar Scenario for TB Pleuritis • Unilateral, benign, lymphocytic effusion • Start 4 drugs (RIPE) for suspected active TB • Primary infection, newly + PPD • Never use a single drug for treating active TB: resistance can emerge (1 mutant in 10 4 to 10 6 ) • Fluid usually smear and culture • Never add a single drug to a failing regimen negative (NAAT insensitive) • Consult and expert and/or local health • Pleural biopsy culture positive ~60%, department with granulomas ~80% • Francis Curry National TB Center: • Treat as for adenitis or pulmonary TB http://www.nationaltbcenter.edu/ Case Presentation • LV is a 58 y/o female from Ukraine referred for treatment of hypertension Screening for Latent TB and diabetes Infection (LTBI) • She is otherwise well • She gives a history of BCG vaccination as a teen 9
What is the best course of action? Who Should Be Screened? 1. The patient should be screened for LTBI with a tuberculin test 2. The patient should not be screened for LTBI • Persons likely to have TB infection because she is not a candidate for INH • Persons with increased risk of progression prophylaxis due to her age 3. The patient should not be screened because with • Not the general population prior BCG vaccination the tuberculin test will be false positive 4. The patient should be screened for LTBI by chest x-ray Increased Risk of Progression Increased Risk of Infection • Children < 5 years old • Recent contacts of an active TB case • Recent infection (contacts and converters) – About 30% are infected • HIV+ • Foreign-born persons from high TB • Prior TB prevalence areas – Asia, Mexico, Middle East, Central and South • Various medical conditions: America, Africa, Eastern Europe – Diabetes, hematologic/reticuloendotheial diseases, • Medically underserved, low-income, racial intestinal or gastric bypass, renal dialysis and ethnic minorities – Malabsorption syndromes, malnutrition, silicosis, alcoholism, smokers • Others: HCW, residents of congregate living – Immunosuppression, anti-TNF agents settings – > 15 mg prednisone QD for > 3 wks 10
Flowchart: Evaluation and Treatment of LTBI Risk of Progression TB Risk? STOP No Yes Risk Factor Increase in risk (+TST) Tuberculin Test + symptom review AIDS/Advanced HIV 9.9 Negative Positive Anti-TNF agent 7.9 Old TB, untreated 5.2 Chest x-ray Diabetes 3.1 Treatment not indicated Normal Abnormal Smoker 2.7 Underweight 1.6 Candidate for Rx R/o active TB of LTBI Reading the TST Diagnosis of LTBI • Measure reaction in 48 to 72 hours • Measure induration, not erythema • Record reaction in millimeters, not as “negative” or “positive” • Positive reactions can be read for up to 7 days TB Skin Test (TST) • Negative reactions can Interferon-gamma be read accurately for Release Assay (IGRA) only 72 hours 11
TST Positivity TST/IGRA Conversion • 5 mm + PPD • Signifies new infection – HIV, immunocompromised, contacts, abnl • > 10 mm increase within 2-year period CXR • 10 mm + PPD • Conversions may represent boosted reactions in some individuals – Those at increased risk of infection: IVDU, health care workers, foreign born, children < • IGRA result: prior negative, new 4 yo, high-risk medical conditions positive (no boosting) • 15 mm +PPD – Persons not at risk (why did you do the test?) Interferon-Gamma Release Assays LTBI Testing (IGRA) • TST should NOT be performed on someone • Indirect test for M. tuberculosis infection with a documented history of a positive test using whole blood • TST should be applied, read, and interpreted • Tests for generation of interferon-gamma by a trained health professional by cell-mediated immunity (not antibody) • RULE OUT active TB before treating for LTBI 12
Recommend
More recommend