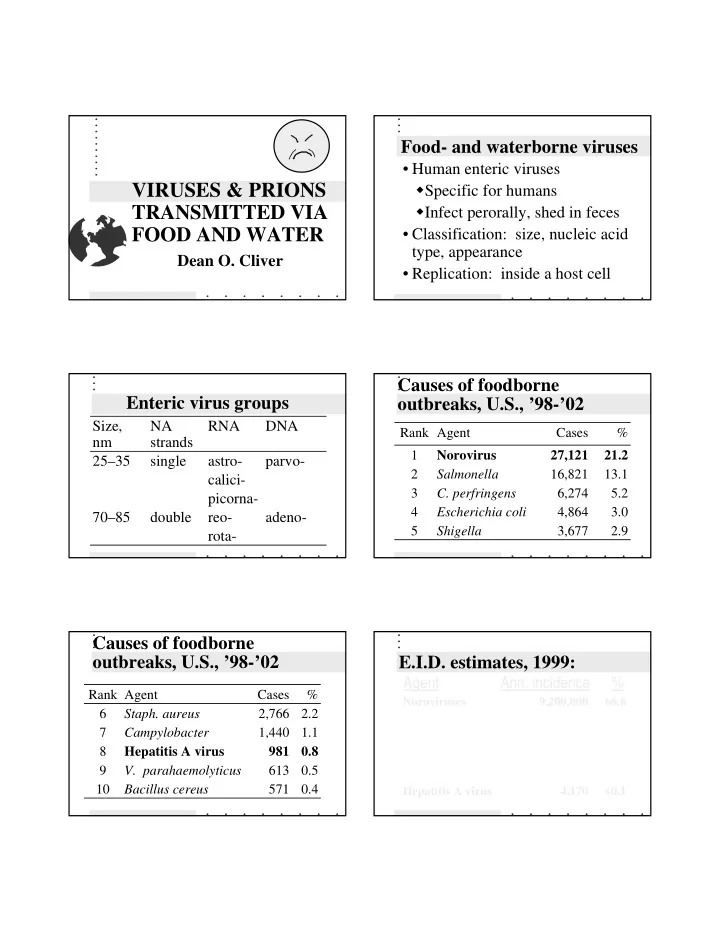
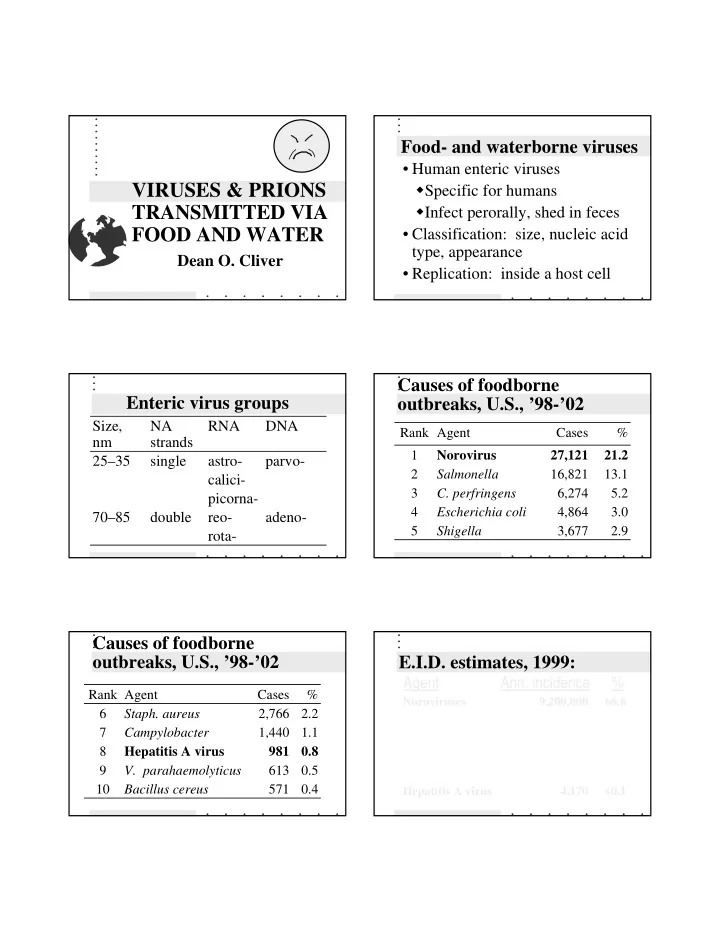
Food- and waterborne viruses • Human enteric viruses � Specific for humans VIRUSES & PRIONS � Infect perorally, shed in feces TRANSMITTED VIA FOOD AND WATER • Classification: size, nucleic acid type, appearance Dean O. Cliver • Replication: inside a host cell Causes of foodborne Enteric virus groups outbreaks, U.S., ’98-’02 Size, NA RNA DNA Rank Agent Cases % nm strands 1 Norovirus 27,121 21.2 25–35 single astro- parvo- 2 Salmonella 16,821 13.1 calici- 3 C. perfringens 6,274 5.2 picorna- 4 Escherichia coli 4,864 3.0 70–85 double reo- adeno- 5 3,677 2.9 Shigella rota- Causes of foodborne outbreaks, U.S., ’98-’02 E.I.D. estimates, 1999: Agent Ann. incidence % Rank Agent Cases % Noroviruses 9,200,000 66.6 6 2,766 2.2 Staph. aureus Campylobacter spp. 1,963,141 14.2 7 1,440 1.1 Campylobacter Salmonella spp. 1,341,873 9.7 8 Hepatitis A virus 981 0.8 Rotaviruses 39,000 0.3 9 V. parahaemolyticus 613 0.5 Astroviruses 39,000 0.3 10 Bacillus cereus 571 0.4 Hepatitis A virus 4,170 <0.1
Icosahedral symmetry RNA virus replication: virus cytoplasm nucleus cell membrane RNA virus replication (2): RNA virus replication (3): cytoplasm cytoplasm nucleus nucleus cell cell membrane membrane RNA virus replication (4): RNA virus replication (5): cytoplasm cytoplasm + nucleus viral nucleus + viral peptide RNA cell membrane
RNA virus replication (6): RNA virus replication (7): coat proteins coat proteins + + nucleus nucleus – strand + RNA + RNA RNA virus replication (8): RNA virus replication (9): progeny progeny virus virus + + + + nucleus nucleus + + Norovirus RNA virus replication (10): lysis EPA
Noroviruses History and naming • Norwalk, Ohio, gastroenteritis • CDC outbreak, 1972 � (U.S., ’98–’02): 657 outbreaks, • Small round structured viruses 27,171 illnesses, 1 death (SRSV), “Norwalk-like” � est. 9.2 million foodborne/yr • Calicivirus group — small ( - 30 • CAST: 181,000 cases/year, 0 nm?), single-stranded RNA, deaths, $890 protein coat has “dimples” The disease The disease 92) • Virus from ill or convalescent • Severe diarrhea & vomiting — person, via feces or vomitus 12–60 hr (usually 24–48 hr), virus shedding up to 7 days • Colonization of intestines — incubation: 1–2 days • Antibody is not protective Diagnosis of noroviral gastroenteritis Transmission/Control • Clinical: vomiting & diarrhea, • Routes — person-to-person, or >18 hr incubation � via water • Virus in feces � “undercooked” shellfish (cf. HA) � Tests for particles or antigen � food handled by an infected � Tests for viral genome person • Antibody production (serogroups) • Prevention — sanitation, cooking
Estimated annual Hepatitis A virus hepatitis A • CDC: ~11,000 cases • CAST: � 4,800–35,000 cases � <14 deaths � $5030/case CDC Hepatitis A virus History • Picornavirus: • Viral hepatitis recognized ca. � ca. 28 nm diameter time of World War II � single (+) strand RNA • Fecal-oral transmission of � coat protein comprises 60 copies of “infectious hepatitis” (now each of four structural polypeptides hepatitis A) recognized much • Relatively resistant to heat and to later drying History (2) The disease • Virus in feces of infected person • 5–6 hepatitis viruses now • Entry via intestines known • Liver colonized • Only hepatitis A is known to be � Infected cells destroyed by transmitted via food and water host’s immune response in North America � Incubation 15–50 days (average 28–30)
The disease (2) Transmission/Control • Virus shed in feces 1–2 weeks • Routes — person-to-person, or via before onset water (drinking, irrigation?), “undercooked” shellfish, or food • Illness: fever, malaise, anorexia, handled by an infected person nausea, abdominal discomfort— jaundice (?) • Prevention — sanitation, cooking, vaccination (U.S., 1995) • Usually complete recovery after a few weeks, permanent immunity • Food as a vehicle — 5%? Events In Hepatitis A Virus Infection Other gastroenteritis viruses Clinical illness • Astroviruses — occasionally foodborne, some replicate in cell Infection ALT culture IgM IgG • Rotaviruses — more often infant Response Viremia diarrhea than foodborne disease • Adenoviruses — serotypes 40 & 41, HAV in stool not known to be foodborne • Coronaviruses — questionable cause of human diarrhea, foodborne once? 0 1 2 3 4 5 6 7 8 9 10 11 12 13 Week Rotaviruses Astroviruses EPA EPA
Adenoviruses Coronaviruses EPA EPA Detection & monitoring: Other viruses and food • Human enteroviruses (polioviruses, • Diagnosis, adapted coxsackieviruses, echoviruses) — rare in U.S. • Cell culture • Hepatitis E virus — water , food? � Cytopathic effects • Tick-borne encephalitis virus — � Plaques milk & milk products, Slovakia • “Non-problems” — hepatitis B, C, & D; herpes, HIV, hantavirus Poliovirus infection (CPE) Virus plaques
Detection of viruses in food RT-PCR of hepatitis A • Sample processing � liquefaction � clarification � concentration • Test methods � probes � RT-PCR � antigen capture “Indicators” “Male-specific” coliphages • Bacteria — fecal coliforms, Escherichia coli , etc. • Viruses — vaccine polioviruses • Phages — fecal origin, resemble human viruses (?) Preventing transmission Food vehicle
Shellfish as vehicles Water vehicle Digestive tract eaten Filter feeders Raw, or slightly cooked Protection from heat
Other food vehicles Prevention • Sanitation (handwashing) • Depuration of shellfish • Cooking & other means of inactivation Viruses are inert — Persist, or lose infectivity can’t multiply in food (“inactivation”) Cooking inactivates viruses Freezing preserves viruses
Some viruses are UV inactivates viruses inactivated by drying on surfaces or in water Chlorine inactivates viruses on surfaces or in water Now for something completely different: PRIONS! Transmissible spongiform encephalopathies (TSEs) Prions are • Low MW peptides found in CNS • Accumulation of abnormal & some other organs. prions in brain leads to • Normal folding depends on spongiform degeneration amino acid sequence. • All are fatal abnormal normal • Some are “contagious” prion prion (PrP Sc ) (PrP C )
Normal human prion protein Normal human prion folding Abnormal prion folding Normal PrP cycle < PrP C PrP Sc > nucleus PrP Sc in neuron Extracellular PrP Sc
“Old” TSEs “New” TSEs • Scrapie in sheep • Bovine spongiform encephalopathy (BSE) — “mad cow disease” • Creutzfeldt-Jakob disease (CJD), sporadic, etc., in humans, • Feline spongiform encephalopathy • Transmissible mink encephalopathy • New variant CJD (vCJD) in humans • Chronic wasting disease (deer, elk) BSE brain Prion “infection” re-configuration (bovine) contact abnormal normal (bovine) BSE in cattle, UK BSE in cattle, UK, 2 • April 1985 to December 2004, • Slaughter of affected herds 184,131 confirmed cases of BSE • Enormous research effort (3–5-yr incubation) • No BSE prions found in red • Control by not feeding rendered meat (voluntary muscle) or milk bovine meat-and-bone meal • Vertical transmission “unlikely” (MBM) to cattle — slow • Carcass disposal precautions enforcement
BSE in cattle elsewhere Mad cow? • Some cattle, much beef, and a lot of MBM exported from UK to other countries • Now ca. 30 countries have BSE (few thousand cases), all in Europe except Japan, Israel, Canada, & US, so far. Non-transmission by prion Inter-species transmission • Ca. 1994, TSE in cats (UK), (sheep no change including zoo species contact scrapie) • In 1995, ~CJD in young people, abnormal UK — “vCJD” (>10-yr normal incubation?) (human) • vCJD differs in more than age distribution of victims Non-transmission by prion Prion “cross-infection” no change contact re-configuration contact (bovine) (bovine) abnormal abnormal normal normal (canine) (human)
Recommend
More recommend