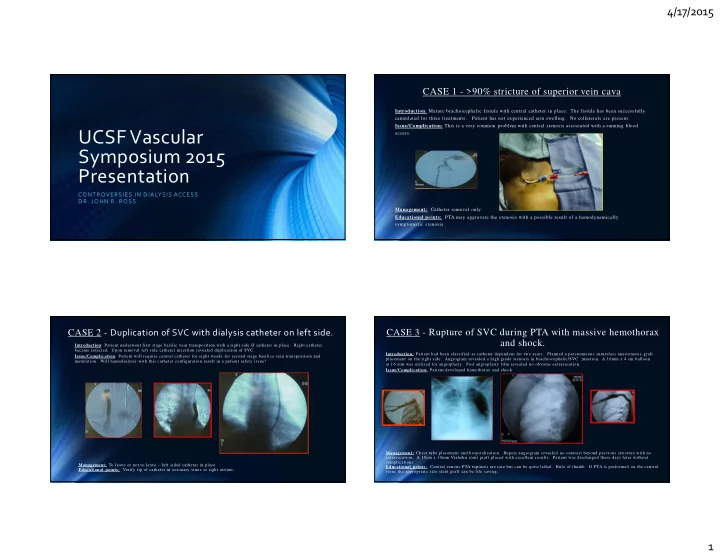
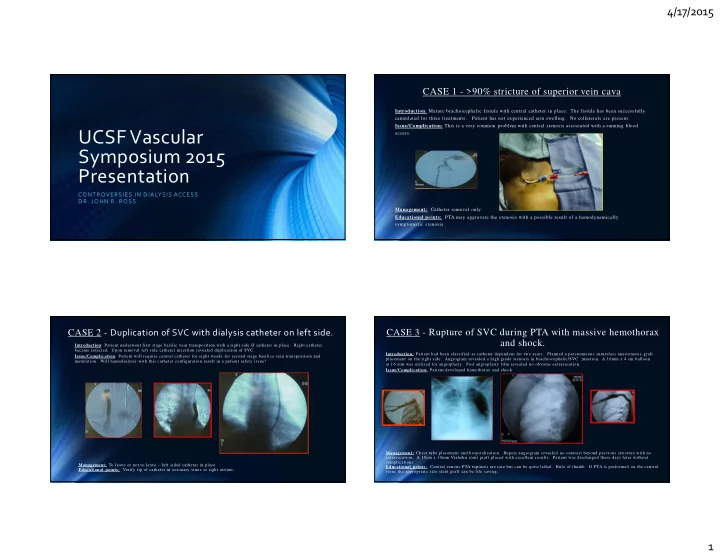
4/17/2015 CASE 1 - >90% stricture of superior vein cava Introduction : Mature brachiocephalic fistula with central catheter in place. The fistula has been successfully cannulated for three treatments. Patient has not experienced arm swelling. No collaterals are present. Issue/Complication: This is a very common problem with central stenosis associated with a running blood access. UCSF Vascular Symposium 2015 Presentation CONTROVERSIES IN DIALYSIS ACCESS DR. JOHN R. ROSS Management: Catheter removal only. Educational points: PTA may aggravate the stenosis with a possible result of a hemodynamically symptomatic stenosis. CASE 2 - Duplication of SVC with dialysis catheter on left side. CASE 3 - Rupture of SVC during PTA with massive hemothorax and shock. Introduction : Patient underwent first stage basilic vein transposition with a right side IJ catheter in place. Right catheter became infected. Upon removal left side catheter insertion revealed duplication of SVC. Introduction: Patient had been classified as catheter dependent for two years. Planned a percutaneous sutureless anastomosis graft Issue/Complication : Patient will require central catheter for eight weeks for second stage basilica vein transposition and placement on the right side. Angiogram revealed a high grade stenosis in brachiocephalic/SVC junction. A 10mm x 4 cm balloon maturation. Will hemodialysis with this catheter configuration result in a patient safety issue? at 16 atm was utilized for angioplasty. Post angioplasty film revealed no obvious extravasation. Issue/Complication: Patient developed hemothorax and shock. Management: Chest tube placement and hospitalization. Repeat angiogram revealed no contrast beyond previous stricture with no extravasation. A 10cm x 10mm Viabahn stent graft placed with excellent results. Patient was discharged three days later without complications. Management: To leave or not to leave – left sided catheter in place Educational points: Central venous PTA ruptures are rare but can be quite lethal. Rule of thumb: If PTA is performed on the central Educational points: Verify tip of catheter in coronary sinus or right atrium. veins the appropriate size stent graft can be life saving. 1
4/17/2015 CASE 5 - Ischemic hand with digit loss associated with CASE 4- Ischemic foot with thigh PTFE loop groin graft upper arm AV fistula Introduction : The patient had 6mm PTFE graft in place for three years without problems. Foot ischemia developed over a two Introduction : Patient had brachiocephalic fistula utilized for access for four years. Following use for 2 years a middle finger month time frame. Significantly the patient experienced a MI and beta blockers were initiated. Prior to the MI the systolic blood amputation was necessary for ischemic digit. Patient developed numbness in the hand x four weeks. Previous angiogram pressures were 160 to 180. Following treatment initiation with beta blockers the systolic blood pressures were 100-110. The revealed segmental occlusions of ulna and radial anastomosis. Symptoms improved. Follow-up angiogram 4 weeks later revealed patient also began Plavix therapy. Patient did have known total occlusion of the SVC. Patient has good sensation of foot. some recurrent stenoses of the forearm arteries requiring 4mm balloon PTA. Radial pulse could be augmented with occlusion of Issue/complication : Could the leg and thigh graft be salvaged? fistula which was not present prior to PTA. Technique Issue/Complication : Ischemic hand The 7mm x 5cm stent graft is placed in the central portion of the graft. A 3mm PTA balloon is placed in the center of the stent graft. With the balloon inflated to bust pressure a 2-0 tie is placed around the stent graft onto the balloon resulting in a 3mm stricture. The graft rarely clots with this technique but will frequently clot without the stent graft. Management : Aortogram with runoff performed and essentially negative for significant peripheral vascular disease. Severe steal syndrome present. Central graft banding performed with 7mm x 5cm Viabahn stent graft and 3mm PTA balloon. Educational points : Thigh graft ischemia is very difficult to manage. The central banding technique drops blood flow Management : DRIL procedure required after forearm runoff improved. substantially. The arterial needle is placed on the inflow part of the graft proximal to banding with venous needle distal to the Educational points : The DRIL (Distal revascularization with internal ligation) for ischemia coupled with distinct PTA resulted in banding. This allows for good dialysis with low flow in the graft. The parallel circuit will flow at the prescribed blood flow rate on the dialysis machine. functioning access and abatement of hand ischemia. With the ability to augment the pulse the DRIL procedure is very effective. CASE 6 - Expanding fistula aneurysm with thin skin CASE 7 - Cannulating deep AV Fistulae Introduction: Patient presented with a six year old brachialcephalic fistula with rapid increase in size of an aneurysm. Patient Introduction : Duplex of an eight week old fistula measures 8mm. Fistula is greater than 1.5cm deep with had a previous history of cephalic arch stenosis requiring repeated PTAs and placement of a 8mm x 10cm stent graft. Most recent exception of the the proximal 5 cm which was only 4mm deep. angiogram revealed a stenosis only at the outflow of the aneurysm. Issue/Complication : Issue/Complication : Repair of a true aneurysm with thin skin Options include using large PTA for BAM to give larger vein, elevate or transpose, or use button-hole technique on the proximal 5 cm. Management : Utilized button-hole technique. Management : Resection of the anterior portion of the aneurysm with the skin to section off the stricture area. Educational Points : With high flow fistulae (greater than 1000cc/min) no recirculation occurs with needles 3 to 5 cm. Educational points : Most aneurysms of fistulae are TRUE aneurysms. A simple anterior resection with a lateral repair and “tucking” apart. of the repair under the skin resolves the problem. 2
4/17/2015 CASE 8 - Second Stage basilic vein transposition planned CASE 9 - Long stricture in first stage basilic fistula Introduction : Patient presented for second stage basilic vein transposition. First stage in this thin patient was Introduction : Patient presented ten weeks status-post first stage BVT for planned performed approximately eight weeks prior to planned second stage procedure. Duplex revealed 8mm superficial second stage. Two prior BAM procedures up to 8mm PTA had been performed. Issue/Complication : Long high grade stricture in the axilla proximal fistula. Occlusion of the outflow reveals measurement of 11mm with a flow rate of 1400cc/min. Issue/Complication : Is second stage transposition needed or is there another option? Management : Placement of large 9 x 10mm stent graft in the stricture followed by Management : Forego second stage and utilize buttonhole technique for cannulation. transposition. Educational Points : If PTA fail with distal fistula stricture, stent grafts can be used if flow Educational Points : If the target for cannulation is good with high flow fistulae (any fistula), the buttonhole technique and size of proximal fistula are satisfactory. A upper graft can be done percutaneous later if should be utilized. necessary. CASE 10 – New Access Placement CASE 11 – Catheter Exchange Introduction : Patient presented for new access placement Patient’s history included three axillary access procedures on the left. Basilic vein transposition, cephalic fistula with drop down to axilla, and a prior exploration of axilla for graft ? Issue/Complication : Introduction : Catheter Exchange – Catheter has been in place for 2 months. Abandon thoughts of left access placement? Issue/Complication : Large right atrial clot. Management : Percutaneous sutureless venous anastomosis graft placement on the left. Management : Ekos Educational points : Using ultrasound the axillary vein is easily identified. A needle wire introducer placed with Educational Points : Can remove right atrial clot. angiograms. The brachial artery is exposed with tunneling of 6mm PTFE graft. The .035 wire ack loaded through the graft. 8 x 15 Viabahn stent graft is threaded over the wire through the graft to adequate outflow vein. 4 cm. of the Viabahn in the graft gives a sutureless anastomosis. A standard arterial anastomosis is then performed. 3
4/17/2015 CASE 12 – Ischemic Hand CASE 13 – Fibrin Sheath Introduction : 56 year old Caucasian female with past medical history of transplant surgery. Introduction : We have a fibrin sheath from the left PICC line before BVT. Presents a creatine level of 3 and symptoms of steal syndrome. Issue/Complication : Transpose or not to transpose managing of the fibrin sheath. Issue/Complication : Patient has creatinine level of 3 and has symptoms of steal syndrome. Management : Pull fibrin sheath out and resume access. Management : External Fistula Banding. Educational Points : You can still due a BVT after a fibrin sheath is found. Educational Points : Salvage fistula by banding. CASE 14 – What to do? Introduction : 56 year old Caucasian female with past medical history of transplant surgery presents a creatine level of 3 and has symptoms of steal syndrome. Issue/Complication : Failing transplant and failing fistula. Management : External balloon banding. Educational Points : Save hand and save fistula. 4
Recommend
More recommend