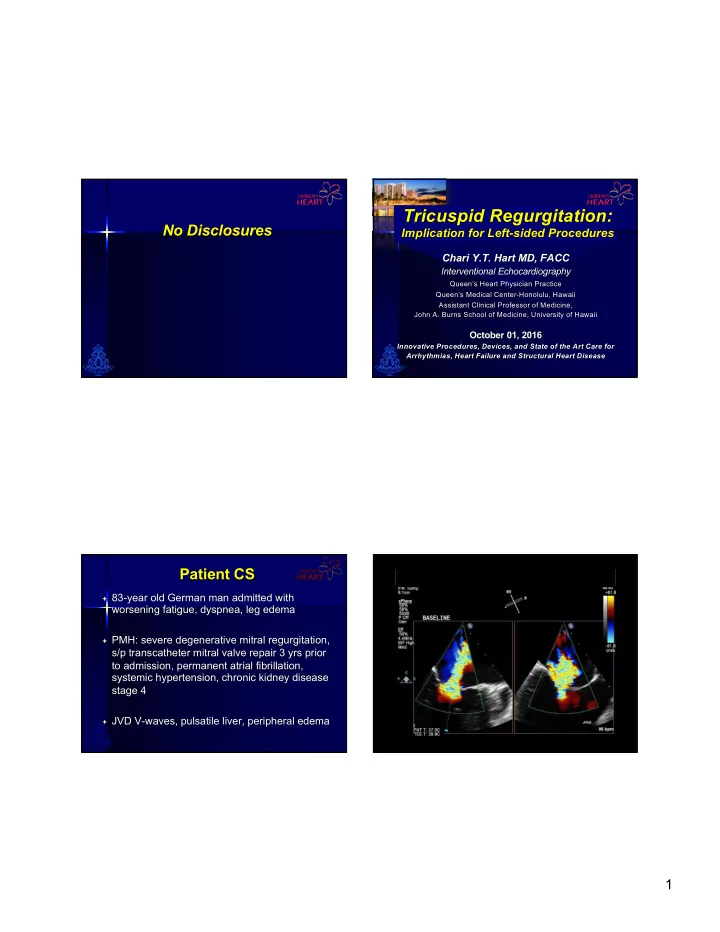
Tricuspid Regurgitation: No Disclosures Implication for Left-sided Procedures Chari Y.T. Hart MD, FACC Interventional Echocardiography Queen’s Heart Physician Practice Queen’s Medical Center-Honolulu, Hawaii Assistant Clinical Professor of Medicine, John A. Burns School of Medicine, University of Hawaii October 01, 2016 Innovative Procedures, Devices, and State of the Art Care for Arrhythmias, Heart Failure and Structural Heart Disease Patient CS ª 83-year old German man admitted with worsening fatigue, dyspnea, leg edema ª PMH: severe degenerative mitral regurgitation, s/p transcatheter mitral valve repair 3 yrs prior to admission, permanent atrial fibrillation, systemic hypertension, chronic kidney disease stage 4 ª JVD V-waves, pulsatile liver, peripheral edema 1
2
Apical 4-chamber view Subcostal view of Apical 2-chamber view dilated RV, RA; severe TR IVC, hepatic vein MitraClip, mild residual MR Parasternal LAX view systolic flow reversals Preserved LVEF, MitraClip, mild MR RV tissue Doppler Hepatic vein PW Doppler peak systolic velocity systolic flow reversals Mitral inflow diastolic MG 4 mmHg at 61 bpm Outline The Clinical Problem… ² Anatomy of the tricuspid valve ª Incidence of tricuspid regurgitation ² Primary versus secondary (functional) associated with left-sided valvular tricuspid regurgitation (TR) disease 8% to 35% of cases ² Pathophysiology of secondary tricuspid ª More common in mitral valve disease regurgitation ª Also in aortic valve disease ² Prognosis of tricuspid regurgitation ² Guideline indications for intervention of ª Tricuspid regurgitation is often clinically secondary tricuspid regurgitation silent, thus an “ignored” problem in left- ² Future non-surgical options for tricuspid sided disease regurgitation Jacovella G et al. Cardiol Prat 1971;22:235-41 King RM et al. Circulation 1984;70:1193-7 3
Tricuspid Valve Tricuspid Valve Anatomy Anatomy n 3 leaflets (septal, anterior, posterior) n Largest valve n The annulus n Area 4-6 cm2 n The chordae n Diam 27-29mm n The papillary n Inferior, anterior to muscles the MV n The adjacent n Saddle-shaped myocardium (atrial, ellipsoid becomes ventricular) planar & circular as it dilates (A-P) Dreyfus G.D., Corbi PJ, Chan KM, et al. Ann Thorac Surg 2005;79:127-32 Dreyfus G.D., Corbi PJ, Chan KM, et al. Ann Thorac Surg 2005;79:127-32 Pathophysiology of Tricuspid Tricuspid Regurgitation Regurgitation in Mitral Valve Disease Rheumatic Degenerative (myxomatous) RHD Ischemic DCM Primary Congenital (Ebstein’s, Left heart disease dysplasia, cleft, etc.) 20% •Left ventricular dysfunction Infective Endocarditis MS MR •Mitral or aortic valve disease Radiation Carcinoid Right ventricular dysfunction á Left atrial size á Left atrial pressure Blunt chest trauma •RV cardiomyopathy Iatrogenic trauma: •RV ischemia •RV biopsy •RV volume overload (ASD, Atrial fibrillation Pulmonary hypertension •RV PM or ICD leads APVR) Secondary Pulmonary Hypertension Tricuspid annulus Organic TV •Chronic lung disease RV dilatation dilatation “Functional” •Left to right shunt disease & dysfunction •Pulmonary (tethering of TV) thromboembolism 80% TRICUSPID REGURGITATION Right atrial abnormalities •Atrial fibrillation Shiran A, Sagie A. J Am Coll Cardiol 2009;53:401-8 4
Pathophysiology of Tricuspid Severe Tricuspid Regurgitation Regurgitation in Mitral Valve Disease Significant â exercise capacity (low output) Negative impact on long-term survival RHD Ischemic DCM 1.0 MS MR 0.8 á Left atrial size á Left atrial pressure 0.6 Surviving Atrial fibrillation Pulmonary hypertension 0.7 Tricuspid regurgitation None Tricuspid annulus Organic TV Mild RV dilatation 0.2 >5,000 patients dilatation Moderate disease & dysfunction (tethering of TV) Severe 0.0 1,000 1,200 1,400 0 200 400 600 800 TRICUSPID REGURGITATION Days Charles J. Bruce, and Heidi M. Connolly Circulation. 2009;119:2726-2734 Prognostic Implications of TR What do the Guidelines Say? in patients with VHD ª Moderate+ secondary TR, mean age 68+16 yrs ª Mean follow-up 43 + 24 mos: ª Deaths 13 (14%) ª Surgeries 12 (13%) ª Multivariate analysis, predictors of death: ª RVSP (p=0.0038) ª RVSP > 48 mmHg, associated with significantly increased mortality and decreased surgery-free survival ª Device implantation (p=0.0487) *TA dilation is defined by >40 mm on TTE (>21 mm/m 2 ) or Jhawar MB et al. J Heart Valve Dis 2013; 418-24 >70 mm on direct intraoperative J Am Coll Cardiol. 2014;63(22):2438-2488. doi:10.1016/j.jacc.2014.02.537 5
2014 AHA/ACC Valvular Heart Disease Guidelines 2014 AHA/ACC Valvular Heart Disease Guidelines Intervention Recommendations Intervention Recommendations for Tricuspid Regurgitation for Tricuspid Regurgitation Class I (…is recommended/indicated): Class IIa (…is reasonable/can be beneficial): ª Tricuspid valve surgery is recommended for patients with ª Tricuspid valve repair can be beneficial for patients with severe functional TR (stages C and D) undergoing left- mild, moderate or greater (stage B) at time of left-sided sided valve surgery. valve surgery with either 1) tricuspid annular dilatation* or 2) prior evidence of right heart failure. * Tricuspid annulus dilatation of >40mm diameter or 21 mm/m2 on preop TTE; >70mm direct intraop ª Tricuspid valve repair can be beneficial for patients with symptoms due to severe primary TR that are unresponsive to medical therapy J Am Coll Cardiol. 2014;63(22):2438-2488. doi:10.1016/j.jacc.2014.02.537 J Am Coll Cardiol. 2014;63(22):2438-2488. doi:10.1016/j.jacc.2014.02.537 2014 AHA/ACC Valvular Heart Disease Guidelines Multimodality Imaging in the Assessment of Tricuspid Intervention Recommendations Regurgitation and Right Ventricular Volumes and Function for Tricuspid Regurgitation Class IIb (…may be reasonable/may be beneficial): ª Tricuspid valve repair may be considered for asymptomatic or minimally symptomatic patients with severe primary TR (stage C) and progressive moderate or greater RV dilatation and/or systolic dysfunction. ª Tricuspid valve repair may be beneficial for patients with persistent symptoms due to severe TR (stage D) in patients who have undergone previous left-sided valve surgery and who do not have severe pulmonary hypertension or significant RV systolic dysfunction. Pilar Tornos Mas et al. Heart 2015;101:1840-1848 J Am Coll Cardiol. 2014;63(22):2438-2488. doi:10.1016/j.jacc.2014.02.537 6
Before left-sided valve surgery, careful Future Non-Surgical Options assessment of TR severity, tricuspid annulus measurement for Tricuspid Regurgitation TA diameter in 4-ch view septal-lateral dimension Josep Rodés-Cabau, MD, Rebecca T. Hahn, MD Azeem Latib, MD et al. J Am Coll Cardiol 2016;67:1829–45 Future Non-Surgical Options Future Non-Surgical Options for Tricuspid Regurgitation for Tricuspid Regurgitation Challenging Anatomy of the Tricuspid Valve for Challenging Anatomy of the Tricuspid Valve for Transcatheter Therapies Transcatheter Therapies n Large tricuspid annulus n Proximity of AV node, right n Large tricuspid annulus n Proximity of AV node, right His bundle branch n Nonplanar, elliptical His bundle branch n Nonplanar, elliptical n Proximity of the RCA to n Proximity of the RCA to n Fragile TA tissue, narrow n Fragile TA tissue, narrow annulus, risk of injury annulus, risk of injury annular shelf annular shelf n Risk of occlusion of n Risk of occlusion of n Noncalcified annulus n Noncalcified annulus coronary sinus, vena cava, coronary sinus, vena cava, n Angulation with SVC, IVC n Angulation with SVC, IVC outflow tract outflow tract n Trabeculated RV, mucular n Trabeculated RV, mucular n Slow-flow in RV n Slow-flow in RV bands, chordae bands, chordae n Pacemaker, ICD leads n Pacemaker, ICD leads n Thin RV free wall n Thin RV free wall Josep Rodés-Cabau, MD, Rebecca T. Hahn, MD Azeem Latib, MD et al. J Am Coll Cardiol 2016;67:1829–45 Josep Rodés-Cabau, MD, Rebecca T. Hahn, MD Azeem Latib, MD et al. J Am Coll Cardiol 2016;67:1829–45 7
Conclusions Future Non-Surgical Options for Tricuspid Regurgitation ª The tricuspid valve is COMPLEX Interventional Edge-to-Edge Repair with the ª The majority (80%) of tricuspid regurgitation is MitraClip system secondary (functional) ª Have R-E-S-P-E-C-T for tricuspid regurgitation secondary to left heart pathology, not automatically corrected ª Less emphasis on conservative treatment, importance of concomitant correction with left heart procedures ª Tricuspid annular dilatation is progressive, ‘prophylactic’ 3 patietnts wih severe, symptomatic n tricuspid regurgitation intervention should be considered, regardless of TR Feasibility, safety demonstrated n severity â ERO with 3D-TEE, á LV stroke n volume, â N-terminal proBNP, relief of ª Proactive approach to secondary tricuspid regurgitation clinical symptoms for right heart failure and its surgical/transcatheter correction Promising option for patients at n prohibitive surgical risk ª Improved long-term survival outcomes for patients Christoph Hammerstingl, Robert Schueler, Margarita Malasa et al. Eur Heart J. 2016 Mar 7;37(10):849-53 Ma Mahalo fo for y r your a r atten ttentio tion! 8
Recommend
More recommend