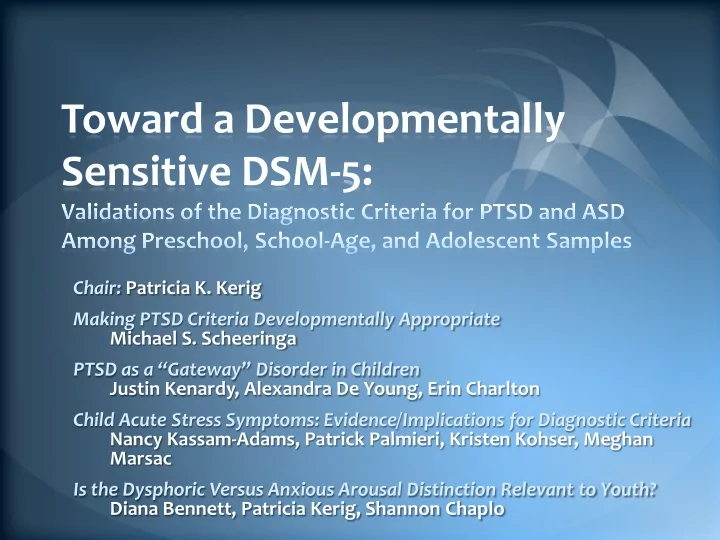
Toward a Developmentally Sensitive DSM-5: Chair: Patricia K. Kerig Making PTSD Criteria Developmentally Appropriate Michael S. Scheeringa PTSD as a “Gateway” Disorder in Children Justin Kenardy, Alexandra De Young, Erin Charlton Child Acute Stress Symptoms: Evidence/Implications for Diagnostic Criteria Nancy Kassam-Adams, Patrick Palmieri, Kristen Kohser, Meghan Marsac Is the Dysphoric Versus Anxious Arousal Distinction Relevant to Youth? Diana Bennett, Patricia Kerig, Shannon Chaplo
Making PTSD Criteria Developmentally Appropriate Michael Scheeringa, MD, MPH Remigio Gonzalez Professor of Child Psychiatry Tulane University New Orleans, LA November 2, 2012 mscheer@tulane.edu
Continuing Medical Education Commercial Disclosure Requirement I, Michael Scheeringa, have no commercial relationships to disclose. mscheer@tulane.edu
Preschool Challenges •Many PTSD symptoms are highly internalized. Difficult to observe. •Emerging verbal capacities. •Different developmental manifestations. Scheeringa MS (2011). Journal of Child & Adolescent Trauma 4:3, 181-197 mscheer@tulane.edu
PTSD-Alternative Algorithm (PTSD-AA) Recommendations for Preschool Children A. Exposed to traumatic event. (2) person’s response involved intense fear, helplessness, or horror. Note: In children, may be expressed by disorganized or agitated behavior. R ecommendation: Delete. B.(1) recurrent and intrusive distressing recollections of the event. Recommendation: “distress” not required. mscheer@tulane.edu
PTSD-AA recommendations C. Avoidance and numbing cluster: Recommendation: only 1 item instead of 3 required. C.(4) diminished interest in significant activities. Recommendation: …may be manifest in play, social interactions, and daily routines . C.(5) feeling of detachment or estrangement from others. Recommendation: Increased social withdrawal . D.(2) irritability or outbursts of anger Recommendation: …or extreme fussiness or temper tantrums. mscheer@tulane.edu
Face Validity for PTSD-AA Criteria Dx % by Dx % by # PTSD sx in DSM-IV alternative alternative dx Scheeringa et al 1995 n=12 13% 69% Not reported Scheeringa et al 2001 n=15 20% 60% 9.9 Levendosky et al 2002 n=62 3% 26% Not reported Ohmi et al 2002 n=32 0% 25% 6.1 Scheeringa et al 2003 n=62 0% 26% 6.1 Meiser-Stedman et al 2008 1.7% 10% 10.0 n=156 de Young et al 2012 n=130 5% 25% 6.4 for “misclassified” Scheeringa et al 2012 n=284 13% 45% 7.0 for “misclassified” mscheer@tulane.edu
New Data on Preschool: Study Design Recruitment different types of trauma groups: 1. Single Event - acute injuries. 2. Repeated Events – domestic violence. 3. Circumstances added a Hurricane Katrina group . • Goal: Compare different diagnostic criteria. Funded by National Institute of Mental Health (R01 MH 65884-01A1) Collaborators: Stacy Drury, Danny Pine, Frank Putnam, Charley Zeanah. Research assistants: Ruth Arnberger, Rociel Martinez, Sarah Watts, Tolanda Age, Cedar O’Donnell, Moira Flanagan, Emily Roser, Yolanda Steptore, Roneisha Alexander, Aleyda Diaz. mscheer@tulane.edu
Characteristics of 3 Trauma Groups Single Repeated Hurricane N 62 85 137 Age 5.2 yrs 5.1 yrs 5.1 yrs 82% a 62% b 62% b Race Black/A-A 11% b 18% b 28% a White Other 7% 20% 10% 12.4 yrs b 12.0 yrs b 13.7 a Mom education 23% b 7% a 34% b Father in home # types of event 1.0 1.7 1.4 # episodes 1.0 68.8 (median 9) 1.5 No differences between groups on mean Total, re-experiencing, avoidance/ numbing, or increased arousal PTSD symptoms. (Scheeringa et al., 2012) mscheer@tulane.edu
DSM-5 • Will include the first developmental subtype of a disorder in the history of the DSM: “Posttraumatic stress disorder in preschool children” • Incorporates all of the PTSD-AA recommendations in previous slides mscheer@tulane.edu
DSM-5 • One difference from PTSD-AA D.4. “Persistent reduction in expression of positive emotions.” mscheer@tulane.edu
DSM-5 “Under Consideration” Symptoms: DSM-5-UC • D.1. “Substantially increased frequency of negative emotional states – for example, fear, guilt, sadness, shame, or confusion.” • E.2. “Reckless or self-destructive behavior.” These are highly problematic: (1) overlap with existing PTSD symptoms, (2) developmental inappropriateness, and (3) overly internalized… Not to mention complete lack of empirical data. mscheer@tulane.edu
Misclassification Rates If DSM-IV Positive If DSM-IV Negative (n = 36) (n = 248) Other: Other Pos. Other Neg. Other Pos. Other Neg. PTSD-AA 100% 0% 37% 63% DSM-5 100% 0% 36% 64% DSM-5-UC 100% 0% 42% 58% mscheer@tulane.edu
Severity and Comorbidity PTSD Impaired Comorbid CBCL Total symptoms Domains Disorder DSM-IV 9.7 2.6 89% 70.6 PTSD-AA* 7.0 2.2 69% 61.1 DSM-5* 7.0 2.2 69% 61.1 DSM-5-UC* 7.4 2.1 67% 60.5 Note: Comorbid disorders = major depression, ADHD, oppositional defiant disorder, separation anxiety, specific phobia, social phobia, and generalized anxiety disorders. *For PTSD-AA, DSM-5, and DSM-5-UC, only misclassified cases used. mscheer@tulane.edu
What About 7-18 Years Youth? • 141 youth, 7-18 years, enrolled for a treatment study of CBT ± D-cycloserine. • Interviewed for PTSD with modified Diagnostic Interview Schedule for Children, parent and child versions. • Funded by U.S. National Institute of Mental Health (1RC1 MH088969-01) Collaborators: Judith Cohen, Danny Pine, Karin Mogg, Brendan Bradley, Carl Weems • Therapists: Emily Roser, Allison Staiger. • Assistants: Megan Kirkpatrick, Jennifer Liriano. mscheer@tulane.edu
No Differences Between Diagnostic Criteria Options with 13-18 Years Youth N=61 Diagnosed: Diagnosed: Number PTSD Number domains No Yes symptoms impaired DSM-IV 30% 70% 11.9 4.7 PTSD-AA 26% 74% * * DSM-5 31% 69% * * *Misclassified samples too small for meaningful means. mscheer@tulane.edu
Marked Differences Between Diagnostic Criteria Options with 7-12 Years Youth N=78 Diagnosed: Diagnosed: Number PTSD Number domains No Yes symptoms impaired DSM-IV 65% 35% 10.8 4.6 PTSD-AA 35% 65% 7.6* 4.0* DSM-5 46% 54% 7.8* 4.4* *Misclassified cases only mscheer@tulane.edu
Conclusions • Preschool children require separate diagnostic criteria. Will be in DSM-5. • Older (7-12 years) children may also need modified criteria. Poorly studied group. • Should lead to huge increases in diagnoses and access to treatment. mscheer@tulane.edu
PTSD AS A “GATEWAY” DISORDER IN CHILDREN JUSTIN KENA RD Y, A LEXA ND RA D E YO UNG , ERIN C HA RLTO N SC HO O L O F PSYC HO LO G Y, & C O NRO D , UNIV ERSITY O F Q UEENSLA ND , A USTRA LIA
COMORBIDITY AND PTSD-I • Adults • Up to 80% o f PT SD ha s c o mo rb id ity a t so me po int • De pre ssio n, Ge ne ra lize d Anxie ty Diso rd e r, Sub sta nc e Ab use • Co mo rb id ity va rie s o ve r time • Re la tio nship b e twe e n De pre ssio n a nd tra uma tic stre ss c ha ng e s o ve r time (O’ Do nne ll e t a l, 2004) • PT SD ma y b e c o nsta nt b ut no t a lwa ys a t a d ia g no stic le ve l Mc Mille n e t a l, 2002) • Co mo rb id ity ma y a lso b e pre mo rb id ity (K o e ne n e t a l 2008)
COMORBIDITY AND PTSD-II • Childre n • PT SD is und e r-re c o g nise d in c hild re n a nd this ma y in pa rt b e b e c a use c o mo rb id ity is e a sie r to re c o g nise • Also PT SD Dia g no stic Crite ria ma y b e ina ppro pria te (De Yo ung e t a l, 2011; Co he n & Sc he e ring a , 2010) • Co ntra ry to b e lie f, PT SD in c hild re n ma y b e le ss like ly to re mit with time (Sc he e ring a e t a l, 2005) • Within ra ng e o f 0-18 pre se nta tio n c a n c ha ng e • Re la tive ly mo re Sub sta nc e Ab use , De pre ssio n, in a d o le sc e nts • Mo re ADHD, ODD, Se pa ra tio n Anxie ty in yo ung c hild re n • Do the se c ha ng e o ve r time ? • Is PT SD a g a te wa y?
AIMS • T o do c ume nt pre va le nc e o f psyc ho lo g ic a l re a c tio ns in c hildre n a t 4 to 6 we e ks, a nd a g a in a t 6 mo nths fo llo wing tra uma tic injury. • T o e xa mine the re la tio nships b e twe e n po sttra uma tic stre ss a nd o the r psyc ho lo g ic a l re a c tio ns in c hildre n
METHOD – PARTICIPANTS STUDY 1 • Sa mple dra wn fro m Ro ya l Childre ns Ho spita l in Brisb a ne Austra lia • Admissio n to ho spita l • Ag e 1 – 6 ye a rs a t a dmissio n • All e xpe rie nc e d tra uma tic b urn injury • N=130 a dmissio ns • Asse sse d using Dia g no stic I nfa nt Pre sc ho o l Asse ssme nt (Sc he e ring a & Ha sle tt, 2010)
STUDY 1 PARTICIPANTS Patie nt Charac te ristic s Ma le 68 (52) F e ma le 62 (48) Ag e (ye a rs), M (SD) 2.70 (1.54) Burn type Sc a ld 53 (41) Co nta c t 51 (39) F ire / fla me s 13 (10) Che mic a l/ e le c tric a l 4 (3) F ric tio n 9 (7) Burn se ve rity % T BSAa , M (SD) 3.24 (4.30) Ho spita lise d 27 (21)
Recommend
More recommend