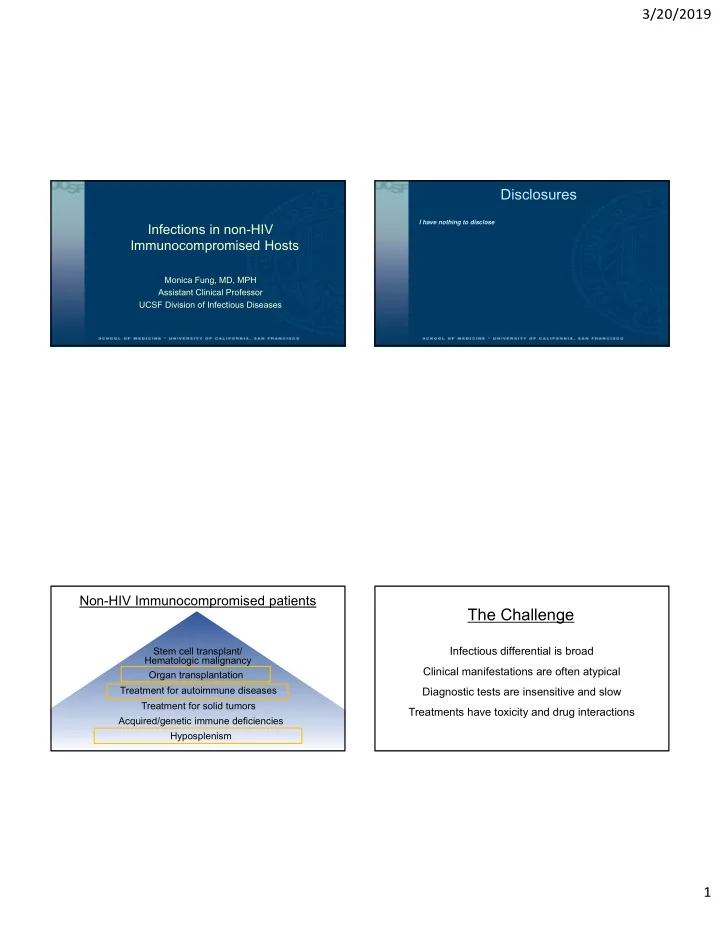
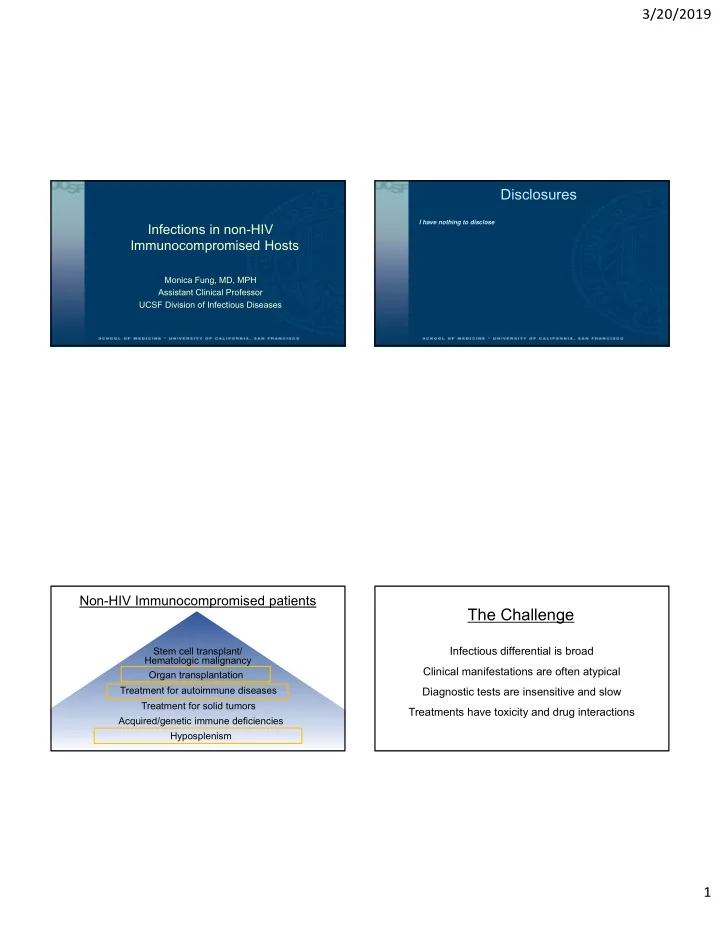
3/20/2019 Disclosures I have nothing to disclose Infections in non-HIV Immunocompromised Hosts Monica Fung, MD, MPH Assistant Clinical Professor UCSF Division of Infectious Diseases Non-HIV Immunocompromised patients The Challenge Stem cell transplant/ Infectious differential is broad Hematologic malignancy Clinical manifestations are often atypical Organ transplantation Treatment for autoimmune diseases Diagnostic tests are insensitive and slow Treatment for solid tumors Treatments have toxicity and drug interactions Acquired/genetic immune deficiencies Hyposplenism 1
3/20/2019 How does this differ from HIV patients? Humoral immunity •Rituximab (anti-CD20) HIV Non-HIV •Hyposplenism •CVID (Low IgG) Death of Innate Immune defect Heterogeneous CD4 + T-cells immunity • Organ transplant Cell‐ • Stem cell transplant • Cytotoxic chemotherapy OI risk No reliable tests mediated • TNF inhibitors CD4 + count • Chronic granulomatous immunity stratification available • Steroids disease (CGD) • Other IS Rx Non-HIV Immunocompromised patients The Spleen Stem cell transplant/ Hematologic malignancy Organ transplantation Treatment for autoimmune diseases Treatment for solid tumors Acquired/genetic immune deficiencies Hyposplenism 2
3/20/2019 Clinically-important Pathogens ASPLENIA HYPOSPLENISM (complete loss of splenic function) (partial loss of splenic function) HOW CAN YOU TELL? • Bacteria • Iatrogenic • Thalassemias • Recurrent infections with incapsulated • Streptococcus pneumoniae (pneumococcus) • Surgical removal • Chronic liver disease • Haemophilus influenzae organisms • Functional • HIV/AIDS • Neisseria meningitidis (meningococcus) • Sickle cell • • Capnocytophaga • Howell-Jolly bodies Immune disorders • Bordetella holmesii • Congenitally absent • Malignancy • Other laboratory evidence of splenic • Disorders with atrophy, • Parasites dysfunction (low IgM memory B cells) infarction, engorgement, or • Babesia infiltration of the spleen • Malaria (P. falciparum) Preventing Infections in Asplenic Patients Asplenia/Hyposplenism and Infection • Asplenic patients have increased risk infection, sepsis, and sepsis-related mortality • Cohort study of 8000 splenectomized patients • 3.4 relative risk of sepsis • 3.0 relative risk of sepsis-related mortality • Increased risk sustained over 10 years (presumably lifelong) • Similar risk presumed with asplenia/hyposplenism due to disorders • History of severe infection predisposes to additional episodes Vaccines Antibiotics Education 3
3/20/2019 Vaccines • Streptococcus pneumoniae (pneumococcus) * ≥8 weeks after • 13-valent pneumococcal conjugate vaccine (PCV13) PCV13; consider every 5 years • 23-valent pneumococcal polysaccharide vaccine (PPSV23)* • Haemophilus influenzae • H. influenzae type b vaccine (Hib) • Neisseria meningitidis (meningococcus) • Quadrivalent meningococcal conjugate ACWY vaccine series (MenACWY) • Monovalent meningococcal serogroup B vaccine series (MenB-4C or MenB-FHbp) • Influenza • Age-appropriate immunizations Antibiotics Vaccines Daily PRN • Vaccines provide adequate protection in asplenic patients, but • At least 1 year after splenectomy response may be lower than in healthy individuals • Concurrent • High local rates of resistant pneumococcus Who immunocompromising conditions • Timing of vaccines • Antibiotic intolerance • History of sepsis caused by • If possible, at least 2 weeks prior to splenectomy (ideally 10-12 weeks) encapsulated bacteria • If not prior to splenectomy, wait until 2 weeks after • Amoxicillin-clavulanate • Penicillin V 250mg PO BID 875mg/125mg PO BID • Other caveats • Amoxicillin 500mg PO BID What • Cefuroxime 500mg PO BID • Asplenia is not a contraindication to live vaccines • Cephalexin 250mg PO BID • Consider concurrent immunocompromising conditions (e.g. HIV, • Levofloxacin 750mg PO daily malignancy) • Azithromycin 250mg PO daily • Moxifloxacin 400mg PO daily 4
3/20/2019 Non-HIV Immunocompromised patients TNF inhibition • Rheumatoid arthritis • Inflammatory bowel disease Stem cell transplant/ Hematologic malignancy • Psoriasis/psoriatic arthritis Organ transplantation • Sarcoidosis Treatment for autoimmune diseases • Uveitis Treatment for solid tumors • Seronegative Acquired/genetic immune deficiencies spondyloarthropathies Hyposplenism 5
3/20/2019 TNF- ⍺ inhibitors: Tuberculosis • Post-marketing survey of TB cases following release of infliximab (1998-2001) • 70 cases of TB • Median time to diagnosis: 12 weeks (range 1-52) • TB characteristics • Extrapulmonary disease: 40/70 (57%) • Disseminated disease: 17/70 (24%) Granulomas • Mycobacteria Keane J. NEJM. 2001 • Fungi TNF- ⍺ inhibitors: TB Screening TNF- ⍺ inhibitors: Latent TB Management • All patients on TNF- ⍺ inhibitors with latent TB should be treated • In U.S., majority of TB cases due to TNF- ⍺ inhibitors are reactivation • Latent TB is diagnosed • Clinical history of TB risk • Positive IGRA or TST (≥5mm) without signs/symptoms of active TB (-CXR) • Birthplace, residence, or prolonged travel (>3mo) to TB endemic area • Negative IGRA or TST, but prior history of latent TB • Living/working homeless shelter, jail, or prison • Healthcare worker in facility with TB patients • Negative IGRA or TST with strong likelihood of prior TB exposure* • Contact with patient with active pulmonary TB • Treatment regimens • Testing * Particularly if • INH for 9 months • More sensitive in • No TB risk: 1-stage with IGRA immunosuppressed • Rifampin for 4 months immunosuppressed • TB risk: 2-stage with IGRA followed by IGRA at the time testing patients • INH x Rifapentine weekly x12 weeks or TST if first test is negative • Requires only 1 visit • Timing of latent TB treatment • Improved specificity when • Rescreening if ongoing TB risk prior BCG vaccination • No data on optimal interval: ? same time, ? delay 1-2 weeks 6
3/20/2019 TNF- ⍺ inhibitors: Active TB Management TNF- ⍺ inhibitors: Fungal Infections • Prioritize (start immediately) active TB therapy • What do do about TNF- ⍺ inhibitor? • STOP (at least temporarily) • Safe timeframe to restart: Unclear but ? after susceptibility testing and clinical improvement • Disseminated TB: watch for IRIS due after stopping TNF- ⍺ inhibitor (OR 11.4) TNF- ⍺ inhibitors: Fungal Infections Fungal Pathogen Screening Clinical history • Histoplasmosis • Travel to endemic regions • 2008 FDA Alert: • High-risk activities (e.g. spelunking) Histoplasmosis • 240 cases in patients on TNF- ⍺ inhibitors • Symptom check • 21 with delayed diagnosis and antifungal therapy CXR if suspicion for active disease or history • 12 fatal outcomes of prior infection • Concurrent methotrexate (44%) and prednisone In endemic regions (34%) common Coccidioidomycosis • CXR • Serology • Not as well characterized • Coccidioidomycosis: incidence 2.8% over 5 years on infliximab, RR 5.2 Cryptococcosis No specific recommendations • Cryptococcosis: 19 cases reported 1998-2002 Aspergillosis No specific recommendations • Aspergillosis: 39 cases reported 1998-2002 Pneumocystis No specific recommendations • Pneumocystis pneumonia: 84 cases reported 1998-2002 7
3/20/2019 TNF- ⍺ inhibitors: Other considerations • Other infectious contraindications to starting TNF- ⍺ inhibitor • Active bacterial infections • Active herpes zoster infection • Nonhealed infected skin ulcers • Acute HBV or HCV • Untreated chronic HBV infection • Child-Pugh classes B or C chronic HBV or HCV • Vaccines • Pneumococcal vaccination: PCV13 & PPSV23 • No live vaccines! Hepatitis B and Biologics Hepatitis B and Biologics • Goal: prevent HBV reactivation HBV Risk Prevention Strategy • Serologic status HBsAg- Antiviral therapy concurrent with HBsAg+ • HBsAg+: active infection HBcAb+ Moderate to immunosuppression • HBsAg-/HBcAb+: prior resolved Very High risk • Tenofovir infection Anti- Very high Moderate • Entecavir CD20 • Immunosuppressing agent Monitoring for reactivation • Rituximab (anti-CD20): reactivation Low and • HBV viral load TNF- ⍺ common Moderate Very low inhibitor Very Low Risk • LFTs • TNF- ⍺ inhibitors: reactivation reported Antiviral therapy if reactivation occurs 8
Recommend
More recommend