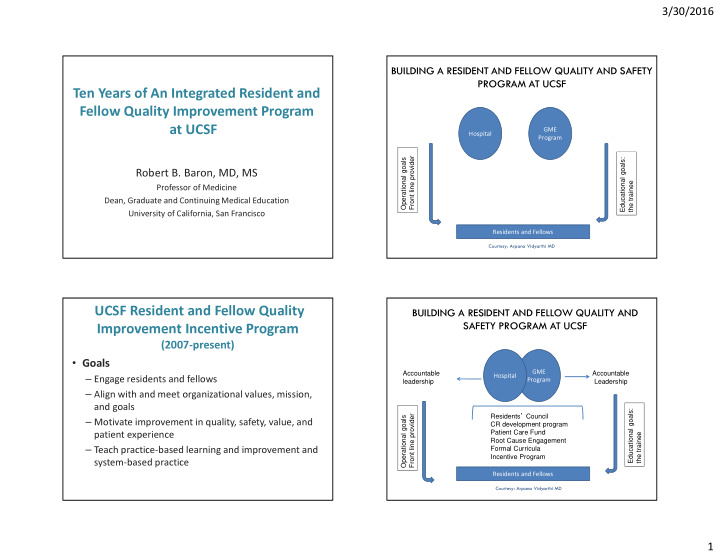

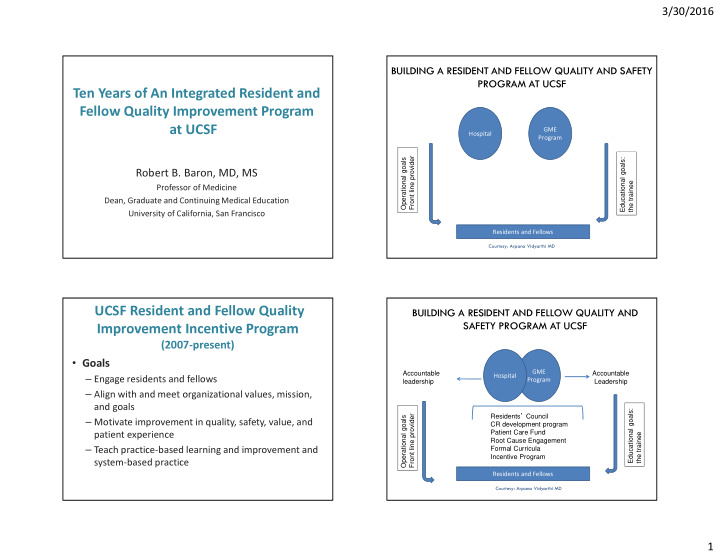

3/30/2016 BUILDING A RESIDENT AND FELLOW QUALITY AND SAFETY PROGRAM AT UCSF Ten Years of An Integrated Resident and Fellow Quality Improvement Program at UCSF GME Hospital Program Educational goals: Front line provider Operational goals Robert B. Baron, MD, MS the trainee Professor of Medicine Dean, Graduate and Continuing Medical Education University of California, San Francisco Residents and Fellows Courtesy: Arpana Vidyarthi MD UCSF Resident and Fellow Quality BUILDING A RESIDENT AND FELLOW QUALITY AND SAFETY PROGRAM AT UCSF Improvement Incentive Program (2007-present) • Goals Accountable Accountable GME – Engage residents and fellows Hospital leadership Leadership Program – Align with and meet organizational values, mission, Residents ’ Council and goals Educational goals: Front line provider Operational goals – Motivate improvement in quality, safety, value, and CR development program Patient Care Fund the trainee patient experience Root Cause Engagement – Teach practice-based learning and improvement and Formal Curricula Incentive Program system-based practice Residents and Fellows Courtesy: Arpana Vidyarthi MD 1
3/30/2016 UCSF Resident and Fellow Quality Results 2007 - 2015 Improvement Incentive Program (2007-present) • All-program goals • All-program goals – Two-thirds of goals met – 3 goals for all residents • Program-specific goals – Patient satisfaction, quality, resource utilization • Program-specific goals – Three-quarters of goals met – Residencies and fellowships design their own • Financial bonus per trainee. – Twenty five programs this year – Approximately $800 per trainee received each year • Financial bonus per trainee. “All for One” – Part of annual Health System budget ($1.2M per year) – Clear return on investment All-program Goals Discharge Before Noon Satisfaction Quality/Safety Operational 2007 Patient Survey Composite Documentation 2008 Patient Survey Pain Management CMS/TJC 2009 Patient Survey Pain Management Documentation 2010 Patient Survey Hand Hygiene Lab testing 2011 Patient Survey Hand Hygiene Lab testing 2012 Patient Survey Hand Hygiene Lab testing 2013 Patient Survey Hand Hygiene Discharge by noon 2014 Patient Survey Cost per discharge Discharge by noon 2015 Patient Survey Influenza Discharge by noon Clostridium difficile 2016 Patient Survey Cost per discharge infections 2
3/30/2016 Program-Specific Goals 2014-2015 Hand Hygiene Compliance Anesthesia Accurate use of neuromuscular transmission module in 50% of cases meeting criteria Cardiovascular Disease Provide a standardized consent video and printed post-procedure reports to 75% of patients fellowship Dermatology Distribute an Atopic Dermatitis Action Plan to 75% of eligible patients, or document reason if not appropriate Emergency Medicine Use post-intubation sedation in 80% of RSI cases Gynecologic Oncology Discharge 75% of laparoscopic cases prior to noon on the first post-operative day Hematology and Oncology Vaccinate 90% of eligible patients against Hepatitis B Hospice and Palliative Medicine Increase the use of POLST to greater than 50% of discharged patients who have chosen DNR or partial code status Internal Medicine Reduce the total number of phlebotomy draws per patient day by 5% Neurology Document an initial NIHSS score in code stroke admission notes for 90% of patients after a code stroke Neurosurgery Participate in a postoperative debrief checklist in 80% of cases Obstetrics and Gynecology Comply with new guidelines for urinary catheter removal in 80% of patients Achieve 95% completion rate of either a brief operative note or a complete operative report within 30 Orthopaedic Surgery minutes of leaving the PACU or arriving in the ICU. Program-Specific Goals 2014-2015 Internal Medicine Refer 80% of inpatients smokers to smoking cessation resources Otolaryngology Pediatrics Screen and refer 80% of parents or teens for smoking, with referral for smoking cessation Complete a postoperative checklist for microvascular free flap patients in the ICU within 90 minutes, with 90% Plastic Surgery compliance Provide intervention and document appropriate recommendations for 65% of patients with alcohol dependence or Psychiatry abuse Provide written notification to referring providers within 48 hours in 75% of patients who have significant Pulmonary CC Fellows hypoxemia during pulmonary testing (excludes those referred for immediate intervention) Complete a treatment planning session within 3 business days of initial consultation for 60% of patients treated Radiation Oncology with 3D radiation for painful bone metastases Radiology Finalize 80% of imaging reports for PE, subarachnoid, stroke, CTA by noon Surgery Increase discharge before noon of patients on the General Surgery services to greater than 30% Perform abdominal imaging every 6 months for hepatocellular cancer (HCC) screening in over 80% of males >40 Transplant Hepatology years and females >50 years of age who self-identify as being of Asian race/ethnicity Urology Increase usage of oral antimicrobials to 80% of eligible GU endoscopic cases 3
3/30/2016 Conclusions Urology • An institution-wide strategic approach is feasible and effective to improve quality, safety, value, and experience • Projects work best when interprofessional • The program enhances resident and fellow competence in PBLI and SBP • A financial incentive may add value • Despite significant costs there is a clear return on investment • Health professionals in training can be part “part of the solution” to improve health care Acknowledgements and Additional Information • Key teammates – Glenn Rosenbluth MD (GME) – Arpana Vidyarthi MD (GME) – Adrienne Greene MD (CMO) – Mark Laret (CEO) • More information – UCSF GME website (year by year projects and results) – Vidyarthi AR, et al. Acad Med, 2014 (program overview) – Vidyarthi AR, et al. Amer J Med Qual, 2015 (lab tests) – Rosenbluth G, et al. Amer J Med Quality, 2015 (hand hygiene) 4
Recommend
More recommend