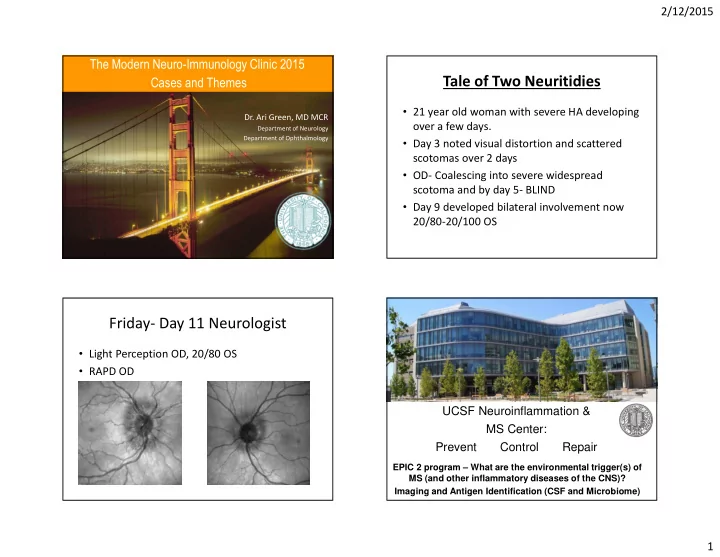
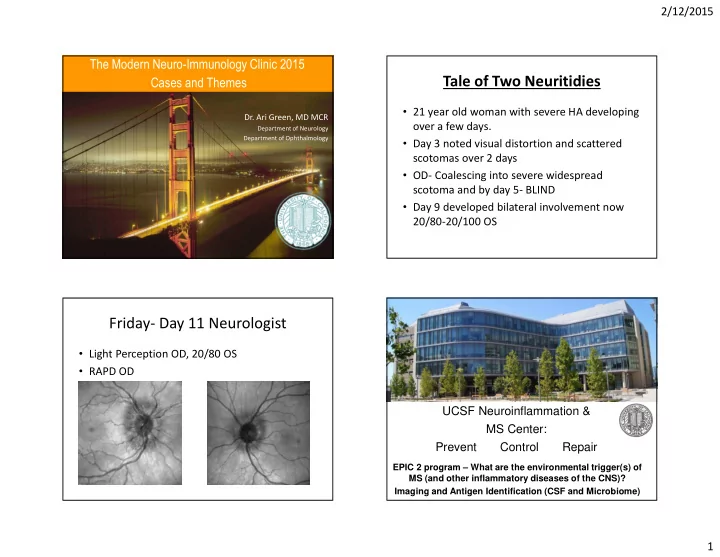
2/12/2015 ��������������������������������������� Tale of Two Neuritidies ����������������� • 21 year old woman with severe HA developing Dr. Ari Green, MD MCR over a few days. Department of Neurology Department of Ophthalmology • Day 3 noted visual distortion and scattered scotomas over 2 days • OD- Coalescing into severe widespread scotoma and by day 5- BLIND • Day 9 developed bilateral involvement now 20/80-20/100 OS Friday- Day 11 Neurologist • Light Perception OD, 20/80 OS • RAPD OD UCSF Neuroinflammation & MS Center: Prevent Control Repair EPIC 2 program – What are the environmental trigger(s) of MS (and other inflammatory diseases of the CNS)? Imaging and Antigen Identification (CSF and Microbiome) 1
2/12/2015 LP Results • LP Op 10 cm H20 • 1 wBC, 0 RBC • Normal glucose, mild protein elevation • IgG Index 0.52 and OCBs negative • NMO IgG negative • ANA negative, SSA/SSB negative Treated with 5 days IV solumderol 2
2/12/2015 What do you do next? • Stable profound residual deficit one week after steroids with no response to steroids A) Treat with 5 more days of steroids B) Treat with Erythropoetin 33,000 IU IV C) Admit for PLEX D) Watch and wait Redux? • 54 year old man painless decline in vision over a few days especially notable when playing sports • No PMHx • Sees PMD and eye care specialist who note nothing on exam • Send labs 3
2/12/2015 Labs • CBC normal • NMO negative • ACE normal • ANA/ SSA/SSB negative • RPR negative • Lyme negative 4
2/12/2015 Utility of EPs acutely LP results • 21 WBCs, 0 RBCs with 81 Lymphs 2% PMNs and 6% plasmacytoid lymphocytes • OP 20.5 cm H20 • IgG Index elevated at 0.9 • 2 OCBs present • Protein 54 (ULN 50) • Glucose 66 5
2/12/2015 “ Syphilidis sive Morbus Gallicus ” Sensitivity and Specificity of CSF- Neurosyphilis Diagnosis VDRL • CSF-VDRL specific, not sensitive “Gold Standard” for Diagnosis – False negatives 30-70% CSF WBC Ocular Syphilis • Elevated CSF WBCs >20/ul – Can be hard to distinguish from HIV Sensitivity 50% 28% • RPR negativity in very high titer secondary (“SNNOUT”) syphilis Specificity 90% 88% (“SPPIN”) 6
2/12/2015 Natural History of Syphilis Primary Syphilis Infection 2 - 6 weeks Neuroinvasion Primary • enter the body via minute abrasions of Chancre, regional adenopathy epithelial cell linings 1 - 3 months Early neurosyphilis • followed by rapid systemic spread via the Secondary Rash, generalized blood and lymphatics adenopathy • chancre is always painless and indurated 1 - 3 months Lifetime latency Latent • associated with regional lymphadenopathy > 70% months - decades Late neurosyphilis Tertiary Gumma Cardiovascular Neuroinvasion Secondary Syphilis +CSF PCR, RT- Symptoms/Signs: PCR, RIT Malaise, HA, arthralgia, sore Clearance 70% throat, fever, lymphadenopathy, Skin lesions Lab findings: Transient Persistent High titer RPR or VDRL, + 30% Meningitis Meningitis syphilis PCR Spontaneous Symptomatic 10-20% Resolution Neurosyphilis 7
2/12/2015 Tertiary Neurosyphilis Secondary Neurosyphilis • Asymptomatic (no sx, + CSF) • “ Acute meningitis ” • Meningovascular meningitis • Headache – 2-5 years after infection (rarely > 10) – Strokes, intellectual deterioration, cranial nerve • Nausea/Vertigo palsies/brainstem signs • Cervical rigidity • General Paresis – >20 years after infection • Cranial neuropathies – Personality change (paranoid, neurotic, euporic, depressed), Affect (childlike), Reflexes (hyperactive), Eyes (argyl robertson), • Ocular syphilis Sensorium (clouded), Intellectual deterioration, Slurred speech (sometimes perseverative) • Within first few years of infection (typically • Tabes Dorsalis months) – Dysesthesias --> Posterior column dysfunction --> ataxia --> paralysis Syphilis cases by country US Primary and Secondary Syphilis 2000-2006 10000 9500 9000 8500 8000 7500 7000 6500 6000 5500 5000 2000 2001 2002 2003 2004 2005 2006 8
2/12/2015 Presenting symptoms • Among 100 cases in Los Angeles County from 2001-2004 – 42% presented with visual changes – 42% presented with HA – 23% presented with cognitive issues or AMS • 60% occurred in patients who were HIV+ Treatment Normalization of CSF WBCs • Penicillin G 2.4 Million units/day (divided over 4 doses) x 2 weeks • Alternative therapy with ceftriaxone in Pen allergic patients • Adjunctive therapy with probenecid and amoxicillin not shown to be of benefit ( “ enhanced therapy ” ) ~86% 9
2/12/2015 Monitoring for treatment failure Normalization of Serum RPR • CDC recommends at 6, 12, 18 and 24 months P<0.005 • Repeat LP – pending RPR < 1:32 RPR > 1:32 10
2/12/2015 “Very Forgetful” - 57 yo right-handed man referred - Chief complaint: “very forgetful” x 1 m - Forgot names of restaurants. Colleagues at work said he repeated conversations and forgets work tasks. He is unable to recount deficits himself - Discrete episodes of “lip quivering,”, groaning, looking at his arm, trouble getting words, poor memory after, spells ~1 minute. No LOC. 11
2/12/2015 Very Forgetful - 2 • PPD+, neg CXR, untreated, works in a prison • No fevers/chills. Pet dog. Lives in Central Valley and no other travel. FLAIR T2 • Former 30+ pack year smoker - CSF exam 1 month into the clinical syndrome was entirely normal. HSV PCR negative (HSV antibodies not sent). - EEG normal - Chest/Abdomen/Pelvis CT normal , Labs: Na normal, ANA low titer + Very Forgetful - 3 Very Forgetful - 4 • Evaluated in UCSF MS and Neuroinflammation clinic • Discharged from outside hospital with valacyclovir and decadron taper • Afebrile. Well-appearing. Unremarkable general exam. • MOCA 24/30 (-5/5 for delayed recall, recalled 2 with category cues • Improved to 80-90% of normal cognitively, but and 3 with multiple choice cues with no false positives; -1 for day had frequent spells as before of week (says Friday when visit was on Monday). • Normal language. Generated 22 F words in 1 minute. • Within 3 weeks of finishing the taper, 10-15 spells per day. Says memory “good” • Normal motor, coordination, sensory and gait exams 12
2/12/2015 Emerging Paradigm: CNS Antibody Disorders Working diagnosis Neuronal Neuronal Synaptic Astrocytic Myelin Other CNS Intracellular proteins • Limbic encephalopathy, which is most likely CRMP-5, Hu, Yo NMDA, VGKC LGI-1, AQP4 ?MOG A-beta limbic encephalitis given the imaging (Purkinje cells), Ri, CASPR, AMPA, GABA-B, Ma, VGCC… appearance, clinical syndrome and amphiphysin.... Frequently associated Usually not cancer related Usually not cancer Not Not cancer related improvement with steroids with cancer (i.e. autoimmune) related • Amnestic syndrome secondary to limbic Cytotoxic T-cell Antibody/complement Antibody/compleme Less clear Response mediated nt mediated encephalopathy Antibodies “epiphenomenon”? Treatment often More robust response to Robust response to Unsatisfactory unsatisfactory standard immunosuppression treatment responses • Seizures, localization related. immunosuppression *Note that Thyroid antibodies do not have a known antigenic target in the CNS Common autoimmune encephalitides NMDAR LGI1 CASPR2 AMPAR GABAb Glycine VGKC 0.37 (normal <0.02) Mayo Approx >700 in 6 ~250 in 3 ~30 in 3 ~25 in 4 ~30 in 3 ~60 in 5 LGI1 positive Quest number of years years years years years years cases CASPR2 negative (mid-2014) Classic Diffuse LE: Morvan’s LE LE Progressive phenotype encephalitis, Amnesia, syndrome: encephalomyel neuropsychiatric seizures, dysautonomia, itis with rigidity features, hyponatremia neuropsychiatric, and myoclonus movement neuromyotonia; (PERM) disorder, seizures, Sometimes LE autonomic Expanding Pure FBDS, Cryptogenic Psychosis LE, brainstem Final Diagnosis: phenotype neuropsychiatric Bradycardic epilepsy, GBS- (atypical) syndromes, or “milder” cases prodrome, like epilepsy cryptogenic epilepsy LGI1 (VGKC-complex) Limbic Encephalitis Tumor Ovarian <10% Thymoma Lung, Lung (~50%) Thymoma teratoma (~30%) (various) (~30%) breast, (<10%) thymoma Infectious Post-HSV encephalitis Adapted from Irani, Gelfand, Al-Diwani, Vincent, Annals of Neurology, 2014 13
Recommend
More recommend