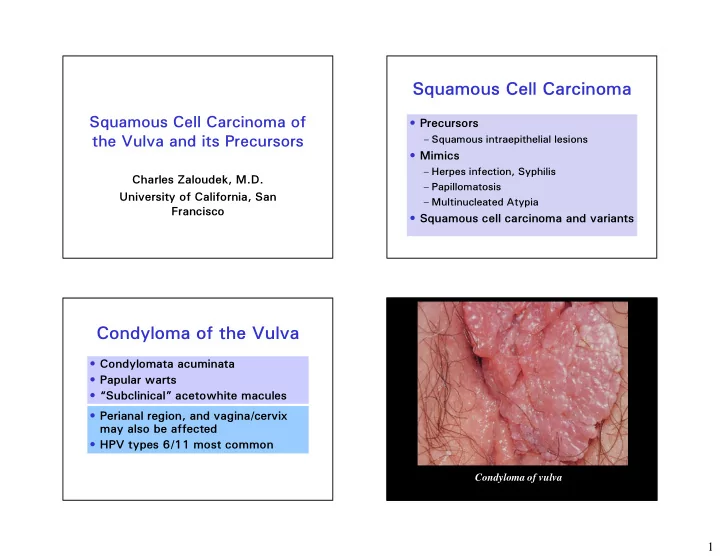
Squamous Cell Carcinoma Squamous Cell Carcinoma of • Precursors – Squamous intraepithelial lesions the Vulva and its Precursors • Mimics – Herpes infection, Syphilis Charles Zaloudek, M.D. – Papillomatosis University of California, San – Multinucleated Atypia Francisco • Squamous cell carcinoma and variants Condyloma of the Vulva • Condylomata acuminata • Papular warts • “Subclinical” acetowhite macules • Perianal region, and vagina/cervix may also be affected • HPV types 6/11 most common Condyloma of vulva 1
Diagnostic Criteria for Condyloma of Vulva • Koilocytosis – cavitated cytoplasm • Nuclear atypia – enlargement, hyperchromasia, pleomorphism, multinucleation, membrane irregularity • Architectural abnormalities – papillomatosis, acanthosis, hyperkeratosis, parakeratosis • MIB-1 staining : Group of 2 or more stained nuclei in same HPF in upper 2/3 of epithelium • More specific: HPV immunohistochemistry and in situ hybridization 2
High Grade SIL (VIN) Classic, or Bowenoid Type • Young women - 30’S and 40’s - increasing in incidence • History of condylomas, herpes infection, HIV disease, smoking • Linked to HPV, usually HPV 16 • Varied appearance: – Papules, plaques, polyps – White, red, or pigmented • Multicentric disease in vagina or cervix Positive HPV ISH Positive HPV Immunostain Vulvar intraepithelial neoplasia Vulva - VIN III 3
Pagetoid Lesions of the Vulva HMWK LMWK CK 7 CEA S100 VIN + - + - - Melanoma - - - - + Paget’s - + + + - Pagetoid VIN 4
The Problem with Low Grade High Grade SIL SIL (VIN) Results of Therapy • Treatment: Excision, laser ablation, • Less than 50% of cases topical imiquimod of VIN I confirmed on • Local recurrence - up to 35% review • Occult invasion - up to 20% • 70% of cases associated • Invasive carcinoma develops in with low risk HPV – 3-10% of treated patients • MIB-1 positive nuclei in – 9% to up to 90% of untreated patients – Invasive carcinoma is basaloid or upper epithelium condylomatous type, some keratinizing correlate with VIN I • Bowenoid papulosis Logani S, et al. Mod Pathol 2003;16(8):735-741 Status of VIN Classification Low Grade SIL of the Vulva Pre-LAST • Some papillomatous with prominent • Category of VIN I eliminated koilocytotic atypia (~ 1/3) – ISSVD • Some flat with minimal koilocytotic – WHO 2004 atypia (~ 2/3) • Most cases VIN I flat condyloma or • No difference in HPV type distribution reactive • 91% had detectable HPV • Diagnosis of VIN refers to high grade lesions only • Classical and Differentiated types Srodon M, et al. Am J Surg Pathol 2007;30:1513-1518 5
VIN 1 with extensive koilocytotic HPV Types in Low Grade SIL of atypia found to have HPV 59 Various Sites HPV T ype Vulva Vagina Cervix Low risk 67% 35% 6% VIN 1 with minimal koilocytotic 6 or 1 1 42% 0 6% atypia found to have HPV 68 High risk 42% 76% 94% 16 6% 6% 1 1% 18 0 24% 17% VIN 3 with HPV 16 Srodon M, et al. Am J Surg Pathol 2007;30:1513-1518 Srodon M, et al. Am J Surg Pathol 2007;30:1513-1518 VIN HPV Types in High Grade SIL of Simplex or Differentiated Type Various Sites • 2-10% of VIN HPV T ype Vulva Vagina Cervix • Postmenopausal women, average age late Low risk 3% 6% 0% 60’s 6 or 1 1 3% 0 0% • Small lesions, roughened gray white, or High risk 100% 94% 100% white plaques, may be multifocal 16 91% 50% 75% • Lichen sclerosis may also be present 18 6 0% 4% • Not associated with HPV • ? Greater potential for progression to Srodon M, et al. Am J Surg Pathol 2007;30:1513-1518 invasive carcinoma; invasive carcinoma is keratinizing squamous cell type 6
p53 7
p53 MIB1 p53 8
Differentiated vulvar intraepithelial neoplasia contains TP53 mutations and is genetically linked to vulvar squamous cell Expanding the morphologic spectrum of differentiated VIN carcinoma. (dVIN) through detailed mapping of cases with p53 loss. Pinto AP, et al. Mod Pathol (2010) 23: 404-412. Singh N, et al. Am J Surg Pathol, 2015;39:52-60 • 6 of 10 dVIN cases had at least 1 VIN focus • p53 negative dVIN and SCC, when present, with 1 or more TP53 mutations in 14 specimens from 10 patients • 4 were p53 immunopositive (missense or splice) • 27% of dVIN cases at Vancouver General and 2 were p53 negative (deletions) Hospital • 5 had SCC associated with dVIN, 4/5 had TP53 • 1 case reclassified as not dVIN mutations • In 5/13 the p53 negative areas corresponded – 2 missense, p53 positive to the morphologic dVIN – 2 nonsense, p53 negative • In 8/13 the p53 negative areas were more • 2/4 cases had same TP53 mutation in dVIN and extensive than the morphologic dVIN and in SCC some were at margins • Multiple foci dVIN with different mutations in some cases Expanding the morphologic spectrum of differentiated VIN (dVIN) through detailed mapping of cases with p53 loss. Singh N et al. Am J Surg Pathol 2015;39:52-60 9
p53 CK17 FIGURE 1. A, Simplex vulvar intraepithelial neoplasia, grade 3 of basaloid type. Diffuse replacement of the whole epidermis by a homogeneous population of small, "undifferentiated" keratinocytes with scanty cytoplasm extending throughout the entire thickness of the epidermis, showing no or only minimal maturation in superficial layers. Normal vulvar squamous epithelium is present on the left. B, The epidermis is thickened and shows a parakeratotic surface reaction. The rete ridges are elongated and markedly enlarged and coalescent. C, Small cells, with scant cytoplasm, showing large vesicular nuclei, with visible nucleoli. D, p16 Moderate to severe atypia, with nuclear pleomorphism, multinucleation, and dyskeratosis. Ordi J et al. Am J Surg Pathol 2009 33:1659-1665 10
LAST Project Current Classification of Vulvar Lower Anogenital Squamous Terminology Standardization Squamous Intraepithelial Lesions Project for HPV-associated Lesions • Single set of diagnostic terms for all lower WHO, 2014 ISSVD, 2015 anogenital sites Low grade SIL Low grade SIL (vulvar • Two-tiered nomenclature for intraepithelial LSIL, flat condyloma or High grade SIL lesions HPV effect) – Low grade generally self-limited lesions Differentiated type VIN – High grade potentially progressive lesions High grade SIL (vulvar • Recommended terminology: HSIL, VIN usual type) -WHO Classification of – Low grade SIL Tumours of the Female Differentiated type VIN – High grade SIL Reproductive Organs, 4 th Ed, 2014 • Use p16 only to improve accuracy -Bornstein J, et al. Obstet Gynecol -Stoler MH and Kurman RJ. 2016;127:264-268 • Vulvar SISCCA = FIGO IA cancer Am J Surg Pathol -Sideri M, et al. Am J Surg Pathol 2007;31;1452-1454 2007;31:1452 Int J Gynecol Pathol 2013; 32:76-1 15 Squamous Cell Carcinoma of the Vulva • Type I – Younger women, average age 55 – VIN, HPV associated, usually HPV 16 – Basaloid, condylomatous types • Type II – Older women, average age 77 – No or simplex VIN, no HPV, some LS or SH – Keratinizing squamous cell carcinoma 11
HPV Testing in Vulvar HPV and Squamous Cell Carcinoma Carcinoma of the Vulva Toki, Kurman, et al 1991 • HPV prevalence in vulvar Ave. Ave. Adj. Adj. Adj. Adj. HPV+ HPV+ SH, LS Adj Nl SH, LS Adj Nl intraepithelial neoplasia: 52% Age Age VIN VIN to 100% 77 77 4/19 4/19 2/19 2/19 14/19 14/19 3/19 3/19 SCC SCC • HPV prevalence in invasive 54 54 6/8 6/8 7/8 7/8 0 0 1/8 1/8 BC BC squamous cell carcinoma: 47 47 3/3 3/3 3/3 3/3 0 0 0 0 WC WC 15% to 79% Histopathology 2013; 62:161-175 VIN and LS adjacent to thin vulvar SCC HPV in SCC of the Vulva Classic Differentiated T ype Ca No VIN VIN VIN • Worldwide study of 2296 cases, 587 Keratinizing 9 18 1 1 VIN and 1709 invasive SCC SCC-38 – 25.1% SCC were HPV related Warty 6 0 0 – Prevalence of HPV related highest in SCC-6 young women Basaloid 4 0 0 – Basaloid and warty most likely to be HPV SCC-4 positive LS 1/19 9/16 4/9 – HPV 16 most common (72.5%, followed by HPV 33 (6.5%) and HPV 18 (4.6%) Age Pt. 62 78 75 De Sanjose, S, et al. Eur J Cancer 2013;49:3450-3461 Am J Surg Pathol 2006;30:310-318 12
Squamous Cell Carcinoma Grading of Vulvar Squamous Cell Carcinoma of the Vulva • Grade 1: No poorly differentiated • Most occur on labia component • Clitoris involved in <15% • Grade 2: < 50% poorly differentiated • Multifocal in <10% component • Exophytic papillary • Grade 3: > 50% mass or endophytic poorly differentiated ulcer component Squamous Cell Carcinoma of the Vulva Subtype 1 1 Keratinizing Non-keratinizing Basaloid Warty (Condylomatous) Verrucous 2 3 13
Basaloid T ype of Squamous Cell Carcinoma 14
Recommend
More recommend