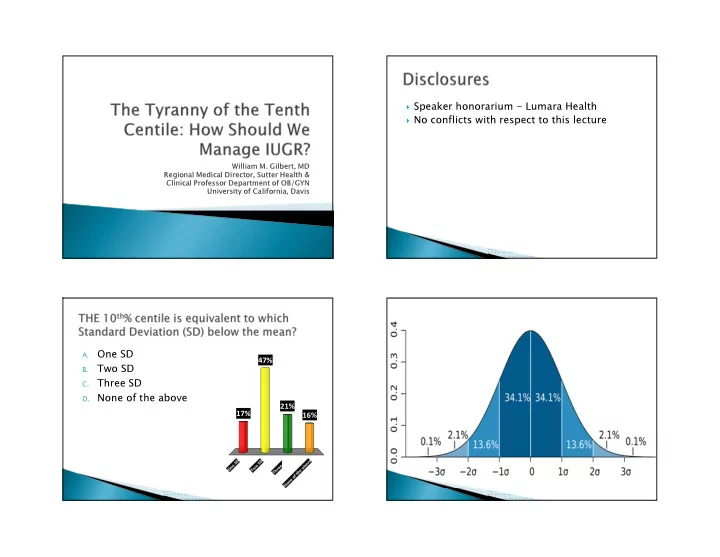
� Speaker honorarium - Lumara Health � No conflicts with respect to this lecture William M. Gilbert, MD Regional Medical Director, Sutter Health & Clinical Professor Department of OB/GYN University of California, Davis One SD A. 47% Two SD B. Three SD C. D. None of the above 21% 17% 16%
� Definitions ◦ Birth weight < 2500 gm 43% AC < 10% centile ◦ EFW < 10 th centile A. ◦ Abdominal circumference < 10 th centile AC < 5 th % centile B. ◦ EFW < 10 th centile AND abnormal Dopplers AC < 3 rd centile 27% C. ◦ AC < 10 th centile AND abnormal Dopplers 19% D. None of the above � SGA relates to newborns < 10 th centile 11%
� 40% of total birth weight due to genetic factors ◦ Maternal primary influence � IUGR in mother increased in offspring � 60% environmental factors ◦ Nutrition ◦ Smoking ◦ Placental factors � Maternal medical conditions � Substance use and abuse ◦ Pregestational diabetes � Multiple gestations ◦ Renal insufficiency � Teratogen exposure ◦ Autoimmune disease ◦ Chemo agents, valproic acid, antithrombotic drugs ◦ Cyanotic cardiac disease � Infectious disease ◦ Pregnancy related hypertension ◦ TORCH, CMV, malaria, syphilis, Zika � Chronic HTN, Gest HTN, PE � Genetic and structural disorders ◦ Antiphospholipid antibody syndrome ◦ T-13, T-18, CHD or gastroschisis � Placental disorders
� Before birth ◦ Increase in Stillbirth, C/S for fetal distress, meconium staining of amniotic fluid � Afterbirth - Birth weight < 10 th centile ◦ PVL, CP ◦ Later life: � Hypertension � Heart disease � DM � Indirect measure of blood flow � Not a good screening tool alone � Is effective with IUGR fetuses � Becomes abnormal before FHT variability � Fd = 2F*V*COS theta 1540 cm/sec
� Most useful with diagnosing fetal anemia ◦ Used with rH isoimmunization and anti Kell ◦ Did away with: � Amniocentesis for Delta-OD450 � Use of the Lilly curve � With fetal hypoxia ◦ Decreased resistance allowing an increase in blood flow to the brain
� Ireland -1200 consecutive pregnancies EFW< � Average maternal age - 30 years old 10 th centile � 83% white European decent � 1/2010 through 6/2012 � Mean GA at enrollment - 30.1 weeks � Examined EFW or AC <10 th , <5 th , <3 rd centile � Mean Delivery GA - 37.8 weeks ◦ Every two weeks � NICU admission - 28% � Abnormal Doppler, oligohydramnios � Adverse outcome 5.2% � Adverse Outcome index � Mortality 0.7% ◦ Death, IVH, RDS, PVL, HIE, BPD, sepsis � 72% had a normal outcome
� EFW < 10 th centile alone: ◦ No increase in M&M � Real increase in Morbidity and Mortality ◦ Abnormal UA Doppler in all EFW < 10 th centile ◦ Oligohydramnios important only with EFW < 3 rd centile ◦ Only weight related basis was EFW < 3 rd centile � 1/2008 through 7/2012 � EFW < 10 th centile 789 with IUGR (7%) � Excluded: multiples, anomalies, absent or reversed Doppler EDVs � Leaving 512 ◦ 394 with normal UA Doppler ◦ 118 with UA Doppler > 95 th centile
� After controlling for demographic and GA at � Protocol to get Abnl UA Doppler to 37 weeks delivery etc ◦ 36 4/7 weeks ◦ Birth weight < 10 th centile - 84.7% � No difference in: ◦ Mean 2.178 kg ◦ NICU admissions ◦ Composite neonatal morbidity � Normal UA Doppler to 39 weeks ◦ Perinatal deaths ◦ 37 6/7 weeks ◦ Birth Weight < 10 th centile - 66.2% � Conclude: In cases of IUGR with: ◦ Abnormal UA Doppler, delivery at 37 weeks ◦ Mean 2.532 kg ◦ Equals 39 weeks with normal UA Dopplers � Ratio of MCA Doppler PI to UA PI � Retrospective cohort study IUGR pregnancies � Adverse outcomes, IVH, death, NRFHT, pH< 7.0, Apgar at 5 < 7, PVL, RDS � 183 identified with 70 at least 1 adverse event � Compared CPR < 1.08 and CPR < 5 th centile
� CPR predictive of poor outcome in: � Definition of IUGR is not well defined ◦ EFW < 10 th centile most commonly used ◦ AGA fetuses ◦ EFW < 3 rd centile more predictive of poor outcome ◦ SGA fetuses ◦ With Abnormal UA Doppler, real increased risk of � May be a screening tool for ALL pregnancies poor outcome in the third trimester ◦ Oligohydramnios - Less important but still � Better than the biophysical profile recommended � Better than UA and MCA Dopplers alone � CPR appears to be better for identifying adverse outcome but further confirmatory studies needed
� Day to Day management ◦ Suspect IUGR? Ultrasound including UA Doppler ◦ EFW < 10th centile with UA Doppler normal? � Deliver at 39 weeks, Repeat US in 2-3 weeks � NSTs OK ◦ EFW < 10 th centile and UA Doppler Abnormal? � Deliver at 37 weeks or earlier PRN � NSTs definitely � Absent or Reversed End Diastolic velocities? ◦ Hospitalize and or deliver
Recommend
More recommend