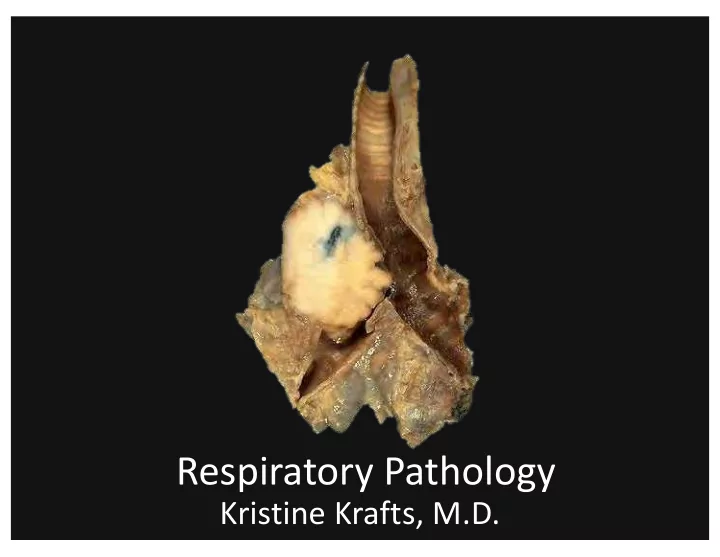
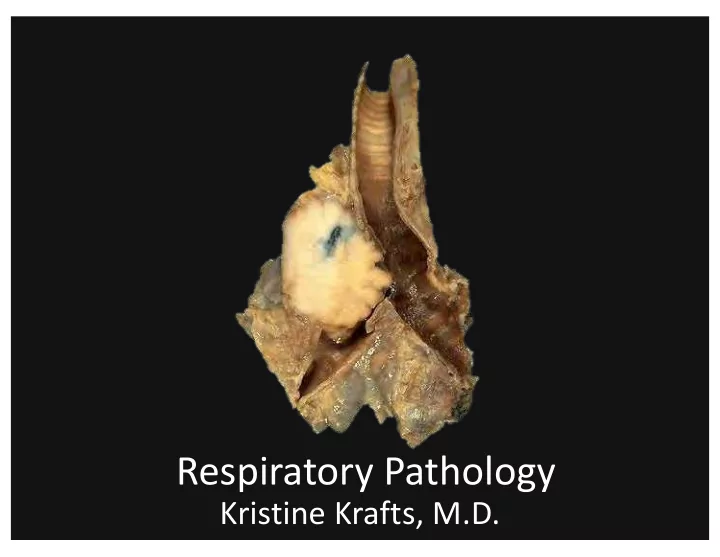
Respiratory Pathology Kristine Krafts, M.D.
Normal lung: alveolar spaces
Respiratory Pathology Outline • Acute respiratory distress syndrome • Obstructive lung diseases • Restrictive lung diseases • Vascular diseases • Infections • Carcinoma
Respiratory Pathology Outline • Acute respiratory distress syndrome
Acute respiratory distress syndrome • Symptoms: rapid onset respiratory insufficiency that doesn’t respond to oxygen • Associated with pneumonia, aspiration of gastric contents, sepsis, severe trauma • Pathogenesis: Damage to alveolar capillary membrane; neutrophils play a big role • Morphology: “diffuse alveolar damage” with hyaline membranes
Diffuse alveolar damage: hyaline membranes
Respiratory Pathology Outline • Acute respiratory distress syndrome • Obstructive lung diseases
Respiratory Pathology Outline • Acute respiratory distress syndrome • Obstructive lung diseases • Emphysema • Chronic bronchitis • Asthma • Bronchiectasis
Emphysema • Destruction/enlargement of airspaces • Centriacinar emphysema • Destruction of proximal acinus • Worse in upper lobes of lung • Smoking • Panacinar emphysema • Destruction of entire acinus • Worse in lower lobes of lung • Alpha-1-antitrypsin deficiency
Pathogenesis of emphysema Smoking α-1 antitrypsin deficiency
Emphysema: dilated air spaces
Emphysema: dilated air spaces
Chronic Bronchitis • Definition: persistent, productive cough for ≥ 3 months in ≥ 2 consecutive years • Pathogenesis: hypersecretion of mucous • Cause: smoking (mostly) and pollution
Chronic bronchitis: mucous gland hyperplasia
Asthma • Chronic inflammatory disease of airways leading to bronchial constriction • Symptoms: wheezing, breathlessness • Hallmarks: intermittent, reversible airway obstruction, chronic inflammation, increased mucus. • Atopic (allergic) vs. non-atopic • Triggers: allergens, infection, smoke, cold, exercise
How is asthma triggered?
Then what happens?
Bronchiectasis • Permanent dilation of bronchi and bronchioles due to chronic inflammation • Secondary to: • obstruction (tumor) • congenital conditions (cystic fibrosis) • bad pneumonia
Bronchiectasis
Respiratory Pathology Outline • Acute respiratory distress syndrome • Obstructive lung diseases • Restrictive lung diseases
Idiopathic pulmonary fibrosis • Patchy, progressive lung fibrosis • Symptoms: gradual onset cough, dyspnea. Respiratory failure and cor pulmonale within about 3 years • Radiologic and histologic term: “usual interstitial pneumonia”
IPF: fibrotic lung
IPF: tons of fibrosis
Pneumoconioses • Disorders caused by inhalation of mineral dusts • Size matters (1-5 μm particles are worst) • Three main dust particles: • Carbon (coal workers) • Silica (sandblasting, mining, ceramics) • Asbestos (mining, insulation removal)
Asbestos fibers
Respiratory Pathology Outline • Acute respiratory distress syndrome • Obstructive lung diseases • Restrictive lung diseases • Vascular diseases
Pulmonary embolism • Most arise from leg veins • Small emboli may be asymptomatic, cause infarction, or cause hemoptysis • Medium-sized emboli (less common) cause shortness of breath and infarction • Large emboli (even less common) can cause sudden death
Pulmonary embolism
Pulmonary infarcts
Respiratory Pathology Outline • Acute respiratory distress syndrome • Obstructive lung diseases • Restrictive lung diseases • Vascular diseases • Infections
Pneumonia • 1/6 of all deaths in the US! • Can be acute or chronic • Causes: bacteria, viruses • Different anatomic patterns • Different clinical settings
Typical bugs in different clinical settings Community-acquired Immunocompromised • Streptococcus pneumoniae • Cytomegalovirus • Haemophilus influenzae • Pneumocystis jiroveci • Mycoplasma pneumoniae • Aspergillus • viruses Nosocomial Chronic • Mycobacterium tuberculosis • gram-negative rods • Histoplasma capsulatum • Staphylococcus aureus Aspiration • Anaerobic bacteria
Most community-acquired pneumonias are one of these: Interstitial Alveolar • viruses • Streptococcus pneumoniae* • Mycoplasma pneumoniae • Staphylococcus aureus • Hemophilus influenzae * Most common
interstitial inflammation alveolar inflammation Viral pneumonia Bacterial pneumonia
Lung abscess • Localized collection of pus • Bugs: Staph , Strep , gram-negative bugs, anaerobes, or mixture • Pathogenesis: aspiration of infected material (from teeth, sinuses), aspiration of gastric contents, as complication of nasty bacterial pneumonia
Lung abscess
Tuberculosis • Cause: Mycobacterium tuberculosis • Chronic, granulomatous disease that can involve any organ but often involves lungs • Spread by respiratory droplet • Primary (initial) TB: Ghon complex. • Secondary (reactivation) TB: Cavitating granulomas.
necrotic debris just macrophages lymphocytes (no necrotic debris) macrophages Regular (non-caseating) Caseating granuloma granuloma
regular macrophages necrotic debris foreign-body giant cells Caseating granuloma
TB organisms (acid-fast stain)
lung lesion involved lymph nodes Ghon complex: lung lesion + involved nodes
Secondary TB: tons of caseating, cavitating necrosis
Spleen: miliary TB
Opportunistic pneumonias • Affect immunosuppressed patients (patients with AIDS, cancer, post-transplant) • Unusual organisms: • Pneumocystis jiroveci • Aspergillus • Cytomegalovirus
Crushed Ping-Pong ball shaped organisms Crescent shaped organisms Pneumocystis
Aspergillus
Cytomegalovirus (two kinds of inclusions)
Respiratory Pathology Outline • Acute respiratory distress syndrome • Obstructive lung diseases • Restrictive lung diseases • Vascular diseases • Infections • Carcinoma
Types of lung cancer Adenocarcinoma Squamous cell carcinoma Large cell carcinoma Small cell carcinoma
Types of lung cancer Adenocarcinoma NSCLC Squamous cell carcinoma Large cell carcinoma SCLC Small cell carcinoma
Presenting symptoms Potentially curable Usually incurable • asymptomatic • dyspnea • cough • chest pain • hemoptysis • anorexia & weight loss • hoarseness • bone pain
Survival statistics…bad. • At diagnosis, >50% have metastases • Overall (all stages) 5ys = 16% • Localized disease 5ys = 45%
Adenocarcinoma • Most common type, especially in women and non-smokers • Usually peripheral
Adenocarcinoma
Adenocarcinoma in situ • Was called bronchioalveolar carcinoma • A rare type of adenocarcinoma • 5 year survival better (40%) • Grows along existing architecture
Adenocarcinoma in situ
Adenocarcinoma in situ
Squamous cell carcinoma • Malignant tumor of squamous cells • Usually centrally located • Usually preceded by distinct lesions
Squamous cell carcinoma precursor lesions squamous metaplasia dysplasia carcinoma in situ
Squamous cell carcinoma
Squamous cell carcinoma
Large cell carcinoma • Composed of large cells • Kind of a “wastebasket” term • Many are probably just anaplastic squamous cell carcinomas or adenocarcinomas
Large cell carcinoma
Small cell carcinoma • VERY high mortality • Small cells, minimal cytoplasm, “molding” • Paraneoplastic syndromes • High growth fraction yet treatment ineffective • Median survival (with treatment) = 1 year
Small cell carcinoma
Mesothelioma • Malignant tumor of mesothelial cells • Most patients have had asbestos exposure • Not related to smoking • Highly malignant; short survival.
Mesothelioma
Recommend
More recommend