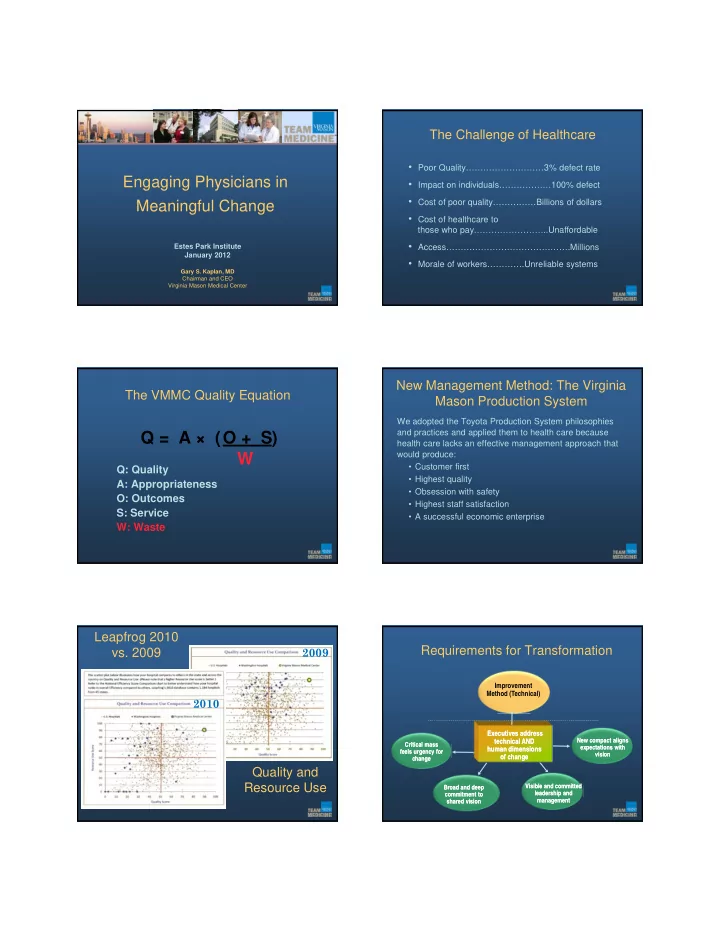
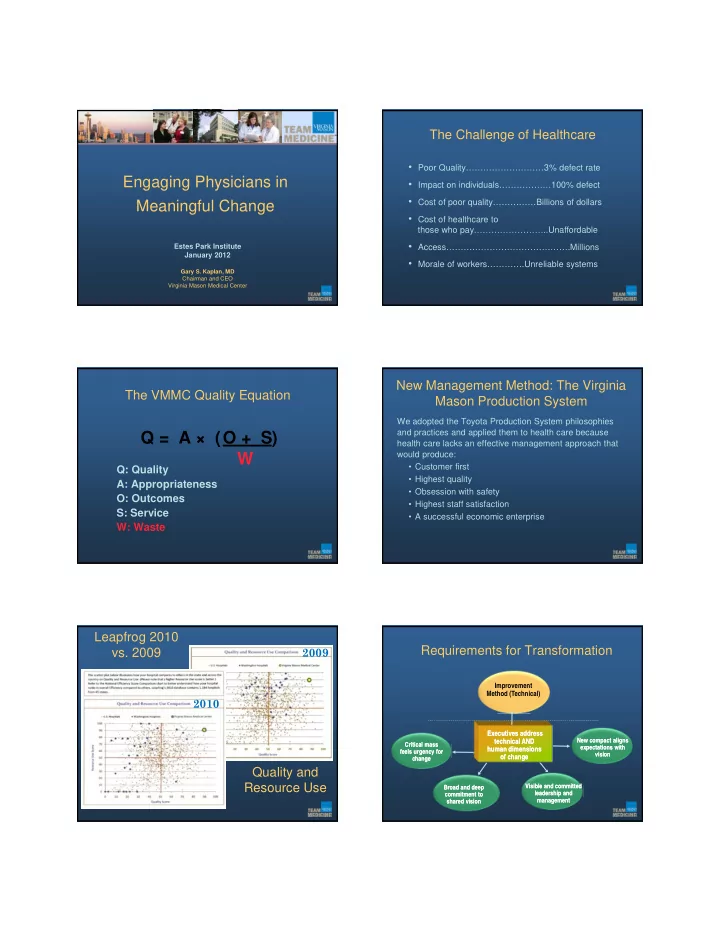
The Challenge of Healthcare • Poor Quality………………………3% defect rate Engaging Physicians in • Impact on individuals………………100% defect • Cost of poor quality……………Billions of dollars Meaningful Change • Cost of healthcare to those who pay……………………..Unaffordable • Access…………………………………….Millions Estes Park Institute January 2012 • Morale of workers………….Unreliable systems Gary S. Kaplan, MD Chairman and CEO Virginia Mason Medical Center New Management Method: The Virginia The VMMC Quality Equation Mason Production System We adopted the Toyota Production System philosophies and practices and applied them to health care because Q = A × (O + S) health care lacks an effective management approach that W would produce: • Customer first Q: Quality • Highest quality A: Appropriateness • Obsession with safety O: Outcomes • Highest staff satisfaction S: Service • A successful economic enterprise W: Waste Leapfrog 2010 2009 Requirements for Transformation vs. 2009 Improvement Method (Technical) 2010 Executives address Executives address technical AND technical AND New compact aligns New compact aligns Critical mass Critical mass expectations with expectations with human dimensions human dimensions feels urgency for feels urgency for vision vision of change of change change change Quality and Resource Use Visible and committed Visible and committed Broad and deep Broad and deep leadership and leadership and commitment to commitment to management management shared vision shared vision
Two Kinds of Challenges Technical Change Ronald Heifetz Adaptive Technical • Challenge is complex • Problem is well defined • To solve requires • Solution is known can be transforming long-standing found habits and deeply held • Implementation is clear assumptions and values • Involves feelings of loss, sacrifice (sometimes betrayal to values) • Solution requires learning and a new way of thinking, new relationships Adaptive Challenge Urgency: Make the Invisible Visible • HOW Self-discovery” – experiential More than facts: John Kotter’s see/feel/change approach • WHAT Cost of doing nothing exceeds cost of change Cold, hard facts on performance and lack of sustainability Gap between aspiration and reality The personal impact of incidents Urgency for Change at VMMC Ongoing Urgency • In a time of constant “ and tumultuous ” We change or we die. change, avoid complacency — Gary Kaplan , VMMC Professional staff meeting, October 2000
̶ Everyone Changes Basis of Vision is Shared Interests • It’s not just physician leaders who shift mindset and actions • Working collaboratively with physicians Organization’s Doctors’ Doctors’ represents an adaptive change for many Interests Interests Interests administrative leaders • Need to move away from language such as: “We need to gain their buy-in” and “We’ll roll it out” SHARED I NTERESTS • Commitment to patients • Economic interests • Recruit and retain talent Some Leadership Styles Thwart Engagement as Key to Coming to Terms Adaptive Work with New Realities • Command and Engaging physicians (and other clinicians): control • Surfaces their good ideas, input, and wisdom • Holding onto all • Develops ownership for solutions authority • Is a critical opportunity for individuals to • Laissez Faire personally process and come to terms with a change and its implications Bedrock of Fair Process: Three Engage Stakeholders Principles • Engagement: involving individuals in decisions that “ affect them. Not handing over control or decision- ” making authority You can’t impose anything on anyone Not endless process and expect them to be committed to it. Not decision by consensus Not getting agreement through compromise Edgar Schein, Professor Emeritus • Explanation: everyone involved and affected should MIT Sloan School understand the rationale for final decision • Expectation clarity: when a decision means new “rules of the game,” they are clearly articulated
Compact Traditional Physician Compact • Expectations members of an organization G IVE G ET have that are: Unstated yet understood • Treat Reciprocal patients • The give • Provide quality care • The get • Autonomy (personally defined) Mutually beneficially • Protection • Entitlement Set up & reinforced by society and the organization Proactively Develop New Clash Of “Promise” And Imperatives Expectations Traditional “ Promise” • When old deal crumbles without Imperatives Legacy Expectations conversation, anger and frustration result • Improve safety/ quality • Dialogue about what is changing • Implement EHR • Autonomy and why accelerates support for • Create service • Protection experience new deal, new behaviors • Entitlement • Be patient-focused • Improve access • Improve efficiency • Recruit/retain quality staff Old Compact at VMMC Not Working Vision Is Context for Compact • Despite the fact things weren’t working, most Organization gives: • Societal needs Physicians give : physicians clung to the fundamental “gets” • Local market • What the • What helps they felt due them physicians meet organization • Competition needs to achieve commitment Protection the vision • What is • Organization’s meaningful to Autonomy strengths physicians Entitlement • Physician-centered world view prevailed
VMMC Compact Process VMMC Compact Process Physician Retreat Physician Retreat Physician Physician (Fall 2000) (Fall 2000) Retreat Retreat • Broad based committee of providers: (Fall 2000) (Fall 2000) Compact committee Compact committee primary care, sub-specialists drafts compact drafts compact • Focus of retreat: physicians-changing (Winter 2001) (Winter 2001) expectations, tools to manage change • Jack Silversin served as our consultant • Broad based group of providers • Spent time at VMMC talking to • Administrative Involvement: CEO, JD, HR, Board physicians Member (also a patient) • Starting point: “Gives” and “gets” from the Retreat Evolving Strategic Plan: patient centered Virginia Mason Medical Center VMMC Compact Process Physician Compact Organization ’ s Responsibilities Physician ’ s Responsibilities Physician Retreat Physician Retreat Foster Excellence Focus on Patients • Recruit and retain superior physicians and staff • Practice state of the art, quality medicine (Fall 2000) (Fall 2000) • Support career development and professional satisfaction • Encourage patient involvement in care and treatment decisions • Acknowledge contributions to patient care and the • Achieve and maintain optimal patient access • Insist on seamless service organization Compact committee Compact committee • Create opportunities to participate in or support research Collaborate on Care Delivery • Include staff, physicians, and management on team Listen and Communicate drafts compact drafts compact • Share information regarding strategic intent, • Treat all members with respect (Winter 2001) (Winter 2001) • Demonstrate the highest levels of ethical and professional organizational priorities and business decisions • Offer opportunities for constructive dialogue conduct • Provide regular, written evaluation and feedback • Behave in a manner consistent with group goals Departmental • Participate in or support teaching Educate • Support and facilitate teaching, GME and CME meetings for input Listen and Communicate • Committee met weekly • Provide information and tools necessary to improve • Communicate clinical information in clear, timely manner • Request information, resources needed to provide care (Spring 2001) practice • Reality Checks Reward consistent with VM goals • Provide clear compensation with internal and market • Provide and accept feedback Management Committee consistency, aligned with organizational goals Take Ownership • Create an environment that supports teams and • Implement VM-accepted clinical standards of care Physicians individuals • Participate in and support group decisions • Focus on the economic aspects of our practice Lead • Multiple Drafts until we reached the “final draft” Manage and lead organization with integrity and Change • Embrace innovation and continuous improvement accountability • Participate in necessary organizational change Hardwiring Compact Compact Supports Alignment with Vision • Recruitment • Compact discussions as foundational – basic to • Orientation moving us toward vision • Job Descriptions • Compact is revisited, made alive, reinforced Chief • Periodic assessments/dialogue as to how both Section Heads “sides” are living up to compact commitments Physicians • Feedback
Recommend
More recommend