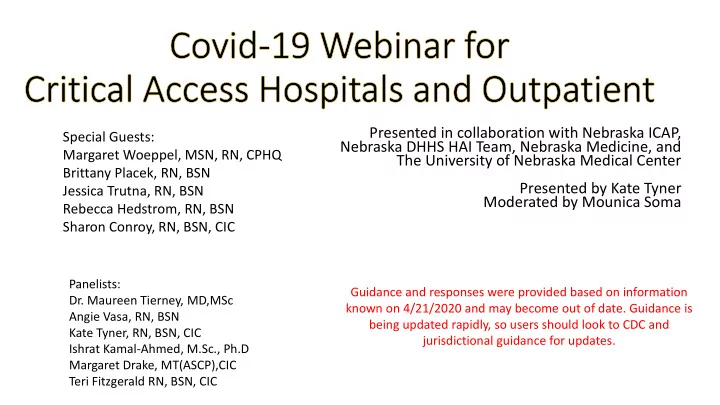
Presented in collaboration with Nebraska ICAP, Special Guests: Nebraska DHHS HAI Team, Nebraska Medicine, and Margaret Woeppel, MSN, RN, CPHQ The University of Nebraska Medical Center Brittany Placek, RN, BSN Presented by Kate Tyner Jessica Trutna, RN, BSN Moderated by Mounica Soma Rebecca Hedstrom, RN, BSN Sharon Conroy, RN, BSN, CIC Panelists: Guidance and responses were provided based on information Dr. Maureen Tierney, MD,MSc known on 4/21/2020 and may become out of date. Guidance is Angie Vasa, RN, BSN being updated rapidly, so users should look to CDC and Kate Tyner, RN, BSN, CIC jurisdictional guidance for updates. Ishrat Kamal-Ahmed, M.Sc., Ph.D Margaret Drake, MT(ASCP),CIC Teri Fitzgerald RN, BSN, CIC
Margaret Woeppel Nebraska Hospital Association https://leadingagene.org/
COVID-19 Preparation, Processes, and Challenges Brittany Placek RN, BSN Crete Area Medical Center Health Service Coordinator Infection Preventionist
COVID-19 Preparation • PPE Donning and Doffing training was mandatory • Hot and cool zones identified for donning and doffing • COVID-19 mock code training in ED • Incident Action Plan • Currently 26 pages and sent to staff M-F with updates managed by our IP • Updates are called out in RED • Covers many topics and a hyperlink table of contents makes it easy to navigate • It is our source of truth • Weekly meetings with community stake holders • Communication with large employers in our area • Communication with Long Term Care facilities planned • Supplies are monitored and reported out twice a week
New Processes Due to COVID-19 • Alternative ways to see and treat patients • Telephone or Tele-health visits for clinic patients who meet criteria • ED Triage in vehicle vs in hospital who meet criteria • Drive up INR nurse visits • Drive up COVID testing • All employees are to wear a mask (N95 or surgical) at all times while in our building (including off-site clinics and business office) • All employees who are in clinical areas are required to wear eye protection (glasses, goggles, face shield) as well • All employees are to take their temperature daily as well as monitor for symptoms • This is submitted to employee health every week with abnormal temperatures or symptoms reported ASAP • Anyone who enters our facility is screened for symptoms and temperature. • This includes patients, EMS workers, approved support persons, vendors • Implemented a no visitor policy with minimal exceptions • Delivering mother – 1 support person for entire stay • Minor child – 1 support person for entire stay • Adult needing support/assistance - 1 support person for entire stay • No visitors for any positive or suspected COVID-19 patients • Anyone who enters the building is to wear a mask • Patients with respiratory illness are given surgical mask • All other individuals are given a cloth or 3D printed mask
Challenges • Access to PPE • Looking at other options to obtain PPE • Donations, purchasing outside normal vendors, local health department, etc. • Limiting PPE use with patients who have non-COVID infections • Only gowning when contact with patient is likely (i.e. transferring/repositioning a patient) • Extended use/re-use of PPE that is normally not re-used • Finding a safe way to do so without contaminating our staff • Communication • Updates are sent out daily in Incident Action Plan. • Leadership has set expectation that staff are required to read the Incident Action Plan and daily updates. • Testing • This has always been a changing piece, first it was access to testing, currently it is access to swabs. • Working with commercial labs and NPHL/LHD to obtain swabs • Access to other essential supplies • Hand sanitizer, soap, oxicide cleaning solution, cleaning wipes, etc. • Receiving donations for some of these supplies (schools, businesses, etc.) • Removed hand sanitizer where a sink is available • Using cleaning solution vs cleaning wipes where appropriate
COVID-19 Response Jessica Trutna, RN, BSN Hospital Nurse Manager/ Trauma Coordinator 16 BEDS, 60 LTC, Rural Health Clinic (7 providers), MS Clinic (2 Providers), Surgery, Specialty clinic (25 specialists), etc. Saunders Medical Center
SMC COVID-19 Response • SMC started really being on alert when Camp Ashland was going to house quarantined COVID-19 individuals (in January) • Never did directly impact us • End of February • Started discussions with EMS- PPE, potential patients, how test results will be communicated • Really started to dive into make sure we had correct cleaning supplies and looking at PPE • Closely monitored patients coming into clinic and ED with respiratory symptoms and asking them to mask • Donning and Doffing education taking place • Upon scheduling appointment in clinic, asked about travel history and symptoms to “flag” chart
SMC COVID-19 Response • March • March 4 th - providers and public health held a community forum at local school • Started our Coronavirus Team meeting daily to plan and prepare for COVID-19 in our facility (in the last 2 weeks we have changed this to M-W-F) • Send out daily updates for all staff from meetings (still continue to do) • First Responders and Healthcare work shop with Three Rivers Public Health • Worked on lab processes (change multiple times initially) • Managing PPE, hand sanitizer, and cleaning supplies- continuous! • Phone triage with Nurse Care Line- developed an algorithm approved by medical staff, who can stay home and who should come in to be tested (changed multiple times) • Early March, we had implemented no visitors in our LTC facility in order to protect our most vulnerable population • Also masked anyone who may come into contact with resident outside of LTC such as in ED • Mid March did a facility and county officials forum for updates
SMC COVID-19 Response • March Continue: • Latter half of March- worked on surge of patients to ED plan (change multiple times). Only have one negative room in facility and it is in the ED • Developed a “path” for COVID patients brought in by EMS • Started thinking about how we will take care of the critical patients while waiting for beds • Mid March started having providers record videos to put on social media for our community- we do 2-4 recordings a week depending on changes • Hired temporary PRN help for departments in need of extra staff (college students mostly) • April • Drive thru testing with our Rural health clinic for high risk individuals • Turned OR’s (2) into negative rooms for patient surge • Cross trained surgery and clinic nurses in hospital and ED patient care • Developed critical care pathways and policies for potential patients waiting beds in large facilities • Immediate critical care education to nurses and providers • Telehealth for rural health clinic patients
SMC COVID-19 Response Drive thru testing
SMC COVID-19 Response • Summary • We have 7 confirmed cases here in Saunders County. • Testing- We have utilized our phone triage, drive thru testing, and Three Rivers Public Health guidance • Most patients, if not in the high risk group (inpatients, HCW, LTC, First Responders, or from group homes), we tell them to self isolate for 14 days • We have limited test kits in our facility so need to reserve them for high risk individuals • Continue to monitor temperatures and symptoms of staff, patients, and residents • Continue to follow latest guidance from CDC and public health
COVID-19 Response Brodstone Memorial Hospital Rebecca Hedstrom, RN, BSN
• Established Team • Key Players: Leadership, Department Managers, Frontline • Incident Command Team • Plan • Clinics (3) • Surgery • Outpatient • Emergency Room • Hospital • Worked the Plan • Revised the Plan
Team Success • Team Approach • Early Planning and Process’s Developed • Referral Pathways • Telehealth • Employee Morale • Communication • Internal • daily emails, safety huddle, provider meetings • External • newspaper, radio, social media
Challenges • Facility • Negative Pressure Rooms*** • ER • Clinic • Lab Send out • RPP • Timely • PPE • Conserve elective surgeries, colonization MRSA, cloth mask vs surgical mask • UV Light • Nursing Home Referrals
COVID Preparedness Sharon Conroy, RN, BSN Community Hospital McCook
• Started incident command on March 6 th • Started screening all patients on March 14 • Allowing no visitors in facility except advocate • All staff self monitoring • Looked ahead for an additional assessment site • Controlled access into facility
• Had an CEO open forum for staff to come as ask questions • Rolled out glove hygiene for clinical staff staff. • Stopped using disposable isolation gowns and Started using reusable isolation gowns instead of disposable – quarantined masks • Partnered with area nursing homes and assisted living (donated money to aide cache) • Started a community cache to aid facilities • Worked with volunteers to make masks for patients and non clinical staff
• Purchased two UV boxes to help in UV disinfection or N95 masks if needed • Partnered with SWPHD and did several radio spots • Making our own hand sanitizer • Mandatory mask wearing of all staff April 13 • All staff that can work from home out of building starting April 13 • Limited travel for work and personal reasons early on in outbreak
Recommend
More recommend