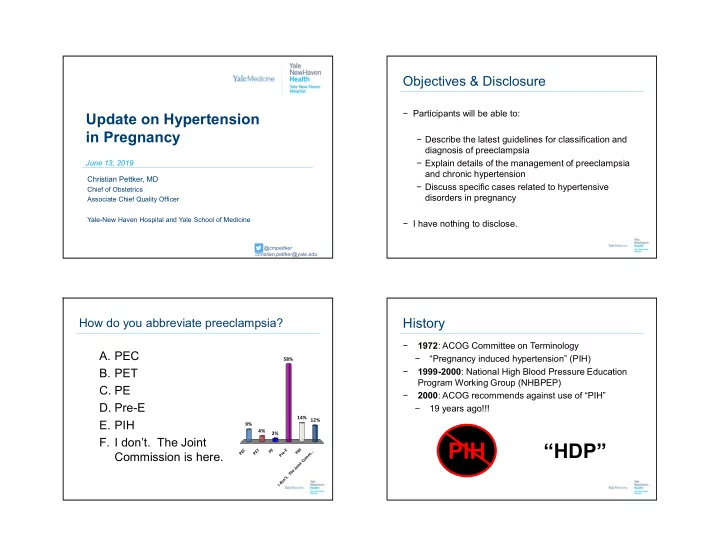
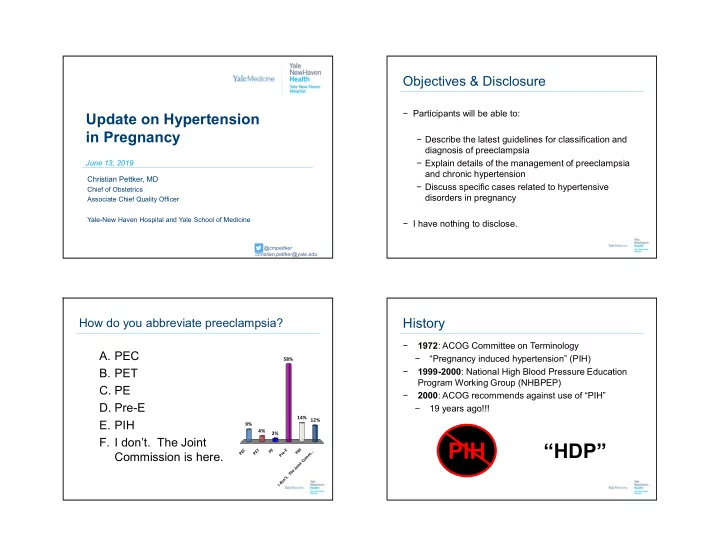
Objectives & Disclosure − Participants will be able to: Update on Hypertension in Pregnancy − Describe the latest guidelines for classification and diagnosis of preeclampsia − Explain details of the management of preeclampsia June 13, 2019 and chronic hypertension Christian Pettker, MD − Discuss specific cases related to hypertensive Chief of Obstetrics disorders in pregnancy Associate Chief Quality Officer Yale-New Haven Hospital and Yale School of Medicine − I have nothing to disclose. @cmpettker christian.pettker@yale.edu How do you abbreviate preeclampsia? History − 1972 : ACOG Committee on Terminology A. PEC − “Pregnancy induced hypertension” (PIH) 58% B. PET − 1999-2000 : National High Blood Pressure Education Program Working Group (NHBPEP) C. PE − 2000 : ACOG recommends against use of “PIH” D. Pre-E − 19 years ago!!! 14% 12% E. PIH 9% 4% 2% F. I don’t. The Joint PIH “HDP” PEC PET PE Pre-E PIH I don’t. The Joint Comm... Commission is here.
January 2019 2013: ACOG Hypertension in Pregnancy Task Force − “With severe features” − Urine protein/creatinine ratio − Outpatient mgmt. of GHTN + PEC − Gest HTN: deliver 37w − CHTN: deliver 38w (or later) − PEC with severe features: − 105 mm Hg diastolic − BP 4 hours apart − Serum creat ≥1.1 (or 2x nl) − FGR not in criteria − Magnesium not universally needed − Low dose ASA for prevention − No NSAIDs! 6 “HDP”: A leading cause of morbidity/mortality “HDP”: A quality of care problem − A leading cause of morbidity/mortality − Preeclampsia: 2-8% of pregnancies globally − 25% increase in US from 1987 to 2004 − Approximately 50% of mortalities are considered preventable − Chronic HTN: 0.9-1.5% of pregnancies − Delays in presenting for care − 67% increase from 2000 to 2009 − Missed or misinterpreted clinical information − 16-18% of all maternal deaths in US − Delays in diagnosis − Often misidentified signs/symptoms or other − 15% of premature births in industrialized countries evidence − Delays in therapy − $2.18 billion estimated cost in US for 12 months after delivery ($1.03 billion maternal cost)
What about elevated BP & stage 1 CHTN? Patient #1 Your new OB patient for the day is a cardiology fellow. She is 8 weeks of gestation and she tells you she has a history of stage I hypertension. She reports her blood pressures were as high as 130s/80s last year, when she was diagnosed, and that she started on labetalol 100mg BID, as she was planning a pregnancy. Her blood pressure at intake is 134/82. − What are your thoughts about her blood pressures and their impact on pregnancy? 10 Stage 1 Hypertension (ACC/AHA) Stage 1 Hypertension (ACC/AHA) Keep her on her medications? − Men + women with BP 130-139 SBP or 80-89 DBP have modifiable long-term cardiovascular risk A. Yes 95% B. No − These patients will now be treated; we may see more pregnancies treated as hypertensive - What type of baseline tests? − Sutton et al ONG 2018 − Higher risk of preeclampsia, gestational diabetes, - Surveillance? indicated preterm birth 5% − ASA does not appear to reduce this risk Yes No
2013 Classification System Patient #2 You are following a patient who you diagnosed with 1. Chronic hypertension gestational hypertension at 32 weeks of gestation. You 2. Gestational hypertension have been following her with weekly visits, NSTs, and 3. Preeclampsia laboratory evaluation. Today, at 35 1/7 weeks of gestation, - without severe features she had a blood pressure of 162/100 and was referred to - with severe features the triage unit for further evaluation, revealing 4. Chronic hypertension with superimposed preeclampsia − Repeat blood pressures 164/90 - without severe features − ‘Normal’ creatinine, LFTs, platelets - with severe features − Urine P/C ratio 0.05 − What is your management plan? Gestational Hypertension, with “severe range” BPs Gestational Hypertension, with “severe range” BPs − Point 1: Treat the blood pressure. − Point 2: Treat as preeclampsia with severe features − Magnesium? − Delivery planning? III. M anagement A cute o s e t, e p rs is ten t l ( a s tin g r 5 1 m i n utes o o m r e) e s v ere s ys tolic ( 16 0m m g H r ) o s ev ere dias to l r ic ( 110m m g H ) b l o o d p e s s ure n a i r s p r egn an t o p o t pa r tum w o s ma n i a h yperten s iv e emergency. The ACOG Committee Opinion Number 514 of December 2011 recommends the following algorithm. S ys tolic B P 160mm Hg and /or D ias to li c B P 1 g 1 0mm H − Mode of delivery? Notify Provider IV Antihypertensive Medication Seizure Prophylaxis Labetalol 20 mg. Hydralazine 5-10 mg . Magnesium Sulfate loading dose 4-6 gm over 20 minutes Repeat BP in 20 minutes If above threshold give Repeat BP in 10 minutes Hydralazine 10 mg If above threshold give Labetalol 40 mg Magnesium Sulfate maintenance dose at Repeat BP in 20 minutes 1-2 gm/hour If above threshold give Repeat BP in 10 minutes Labetalol 20 mg If above threshold give Labetalol 80 mg Repeat BP in 10 minutes If above threshold give Labetalol 40 mg AND Repeat BP in 10 minutes Obtain anesthesia consult If above threshold give Hydralazine 10 mg Repeat BP in 20 minutes If remains elevated obtain anesthesia consult Use labetalol with caution in patients with asthma; may cause bronchospasm http://www.safehealthcareforeverywoman.org
Patient #3 Diagnosing Superimposed Preeclampsia − Importance of baseline screening Your patient with essential chronic hypertension has been − Baseline creatinine managed with labetalol her entire pregnancy. She started − Baseline proteinuria on 200mg BID but at 28 weeks her blood pressures were rising above 160/110 and her labetalol increased steadily over time. − Consider pathophysiology of hypertension Today, she is 36 4/7 weeks of gestation and her blood − SLE? Primary Renal? Intoxication? pressure is 180/115. How do tell if this is preeclampsia? − Other labs? − Uric Acid − Hematocrit − Response to treatment Patient #4 What is the utility of urine protein/creatinine ratio? Your patient with chronic hypertension on labetalol 200mg − Protein/creatinine ratio is a spot urine test TID presents is referred by your colleague at 36 3/7 for elevated blood pressures. In triage, BP is 165/95 and − Protein excretion varies during the day when repeated is 155/90. In the first trimester her 24 hour − With activity urine showed 100mg of protein. Given her rise in blood − Especially during pregnancy pressure, you send laboratory tests, including a urine protein/creatinineratio. − < 0.13 to 0.15 very sensitive to rule out preeclampsia UPC comes back at 0.29. What is the utility of this test? Is − Papanna et al ONG 2008 (90-98% sensitivity) this preeclampsia? − Morris et al BMH 2012 (85-93% sensitivity)
Patient #5 Controlled CHTN: delivery at 37w, 38w, or 39w? Your 33 year old nulliparous patient with chronic hypertension is 34 weeks of gestation and seeing you for a routine prenatal visit. Her blood pressure has been well controlled on labetalol 200mg BID her whole pregnancy. Her baseline studies (EKG, urine protein, serology/hematology) were all normal. She has been ACOG CO 764 having normal weekly testing and fetal ultrasounds, including She is asking about her delivery plan. When do you deliver? 45% 43% A. 37 weeks B. 38 weeks C. 39 weeks 12% D. 40 weeks? 0% s s s ? k k k s e e e k e e e e e w w w w 7 8 9 3 3 3 0 4 Controlled CHTN: delivery at 37w, 38w, or 39w? Patient #6 Your patient has just delivered by cesarean. She had two − Planned delivery prior to 39w is associated with a lower prior cesareans and was 35 weeks of gestation, with risk of developing preeclampsia with severe features preeclampsia with severe features. She is on magnesium − 10% v. 1% absolute risk (adj OR 0.07, 95%CI 0.01-0.5) for seizure prophylaxis. Your nurse is asking what you − Harper LM. ONG 2016 (retrospect cohort) would like to give for pain control. 62% What is your approach? − Routine induction 38w vs. 39w lowers risk of 38% superimposed PEC and eclampsia, with no increased risk A. Routine (NSAIDs/Tylenol/Oxycodone) of CD B. Anything but NSAIDs − Ram M. ONG 2018 (retrospective cohort) . s . D . o I A n S e N l y T t u / b s D g I n A i S h N t y ( n e A n i t u o R
“I can’t give my patient NSAIDs?” ACOG Task Force (2013) ACOG PB 203 (2019) “Overall, data support the safe use of NSAIDs in postpartum patients with blood pressure issues.” − RCT of ibuprofen v. acetaminophen in preeclampsia with severe features: no prolongation of severe-range blood pressures (Blue NR et al. AJOG 2018) − Cohort study of 399 patients with preeclampsia with severe features; no difference in hypertensive episodes, renal injury, ICU admission, pulmonary edema (Viteri OA et al ONG 2017) − Cohort study of postpartum patients on magnesium for preeclampsia; no increased antihypertensive requirements. (Wasden SW et al Pregnancy Hypertens 2014) 26 http://tmedweb.tulane.edu/pharmwiki/doku.php/nsaid_side_effects
Recommend
More recommend