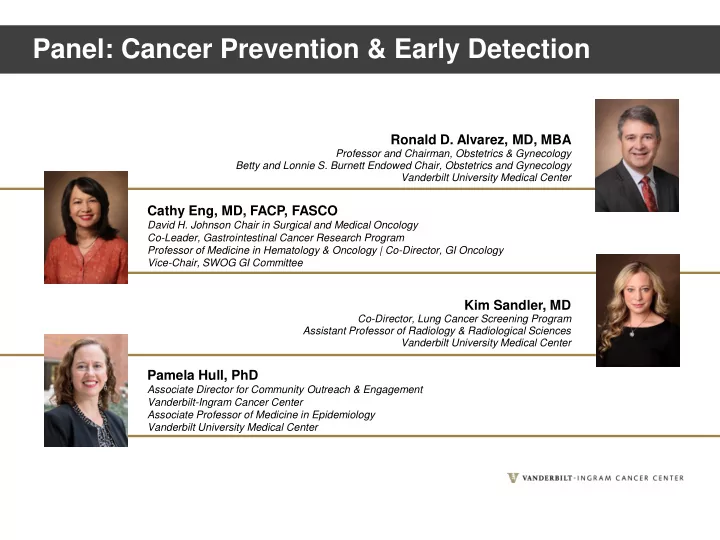
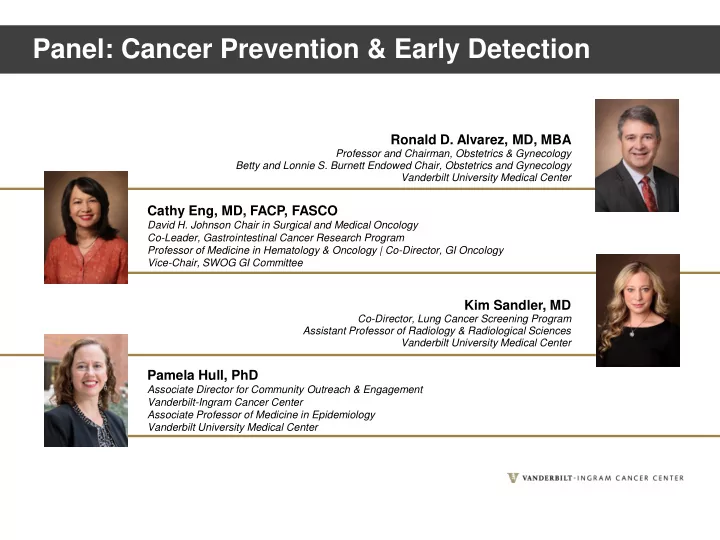
Panel: Cancer Prevention & Early Detection Ronald D. Alvarez, MD, MBA Professor and Chairman, Obstetrics & Gynecology Betty and Lonnie S. Burnett Endowed Chair, Obstetrics and Gynecology Vanderbilt University Medical Center Cathy Eng, MD, FACP, FASCO David H. Johnson Chair in Surgical and Medical Oncology Co-Leader, Gastrointestinal Cancer Research Program Professor of Medicine in Hematology & Oncology | Co-Director, GI Oncology Vice-Chair, SWOG GI Committee Kim Sandler, MD Co-Director, Lung Cancer Screening Program Assistant Professor of Radiology & Radiological Sciences Vanderbilt University Medical Center Pamela Hull, PhD Associate Director for Community Outreach & Engagement Vanderbilt-Ingram Cancer Center Associate Professor of Medicine in Epidemiology Vanderbilt University Medical Center
Cervical Cancer Screening Ronald D. Alvarez, MD, MBA Vanderbilt University Medical Center
Cervical Cancer Stats Cases Deaths US (2020) 13,800 4,290 World (2018) 569,800 311,400 Cancer Statistics, 2020 Global Cancer Facts and Figures, 2018
Cervical Cancer in US Cervical cancer death rates, 2016 Cervical cancer incidence rates, 2016
Screening has Reduced Cervical Cancer Mortality in the US 5 Singh J Community Health 2012
2018 USPSTF Cervical Cancer Screening Guidelines • Women < age 21 – No screening indicated • Women age 21-29 – Cervical cytology every 3 yrs • Women age 30-65 – Cervical cytology every 3 yrs – hrHPV testing every 5 yrs – Cervical cytology/HPV co-testing every 5 yrs • Women > age 65 – Discontinue with adequate prior screening and no prior CIN 2 or greater • Post hysterectomy – Discontinue screening if for benign indication and no prior CIN 2 or greater USPSTF, JAMA, 2018
Challenges with Cervical Cancer Screening in Rural and Underserved Populations • So many other higher priority concerns • Poor knowledge of risks for cervical and other HPV associated cancers • Noncompliance with cervical cancer screening (and HPV vaccination) recommendations • Lack of alternative and more convenient screening strategies
Enhancing Cervical Cancer Screening in Rural and Underserved Populations • Address basic human needs • Enhance education and communication • Engage community health advisors • Employ self testing strategies • Utilize alternative strategies (i.e. VIA, VILI) • Move from opportunistic to organized screening in most vulnerable populations
Make Cervical Cancer Screening Irrelevant – Vaccinate!
Questions?
Recommend
More recommend