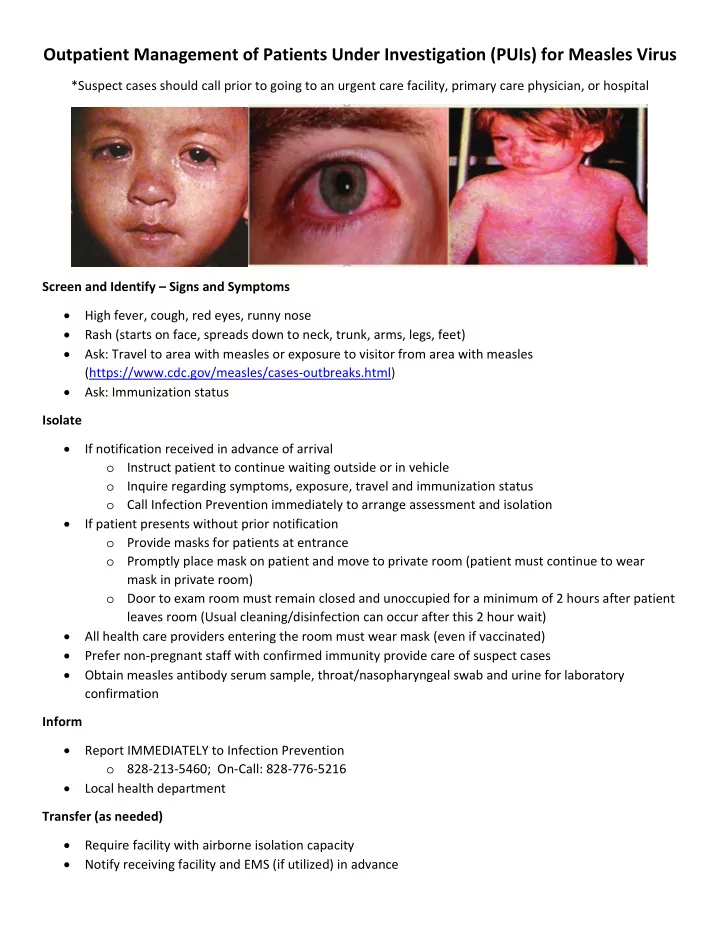
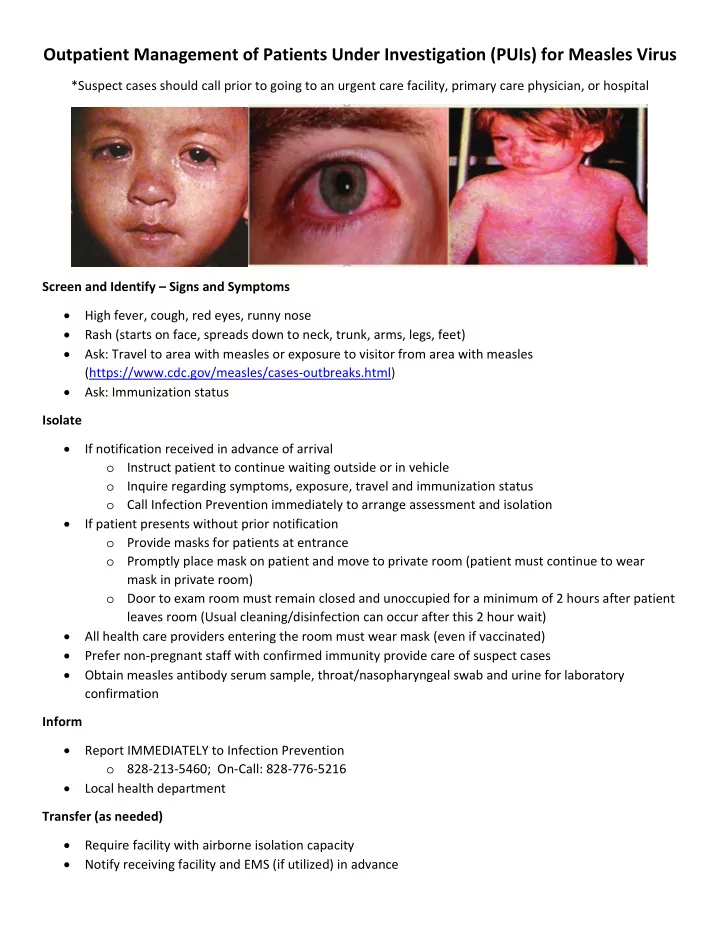
Outpatient Management of Patients Under Investigation (PUIs) for Measles Virus *Suspect cases should call prior to going to an urgent care facility, primary care physician, or hospital Screen and Identify – Signs and Symptoms High fever, cough, red eyes, runny nose Rash (starts on face, spreads down to neck, trunk, arms, legs, feet) Ask: Travel to area with measles or exposure to visitor from area with measles (https://www.cdc.gov/measles/cases ‐ outbreaks.html) Ask: Immunization status Isolate If notification received in advance of arrival o Instruct patient to continue waiting outside or in vehicle o Inquire regarding symptoms, exposure, travel and immunization status o Call Infection Prevention immediately to arrange assessment and isolation If patient presents without prior notification o Provide masks for patients at entrance o Promptly place mask on patient and move to private room (patient must continue to wear mask in private room) o Door to exam room must remain closed and unoccupied for a minimum of 2 hours after patient leaves room (Usual cleaning/disinfection can occur after this 2 hour wait) All health care providers entering the room must wear mask (even if vaccinated) Prefer non ‐ pregnant staff with confirmed immunity provide care of suspect cases Obtain measles antibody serum sample, throat/nasopharyngeal swab and urine for laboratory confirmation Inform Report IMMEDIATELY to Infection Prevention o 828 ‐ 213 ‐ 5460; On ‐ Call: 828 ‐ 776 ‐ 5216 Local health department Transfer (as needed) Require facility with airborne isolation capacity Notify receiving facility and EMS (if utilized) in advance
ASSESSMENT OF SUSPECTED MEASLES CASES Given the recent increase in the number of suspected measles calls, The NC Communicable Disease Branch (CDB) wanted to share general criteria for evaluation that may be useful to you when assessing whether measles testing should be approved by CDB for testing at the NC State Laboratory of Public Health (SLPH). Approval is required and must be discussed with the Epidemiologist On Call at 919 ‐ 733 ‐ 3419. Testing is reserved for those cases most likely to have measles (such as unvaccinated travelers) or those with fever and generalized maculopapular rash with strong suspicion of measles. Because approving testing indicates that we have a strong suspicion for measles, it also often indicates the need to implement control measures (isolating suspected cases, identifying contacts, assessing for evidence of immunity, and implementing quarantine and post exposure prophylaxis (PEP) if indicated. In most circumstances, testing should not be approved for patients with no known risk factors for measles (such as fully ‐ immunized NC residents with no travel history). Consider these factors when determining the level of suspicion for measles: 1. Immune Status – Persons who meet the criteria for acceptable evidence of immunity (described below) have a very high likelihood of immunity and are unlikely to acquire measles. Measles vaccine is highly effective [1 dose: 93%, 2 doses: 97%] and is believed to produce life ‐ long immunity. Evidence of immunity includes: a. History of age ‐ appropriate vaccination, b. Birth before 1957 in the United States, or c. Laboratory evidence of immunity. 2. Exposure History – Inquire about potential sources of infection in the 21 days prior to onset such as: a. International travel, b. Domestic travel to locations with known cases, c. Contact with persons with similar symptoms, or d. Contact with known or suspected cases. 3. Clinical Picture – Consider if the clinical picture is compatible with measles and if the case definition is met. a. Prodrome: i. High fever (stepwise increase, can be up to 105 ⁰ ) ii. Cough, coryza, conjunctivitis iii. Koplik spots (tiny white spots in the mouth with bluish ‐ white centers) b. Rash (usually 14 days after exposure): i. Begins a few days after onset prodrome ii. Maculopapular rash begins on face and head iii. Spreads to trunk and then extremities (downward and outward) iv. Fades in order of appearance 4. Other Causes – Consider other possible causes for the illness. Inquire about: a. Recent use of antibiotics, b. Contact with cases of rash illness with known etiology (e.g. parvovirus or fifths disease, coxsackie or hand, foot and mouth disease, roseola or humanherpes virus 6 ‐ 7, strep or scarlet fever), and c. Other testing that was performed (RMSF). The local health department investigation steps for measles are available in the CD Manual. Other materials, such as post ‐ exposure prophylaxis guidelines, isolation and quarantine information and templates are also available if needed. Vaccine Preventable Disease Program NC Communicable Disease Branch Rev. 02122019
ROY COOPER • Governor MANDY COHEN, MD, MPH • Secretary DANNY STALEY • Director, Division of Public Health SCOTT J. ZIMMERMAN, DrPH, MPH, HCLD (ABB) • Laboratory Director, State Laboratory of Public Health NCSLPH Measles Specimen Collection and Testing Guidelines, 6/25/2018 Testing Criteria for Measles: All suspect or probable cases of measles must be reported to the Communicable Disease Branch at (919) 733-3419 for prior approval for laboratory testing . Individuals presenting with fever, cough, coryza and/or conjunctivitis, and a rash are considered suspect cases. Testing Systems Employed: Serological specimens will be evaluated at the NCSLPH using an Indirect Immunofluorescent Antibody (IFA) test to detect IgM and IgG antibody. Nasopharyngeal (NP) swabs, throat swabs, and urine will be processed for viral isolation and PCR analysis at the NCSLPH. SPECIMENS SHOULD BE COLLECTED AT THE FIRST CONTACT WITH A SUSPECTED CASE Specimen Test Specimen Shipment Expected TAT Volume Serum* IgM and IgG IFA 1 – 3 ml Refrigerated (4°), place 1 – 2 days on cold packs NP or Viral Culture** 2ml VTM Refrigerated (4°), place Culture: 1 - 2 Throat PCR on cold packs weeks Swab PCR: 3 days Urine Viral Culture** 15 ml (20 – Refrigerated (4°), place Culture: 1 - 2 PCR 35 ml on cold packs weeks preferred) PCR: 3 days *Note: Optimal collection for this specimen type is >3 days post-onset of rash. Collection prior to this time may result in a false negative test due to the lack of detectable levels of IgM and IgG immunoglobulin. **Note: Measles virus isolation is most successful when samples are collected on the first day of rash through 3 days following onset of rash; however, it is possible to detect virus up to day 7 following rash onset. SPECIMEN COLLECTION AND STORAGE • Collection instructions for viral culture: Nasopharyngeal Swab – Carefully swab the posterior nasopharyngeal area via the external nares with a dry sterile tipped swab. Break off the swab tip into a vial containing 2 ml of viral transport medium. Screw the cap on tightly. NC DEPARTMENT OF HEALTH AND HUMAN SERVICES • DIVISION OF PUBLIC HEALTH • STATE LABORATORY OF PUBLIC HEALTH LOCATION: 4312 District Drive, Raleigh, NC 27607 MAILING ADDRESS: 1918 Mail Service Center, Raleigh, NC 27699-1918 www.ncdhhs.gov • http://publichealth.nc.gov • slph.ncpublichealth.com • TEL: 919-733-7834 • FAX : 919-733-8695 AN EQUAL OPPORTUNITY / AFFIRMATIVE ACTION EMPLOYER
Throat Swab – Vigorously rub the posterior wall of the pharynx with a dry, sterile, swab. The swab should not touch the tongue or buccal mucosa. Break off the swab tip into a vial of viral transport medium. Screw the cap on tightly. Urine: Collect clean voided urine. Transfer to a plastic shipping tube. • All specimen types should be refrigerated promptly after collection. Temporary storage and transport temperature should be 4° - 8°C. DO NOT FREEZE. • Clearly label each specimen with patient's first and last name, either date of birth, SSN, or other unique identifier, specimen source, and collection date. • Complete the appropriate specimen submission forms and request Measles testing only during times of active Measles surveillance : - Serological specimens: DHHS# 3445, found at http://slph.ncpublichealth.com/Forms/DHHS-3445-SpecialSerology-20130809.pdf Include the statement: “Prior approval/consultation received from:” the name of the individual in the Communicable Disease Branch that provided approval for testing. - Swabs and urine for culture: DHHS# 3431, found at http://slph.ncpublichealth.com/Forms/DHHS-3431-Virology-20130809.pdf • Do not use calcium alginate tipped OR wooden shafted swabs. Calcium alginate may inactivate some viruses. Wooden shafts may be toxic to viruses. SHIPPING OF DIAGNOSTIC SPECIMENS (PLEASE NOTE THE CHANGE OF ADDRESS) • Ship specimen(s) to the State Laboratory the same day collected. • Wrap the properly labeled inoculated transport medium (primary container) or serological specimen in absorbent material, i.e. paper towel, and place into a leak proof secondary container (50ml conical tubes). • Place two frozen ice packs in the shipping container. • Place secondary container(s) containing specimen(s) between the ice packs. • Place completed forms in plastic bag and slide into space at narrow end of ice pack. • Ship specimens to: Attention: Virology/Serology North Carolina State Laboratory of Public Health 4312 District Drive Raleigh, NC 27607-5490 • Ship specimens by the fastest means possible. Transit time of less than 24 hours will optimize virus detection. Please contact John Bunting (919-807-8824) or Segun Awe (919-807-8821) at the NCSLPH if you have questions regarding sample collection or shipment. 2
Recommend
More recommend