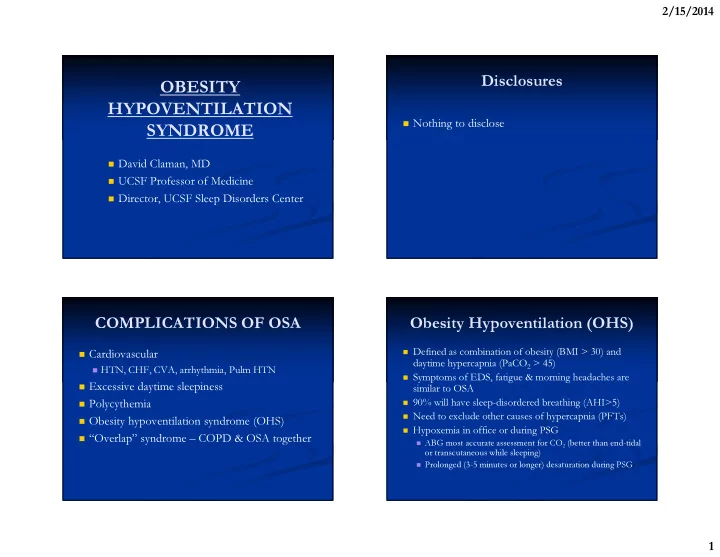
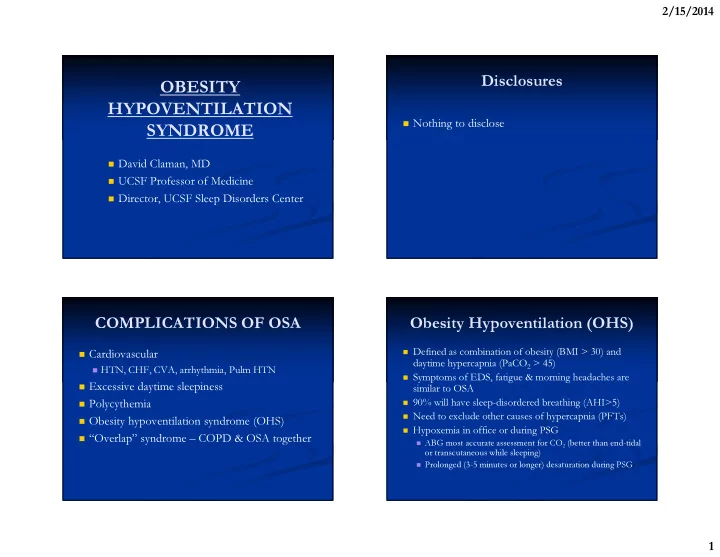
2/15/2014 Disclosures OBESITY HYPOVENTILATION � Nothing to disclose SYNDROME � David Claman, MD � UCSF Professor of Medicine � Director, UCSF Sleep Disorders Center COMPLICATIONS OF OSA Obesity Hypoventilation (OHS) � Defined as combination of obesity (BMI > 30) and � Cardiovascular daytime hypercapnia (PaCO 2 > 45) � HTN, CHF, CVA, arrhythmia, Pulm HTN � Symptoms of EDS, fatigue & morning headaches are � Excessive daytime sleepiness similar to OSA � 90% will have sleep-disordered breathing (AHI>5) � Polycythemia � Need to exclude other causes of hypercapnia (PFTs) � Obesity hypoventilation syndrome (OHS) � Hypoxemia in office or during PSG � “Overlap” syndrome – COPD & OSA together � ABG most accurate assessment for CO 2 (better than end-tidal or transcutaneous while sleeping) � Prolonged (3-5 minutes or longer) desaturation during PSG 1
2/15/2014 INCREASED MORTALITY IN OHS HYPERCAPNIA IN OSA � If untreated, approx 23% mortality at 1-1.5 yrs � French Multicenter Study; n=1141 from database � Treated with NPPV: mortality 3% at 1.5 yrs � Excluded those with FEV1<80% Mokhlesi B et al. Proc Am Thorac Soc 2008(5):218-225 � � Overall prevalence of 11% with PaCO 2 >45 � BMI < 30 – prevalence 7.2% � BMI 30-40 – prevalence 9.8% � BMI > 40 – prevalence 23.6% � Laaban J-P et al. Chest 2005;127:710-715 Increased Risk with Higher BMI Oxygen in OHS � Patients treated with � Data from USA, France and Italy NIV + O2 had higher � Mokhlesi B et al. Chest 2007;132:1322-1336 mortality than NIV alone, possibly due to worse underlying disease (Priou; Chest 2010;138:84) � Experimentally, 100% Oxygen while awake causes 5 mm Hg increase in TcCO2 (Wijeinghe Chest 2011;139:1018) 2
2/15/2014 DDx of Hypercapnia Olson AL & Zwillich C; Am J Med 2005;118:948- Limitation to ventilation – CAN’T BREATH � 956 � Restrictive lung disease from morbid obesity � Chest wall diseases � Neuromuscular diseases � Obstructive lung disease Central Control - WON’T BREATH � � Congenital Central Hypoventilation (Ondine’s curse) � PHOX2B mutation on chromosome 4p12 � Brainstem lesions � Carotid body disease � Metabolic alkalosis Combined defect � � COPD � Hypothyroidism � Sleep Apnea OHS: A SPECTRUM OF RESPIRATORY ABNORMALITIES � OSA with apneas and hypopneas � Sleep hypoventilation especially in REM � Prolonged obstructive hypoventilation due to partial upper airway obstruction � Overlap of pulmonary disease with ventilatory sleep disturbance � Berger KI et al. Chest 2001;120:1231-1238 3
2/15/2014 TREATMENT OF OHS CPAP & BILEVEL FOR OHS � Spanish retrospective analysis of 54 patients (18 women) � Weight loss – consider bariatric surgery with OHS; mean BMI 44 (Perez de Llano LA et al. Chest 2005;128:587-594) � CPAP for OSA patients with only mildly � OSA (AHI > 5) present in 87% elevated PaCO 2 � Overall, all patients had improved PaCO 2 and PaO 2 on treatment; 5 weaned from treatment after weight loss � Bilevel or non-invasive ventilation essential if � Modality When discharged Outpt f/u significant hypercapnia is present � CPAP 3 16 � Improved ventilation control in 4-6 days � Bilevel 49 30 � Berthon-Jones M et al. Am Rev Respir Dis 1987;135:144-7 � Volume ventilator 2 3 � Progesterone treatment remains inconsistent � Oxygen 47 31 RCT of NPPV for Mild OHS CONCLUSIONS � One month of NIV improved sleep and blood gases, but did not change inflammatory (hsCRP, Leptin, RANTES, MCP1, IL6, IL8, TNFα), metabolic (adiponectin, IL1-RA) and cardiovascular markers � OHS complicates 10-15% of OSA patients ( Borel J-C et al. Chest 2011;10:2531) � OHS has higher mortality risk if untreated � Risk of OHS increases with higher BMI � OHS represents a spectrum of ventilatory disturbances � Basic treatment should usually focus on weight loss and bilevel treatment with oxygen if needed 4
Recommend
More recommend