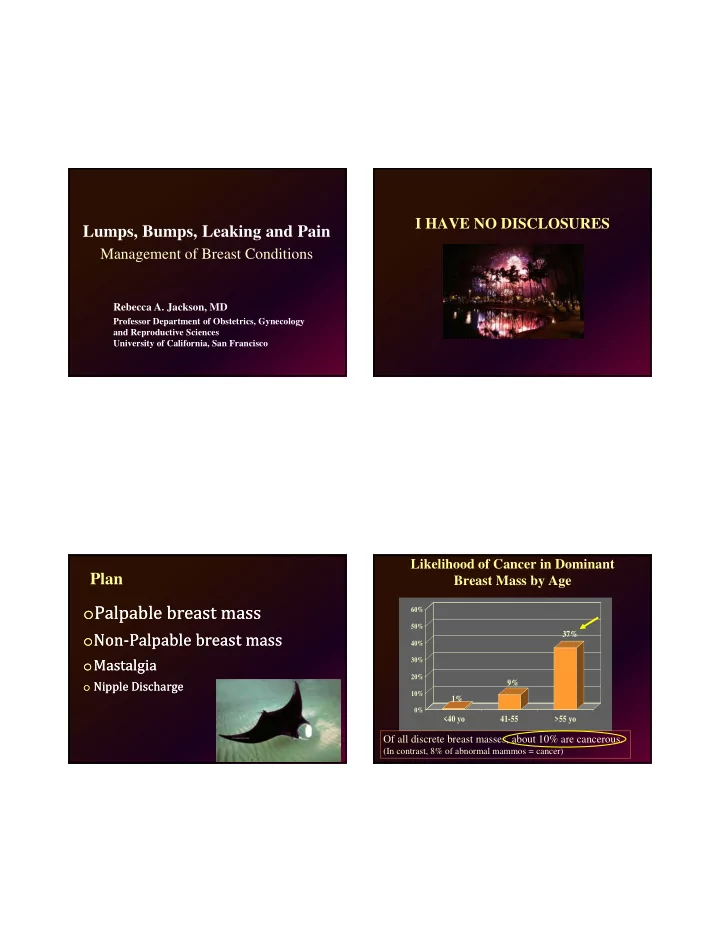
I HAVE NO DISCLOSURES Lumps, Bumps, Leaking and Pain Management of Breast Conditions Rebecca A. Jackson, MD Professor Department of Obstetrics, Gynecology and Reproductive Sciences University of California, San Francisco Likelihood of Cancer in Dominant Plan Breast Mass by Age o Palpable breast mass o Palpable breast mass 60% 50% o Non‐Palpable breast mass o Non‐Palpable breast mass 37% 40% o Mastalgia o Mastalgia 30% 20% o Nipple Discharge o Nipple Discharge 9% 10% 1% 0% <40 yo 41-55 >55 yo Of all discrete breast masses, about 10% are cancerous. (In contrast, 8% of abnormal mammos = cancer)
Failure to diagnose breast cancer “Dominant Mass”? in a timely manner is a leading o Discrete or dominant mass= stands out cause of malpractice claims from adjoining breast tissue, definable borders, is measurable, not bilateral. Common reasons: Common reasons: o Unimpressive o Unimpressive o Nodularity or thickening = ill‐defined, physical findings physical findings often bilateral, fluctuates with menstrual o Failure to f/u with pt o Failure to f/u with pt cycle o Palpable mass with o Palpable mass with o In women <40 referred for mass, only negative mammo negative mammo 1/3 had confirmed dominant mass Question 1 Breast Mass: Diagnostic Options A 42 yr old woman with no family or A 42 yr old woman with no family or o Physical exam o Physical exam personal history of breast cancer has personal history of breast cancer has o Ultrasound o Ultrasound found a breast lump. She doesn’t know found a breast lump. She doesn’t know o Diagnostic Mammogram o Diagnostic Mammogram how long it has been there. It is not how long it has been there. It is not o Digital Breast Tomosynthesis (DBT) o Digital Breast Tomosynthesis (DBT) painful. painful. o Cyst aspiration o Cyst aspiration On exam, it is a discrete mass, 2 cm, On exam, it is a discrete mass, 2 cm, o Fine needle aspiration o Fine needle aspiration relatively smooth, mobile and non‐tender. relatively smooth, mobile and non‐tender. She has no axillary lymphadenopathy. She has no axillary lymphadenopathy. o Core needle biopsy o Core needle biopsy What is your next step? What is your next step? o Excisional biopsy o Excisional biopsy
Q1: Palpable mass in 42 yo Q1b: Palpable mass in 42 yo Next step (pick one)? Next step (pick one)? A mammography was chosen and is A mammography was chosen and is A. Nothing now. Re‐examine in 1‐2 months A. Nothing now. Re‐examine in 1‐2 months negative. Next step (pick one)? negative. Next step (pick one)? B. Ultrasound B. Ultrasound A. Re‐examine in 1‐2 months A. Re‐examine in 1‐2 months C. Digital Mammography C. Digital Mammography B. F/u 1 year for annual exam B. F/u 1 year for annual exam D. DBT: Digital Breast Tomosythesis D. DBT: Digital Breast Tomosythesis C. Ultrasound C. Ultrasound E. Office aspiration E. Office aspiration D. Office aspiration D. Office aspiration F. FNAB (fine needle aspiration biopsy) F. FNAB (fine needle aspiration biopsy) E. FNAB E. FNAB G. Core biopsy G. Core biopsy F. Core biopsy F. Core biopsy Q1c: Palpable mass in 42 yo Step 1: Palpable Breast Mass An ultrasound was chosen as the first step. An ultrasound was chosen as the first step. o Determine if mass is cystic or o Determine if mass is cystic or It shows a cystic mass. Next step? It shows a cystic mass. Next step? solid solid A. Re‐examine in 1‐2 months A. Re‐examine in 1‐2 months B. F/u 1 year for annual exam B. F/u 1 year for annual exam o Simple cysts are benign and don’t o Simple cysts are benign and don’t require further evaluation require further evaluation C. Standard diagnostic mammogram C. Standard diagnostic mammogram o 20‐25% of palpable masses are simple o 20‐25% of palpable masses are simple D. DBT (digital breast tomosynthesis) D. DBT (digital breast tomosynthesis) cysts, most occurring in 40‐49 yo’s cysts, most occurring in 40‐49 yo’s E. Office aspiration E. Office aspiration o Options?: Ultrasound, office aspiration, FNA, o Options?: Ultrasound, office aspiration, FNA, F. FNA F. FNA core needle biopsy core needle biopsy G. Core biopsy G. Core biopsy
Breast Exam Ultrasound o Nether sensitive (50‐60%) nor specific (60‐ o Nether sensitive (50‐60%) nor specific (60‐ o Primary Use: Classify mass as cystic or solid o Primary Use: Classify mass as cystic or solid 90%) (even when done by experts) 90%) (even when done by experts) o Also can help to further classify mass via Bi‐ o Also can help to further classify mass via Bi‐ o Cannot reliably distinguish cyst from solid (58% o Cannot reliably distinguish cyst from solid (58% Rads system for sono‐‐ but much less data on Rads system for sono‐‐ but much less data on accuracy) accuracy) risk of cancer assoc with each classification risk of cancer assoc with each classification o Not reliable for determining if biopsy needed o Not reliable for determining if biopsy needed o Guidance for cyst aspiration or biopsy o Guidance for cyst aspiration or biopsy o Nonetheless, it is important for determining if o Nonetheless, it is important for determining if mass is discrete (vs nodularity or thickening) mass is discrete (vs nodularity or thickening) o Adjunct to evaluate symmetric densities o Adjunct to evaluate symmetric densities and for follow‐up of masses and for follow‐up of masses detected by mammography detected by mammography o Perform in 2 positions, methodical, spirals or strips o Perform in 2 positions, methodical, spirals or strips o Can be the first test performed & if cyst is o Can be the first test performed & if cyst is o Mark mass prior to biopsy so others can find it o Mark mass prior to biopsy so others can find it confirmed—the only test required confirmed—the only test required Cyst Aspiration Fibroadenoma Cancer Cyst o Simple office procedure: 20‐23 gauge needle o Simple office procedure: 20‐23 gauge needle and syringe, ultrasound guidance optional, and syringe, ultrasound guidance optional, specialized training not necessary specialized training not necessary o Primary Use: Confirm mass is cystic o Primary Use: Confirm mass is cystic o Secondary use: Relieve pain/pressure due to o Secondary use: Relieve pain/pressure due to symptomatic cyst symptomatic cyst Anechoic, well- circumscribed, Well-circumscribed, Irregular, deep o Benefits: If cystic fluid obtained, establishes o Benefits: If cystic fluid obtained, establishes superficial immediate diagnosis and provides immediate diagnosis and provides Ultrasound is 98-100% accurate for diagnosis of simple cysts. symptomatic relief symptomatic relief However, for solid masses, it cannot reliably distinguish benign from malignant.
Cyst Aspiration (cont’d) Adequate/reassuring if: Adequate/reassuring if: 1. Cyst fully collapses (no residual mass) 1. Cyst fully collapses (no residual mass) 2. Fluid is not brown/red (cloudy ok) 2. Fluid is not brown/red (cloudy ok) 3. Does not re‐accumulate (i.e. frequent f/u) 3. Does not re‐accumulate (i.e. frequent f/u) o If all are true, no need to send fluid. o If all are true, no need to send fluid. o F/u in 1‐3 months to ensure no o F/u in 1‐3 months to ensure no reaccumulation or residual mass reaccumulation or residual mass o If no fluid or if bloody further workup o If no fluid or if bloody further workup Fine Needle Aspiration: QUIZ Fine Needle Aspiration Biopsy o Primary Use: Diagnosis of solid masses o Primary Use: Diagnosis of solid masses o FNAB should be done by an experienced o FNAB should be done by an experienced o Least invasive biopsy method o Least invasive biopsy method cytopathologist or breast surgeon? ….TRUE OR cytopathologist or breast surgeon? ….TRUE OR o Sensitivity is operator dependent: o Sensitivity is operator dependent: FALSE? FALSE? o For experienced personnel, 92‐98% o For experienced personnel, 92‐98% o For untrained personnel, 75% Average (as low as 65%). o For untrained personnel, 75% Average (as low as 65%). o A diagnosis of FATTY TISSUE on FNA means o A diagnosis of FATTY TISSUE on FNA means o Experienced cytopathologist necessary to interpret o Experienced cytopathologist necessary to interpret what? what? o Cannot diagnose DCIS, atypical hyperplasia or o Cannot diagnose DCIS, atypical hyperplasia or infiltrating carcinoma. However, >90% there is infiltrating carcinoma. However, >90% there is sufficient material to perform prognostic studies sufficient material to perform prognostic studies o When should you FOLLOW‐UP a woman with a o When should you FOLLOW‐UP a woman with a palpable mass and negative FNA and palpable mass and negative FNA and o A non‐diagnostic result in the setting of a discrete o A non‐diagnostic result in the setting of a discrete mammogram? mammogram? mass requires further work‐up (possible sampling mass requires further work‐up (possible sampling error) error)
Recommend
More recommend