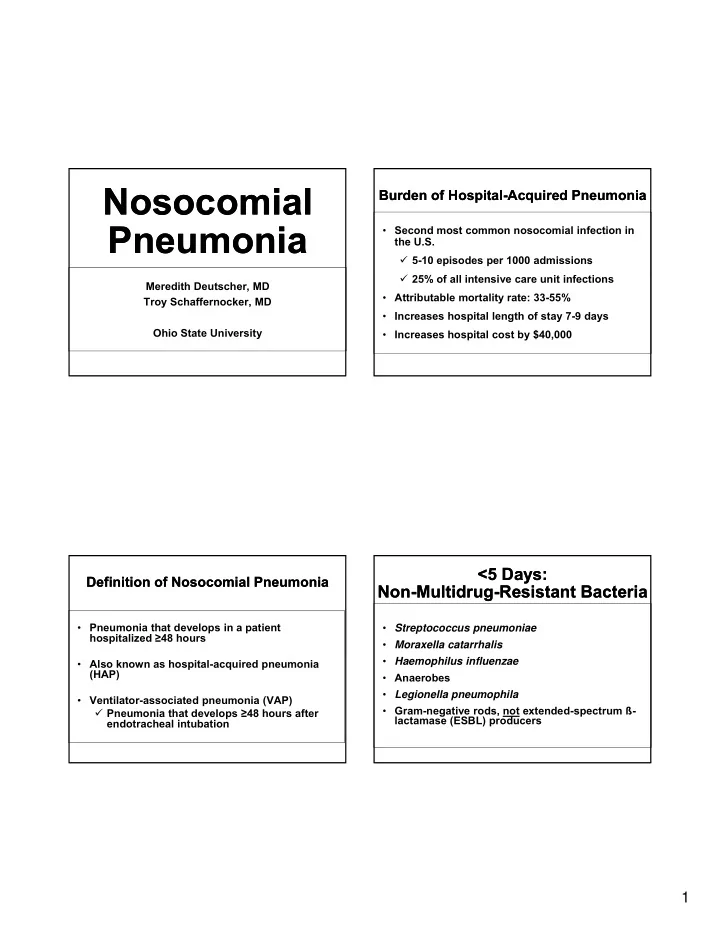
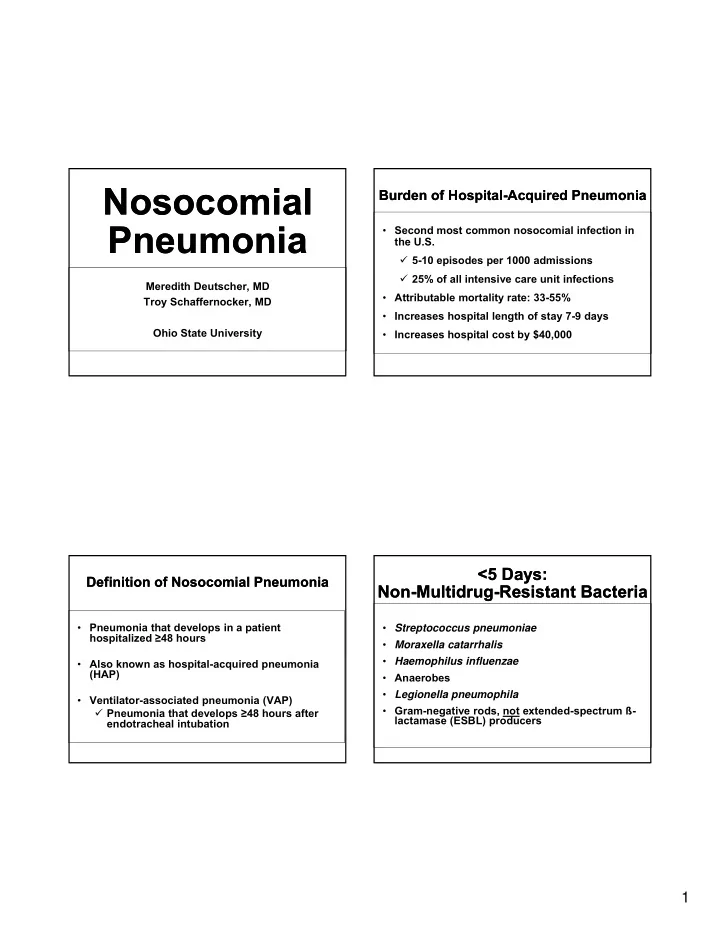
Nosocomial Nosocomial Burden of Hospital-Acquired Pneumonia Burden of Hospital-Acquired Pneumonia Pneumonia Pneumonia • Second most common nosocomial infection in the U.S. � 5-10 episodes per 1000 admissions � 25% of all intensive care unit infections Meredith Deutscher, MD • Attributable mortality rate: 33-55% Troy Schaffernocker, MD • Increases hospital length of stay 7-9 days Ohio State University • Increases hospital cost by $40,000 <5 Days: <5 Days: Definition of Nosocomial Pneumonia Definition of Nosocomial Pneumonia Non-Multidrug-Resistant Bacteria Non-Multidrug-Resistant Bacteria • Pneumonia that develops in a patient • Streptococcus pneumoniae hospitalized ≥ 48 hours • Moraxella catarrhalis • Haemophilus influenzae Haemophilus influenzae • Also known as hospital-acquired pneumonia (HAP) • Anaerobes • Legionella pneumophila • Ventilator-associated pneumonia (VAP) • Gram-negative rods, not extended-spectrum ß- � Pneumonia that develops ≥ 48 hours after lactamase (ESBL) producers endotracheal intubation 1
Diagnosis Diagnosis ≥ 5 Days: ≥ 5 Days: Multidrug-Resistant Bacteria Multidrug-Resistant Bacteria • Methicillin-resistant Staphylococcus aureus • Pseudomonas aeruginosa Pseudomonas aeruginosa • Acinetobacter species • Gram-negative rods, ESBL producers • Gram-negative rods, carbapenemase producers ATS/IDSA HAP HAP Hospital-Acquired Pneumonia with Viral Hospital-Acquired Pneumonia with Viral and Fungal Pathogens Uncommon and Fungal Pathogens Uncommon Viral pathogens Fungal pathogens • Influenza • Candida spp. • New radiographic infiltrate after 48 hours of hospitalization. • Parainfluenza • Aspergillus fumigatus fumigatus • Respiratory syncytial R i t ti l • Clinical findings suggestive of infection virus (including new fever, leukocytosis, purulent • Adenovirus sputum, and decline in oxygenation). • Novel influenza A (H1N1) virus was the dominant circulating influenza virus in 2009 2
HAP HAP Defense Defense • 80% of cells in central airways Ciliated, pseudostratified, columnar epithelium. • Requires entry of microbial pathogens into the lower respiratory tract. Defense Defense Defense Defense • Alveoli � Alveolar • Upper Airway Macrophages � Sneezing Sneezing (phagocytes) (phagocytes) � Swallowing � Lining fluid: � Expectoration surfactant, fibronectin, immunoglobulins which can opsonize or lyse microbial pathogens. 3
Pathophysiology Pathophysiology Transmission Transmission • Inflammatory Exudate • Hematogenous � Extrapulmonary Sites � Pulmonary Consolidation • Endocarditis • Vascular Catheter infections V l C th t i f ti � Systemic Manifestations • Retropharyngeal infections • Fever • Direct Inoculation/Contiguous Spread • Chills � Tracheal intubation • Myalgias � Penetration of the chest wall • Malaise Transmission Transmission HAP HAP • Aspiration � Level of consciousness (alcohol, drugs) • Requires entry of microbial pathogens into the � Neurologic Dysfunction (seizure, stroke) lower respiratory tract. � Mechanical Impairments (endotracheal tube, p ( � Aspiration of oropharyngeal pathogens � Aspiration of oropharyngeal pathogens nasogastric tube) � Leakage of bacteria around an endotracheal tube • Inhalation � Less common: Direct inhalation, Hematogenous � Particles > 10μ m get deposited in nose and spread, Translocation from the GI tract. oropharynx � 5-10 μ m Central airways � <5 μ m can make it all the way to alveoli 4
Physical Exam Physical Exam Diagnosis: Sample Analysis Diagnosis: Sample Analysis • Fever • Sputum • Purulent Sputum � Gram’s staining � Culture • Signs of pulmonary consolidation • Fiberoptic Bronchoscopy p py � D ll � Dullness � Bronchoalveolar lavage (BAL) � Increased fremitis � Protected Sheath Brush � Transbronchial Biopsy � Egophony • Thoracentesis � Bronchial breath sounds � Consider if significant pleural effusion � Rales • Open-Lung Biopsy Diagnosis: Chest Diagnosis: Chest HAP HAP Radiography Radiography • Confirm the presence and • Invasive Diagnostic Strategy vs Clinical location of an infiltrate Diagnosis? • Assess the extent of infection • Detect pleural involvement • Gauge hilar lymphadenopathy • Monitor response to therapy 5
Algorithm Algorithm Endotracheal Aspirate Endotracheal Aspirate • Blind tracheobronchial aspiration � Insertion of a flexible catheter into the distal trachea distal trachea • Bronchoscopically guided � BAL (Bronchoalveolar Lavage) � Protected Specimen Brush ATS/IDSA HAP HAP Selecting Antimicrobial Selecting Antimicrobial Regimens Regimens • Invasive Diagnostic strategy vs Clinical Diagnosis? � Lower respiratory culture should be obtained • Choosing an empiric regimen g g • Bronchoscopically • Choosing a specific regimen • Non-bronchoscopically • Bronchoscopic strategy may improve outcomes – one study showed improved 14 day mortality 6
Selecting an Empiric Selecting an Empiric Selecting an Empiric Regimen, cont’d. Selecting an Empiric Regimen, cont’d. 3. Consult hospital antibiogram Regimen Regimen ICU may have separate antibiogram • Indicates which antimicrobials are more likely • to be effective against a particular pathogen 1. Collect blood and sputum cultures before administering antimicrobials administering antimicrobials 2. Determine whether patient is at risk for infection with MDR pathogen Risk Factors for Infection Risk Factors for Infection Selecting an Empiric Regimen, cont’d. Selecting an Empiric Regimen, cont’d. with MDR Pathogens with MDR Pathogens • Receiving antimicrobial therapy in past 90 days 4. Consider what antimicrobials the patient has • Current hospital stay ≥ 5 days already received • Exposure to hospital’s ICU MDR pathogens What did the patient receive in the past 14 • days? y • Immunocompromised status Immunocompromised status • Risk factors for healthcare-associated Did the patient develop HAP while on • pneumonia: treatment? � Resident of long term-care facility � Hospitalized for ≥ 2 days in past 90 days If possible, the empiric regimen should be � Received hemodialysis in past 30 days comprised of agents from antimicrobial classes to � Receiving wound care which the patient has not been recently exposed. � Family member with MDR pathogen 7
Empiric Regimens: Empiric Regimens: Keys to Empiric Regimen Selection Keys to Empiric Regimen Selection At Risk for MDR Infection At Risk for MDR Infection A. B. C. MRSA coverage antipseudomonal aminoglycoside • Empiric therapy should be broad enough to cover cephalosporin all suspected pathogens. all suspected pathogens • Optimal dosing is needed to control infection. antipseudomonal antipseudomonal carbepenem fluoroquinolone ß-lactamase inhibitor Am J Respir Crit Care Med 2005;171:388-416. Empiric Regimens: Empiric Regimens: Specific Infection � Specific Regimen Specific Infection � Specific Regimen Not at Risk for MDR Infection Not at Risk for MDR Infection • Reassess empiric regimen after 48 hours • Goal: de-escalate or streamline antimicrobial 1. Ceftriaxone coverage • Base on microbiologic data and clinical response • Base on microbiologic data and clinical response 2. Fluoroquinolone • Improves patient outcome by minimizing +/- Azithromycin complications caused by broad-spectrum 3. Ampicillin/sulbactam coverage � C. difficile infection 4. Ertapenem � Selection of MDR pathogens 8
Limit Duration Limit Duration Prevention Measures: Prevention Measures: Aspiration Precautions Aspiration Precautions 7 days 14 days • Uncomplicated HAP • P. aeruginosa or VAP, and • Monitor sedation • Acinetobacter species • Responding to • Responding to • Not responding to N t di t • Elevate head of bed therapy therapy • Consider speech and swallow consult Prolonged therapy leads to colonization with resistant organisms. Prevention Measures: Prevention Measures: Assess Nonresponders Assess Nonresponders Vaccination Vaccination • Wrong diagnosis (not pneumonia) • Assess vaccination status prior to discharge • Wrong antimicrobial � Pneumococcal vaccine � Wrong organism or drug-resistant organism � Influenza vaccine � Influenza vaccine � Suboptimal dosing � S b ti l d i • These vaccines may be given together • Complication • S. pneumoniae is a leading cause of vaccine- � C. difficile preventable illness and death in the U.S. � Empyema or abscess � Approximately 70 million people with existing � Drug fever indications for vaccination are not vaccinated NHIS, 2007 9
Prevention Measures: Prevention Measures: VAP – ET tube VAP – ET tube Infection Control Infection Control • Endotracheal tube � Cuff pressure 20 cm H2O • Hand hygiene to reduce spread of multidrug- � Aspiration of subglottic secretions may resistant pathogens help prevent early VAP p p y • Transmission-based precautions • Transmission based precautions � Contact � Droplet � Airborne Prevention of VAP Prevention of VAP VAP – GI considerations VAP – GI considerations • Oral antiseptics – positive results in • Intubation and Mechanical Ventilation cardiothoracic surgery patients increase the risk of pneumonia 6 to 21 fold • Selective Decontamination of the Digestive tract – in prospective studies. p p Mixed results Mixed results • Antacids, H2 blockers, Proton Pump inhibitors – Mixed results, increased enteric gram negative colonization • Probiotics - jury still out 10
Recommend
More recommend