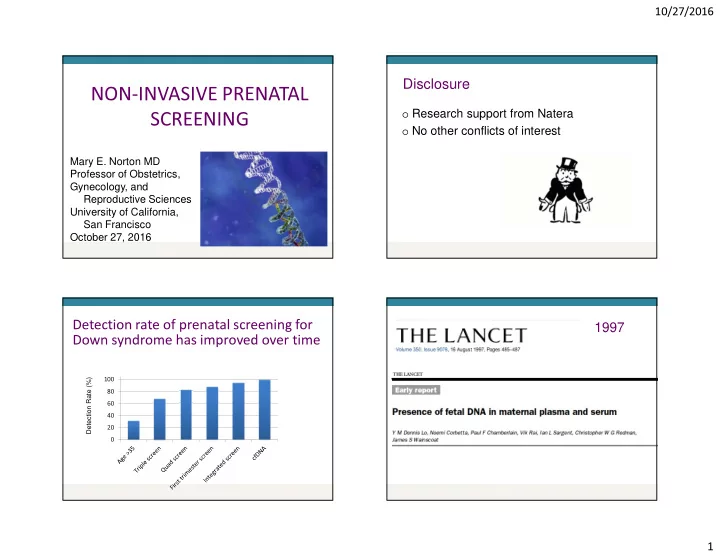
10/27/2016 Disclosure NON-INVASIVE PRENATAL o Research support from Natera SCREENING o No other conflicts of interest Mary E. Norton MD Professor of Obstetrics, Gynecology, and Reproductive Sciences University of California, San Francisco October 27, 2016 1997 Detection rate of prenatal screening for Down syndrome has improved over time 120 Detection Rate (%) 100 80 60 40 20 0 1
10/27/2016 o Short segments of DNA in Cell free DNA Analysis of cell free DNA maternal plasma o Primarily placental origin Massively Parallel Shotgun Sequencing (MPSS): Palomaki et al, 2011 o Random sampling of cfDNA fragments from all chromosomes o A z-score value is used as a cut-off for trisomy (z-score of 3) N=1696 Palomaki GE et al. (2011), Genet. Med 2
10/27/2016 cfDNA screening for T21: meta-analysis ( Gil et al, Ultrasound Obstet Gynecol, 2015 Professional Society Opinions (2012): ACOG; ACMG; International Society of Prenatal Diagnosis; National Society of Genetic Counselors Common themes: There are recognized benefits, but… o Not diagnostic • Needs confirmation • “Advanced screening test” DR: 99.2% (98.5 - 99.6) FPR: 0.09% (0.05 - 0.14) o Only detects T18 and T21 (vs invasive testing) o Requires comprehensive genetic counseling o Should only be used in validated groups (eg high risk) � Need a low risk study before introducing into general population screening Why Did We Need a Low Risk Study? “There are known knowns; there are things we know we know. We also know there are known unknowns; that is to say we know there are some things we do not know. But there are also unknown unknowns -- the ones o 15,841 women had cfDNA and first trimester we don't know we don't know.” screening - Donald Rumsfeld o Mean maternal age = 30.7 yrs 3
10/27/2016 Cell free DNA: Biologic Challenges “NEXT” study: 15,841 average risk women False positives: o Unrecognized or “vanishing” twin o Placental mosaicism Cell free First o Low level maternal mosaicism, esp sex chromosomal o Maternal genetic variation (copy number variants) DNA trimester o Maternal malignancy screening screening False negatives: o Low level of fetal DNA Detection rate 38/38 30/38 (79%) P=0.008 o Placental mosaicism (100%) o Maternal genetic variation (copy number variants) False positive 0.06% 5.4% P<0.0001 Failed results: o Increased BMI rate o Low level of fetal DNA Positive 81% 3.4% P<0.0001 o Fetal aneuploidy predictive value Norton et al, NEJM, 2015 Fraction of cell free DNA that is fetal in origin: Fetal fraction and maternal weight “Fetal Fraction” Hudecova I et al, PLoS One, 2014 4
10/27/2016 The less fetal DNA, the harder to tell Obesity in US Adults (BMI) normal from abnormal Fetal Fraction Fetal Fraction 5
10/27/2016 “NEXT” study: 15,841 average risk women Fetal Fraction o 488 (3%) women had no result • Low fetal fraction, failed sequencing, high variance in sequencing • Risk of aneuploidy was 1/38 (2.7%) • Much higher than 1/236 (0.4%) in cohort o Total of 68 significant aneuploidies in the cohort • 57/68 (84%) were detected Norton et al, NEJM, 2015 Kaiser Experience: No Results Cases Kaiser Experience: No Results Cases Total Pregnancies Sampled N = 4446 KPNC 10/29/12 – 6/30/14 Total pregnancies sampled = 4446 Low Risk High Risk No Results NO FINAL RESULT N = 4187 N = 157 N = 102 N = 65 (1.5%) (94.2%) (3.5%) (2.3%) Redrawn Redraw Declined N = 63 N=39 Chromosomes not done Normal chromosomes Abnormal chromosomes Low Risk High Risk No Result 43/65 (66%) 13/65 (20%) 9/65 (14%) N=32 (50.8%) N=5 (7.9%) N=26(41.3%) NO FINAL RESULT N = 65 (1.5%) 6
10/27/2016 No result by cfDNA: low FF, karyotype T18 Fetal Fraction Fetal Fraction Meschino et al, Prenatal Diagn, 2016 7
10/27/2016 cfDNA screening Traditional screening � Trisomy 13, 18, 21 � Trisomy 18, 21, +/-13 � Sex chromosomes � Other chromosomal � +/- microdeletions � Early dx fetal anomalies, including cardiac (NT) � Maternal cancer � Spina bifida and ventral � Maternal genetic wall defects (MSAFP) diseases � Adverse obstetric � Maternal sex outcomes chromosomal � Preeclampsia, PTB, FGR aneuploidy High Risk, Low Risk, and Positive Predictive Value 8
10/27/2016 Wang et al, Genetics in Medicine, 2015 Aneuploidy No. of positives No (%) confirmed T21 41 38/41 (93%) T18 25 16/25 (64%) Risk Group Positive predictive value Entire cohort 81% T13 16 7/16 (44%) (mean age 30.7 yrs 45,X 16 6/16 (38%) Maternal age <35 yo 76% Low risk serum FTS (<1/270) 50% 9
10/27/2016 The poorly understood PPV Consequences of false positive results cfDNA N=100,000 1% false positives 1000 abnormal results 6.2% TAB w/o confirmation 62 TAB o 6.2% had termination without karyotype 50% PPV 31 TP 31 FP confirmation o Disconcerting if PPV is <50% 31 TAB of normal fetuses 10
10/27/2016 PPV Calculator: www.perinatalquality.org Consequences of false positive results cfDNA Serum Screening N=100,000 N=100,000 1% false positives 5% false positives 1000 abnormal results 5000 abnormal results 6.2% TAB w/o confirmation 0.1% loss 62 TAB rate (amnio) 50% PPV 31 TP 31 FP 5 losses of normal fetuses 31 TAB of normal fetuses 11
10/27/2016 Trisomies 13,18 and 21 comprise 75% of aneuploidies Other 16.9% Tri 21: 53.2% SCA: 8.2% Tri 13: 4.6% Tri 18: 17.0% Chromosomal Microarray (CMA) for Microdeletions are genomic imbalances Prenatal Diagnosis detected by microarray but not karyotype Miller et al, 2010, AJHG 12
10/27/2016 Diagnostic Yield of Chromosomal Microarray in New “menu” in prenatal testing Cases with Normal Karyotype Indication for Testing Clinically Relevant (N=96) U/S Anomaly Screening test for common aneuploidies (1/500) 6.0% N=755 AMA 1.7% VS N=1,966 Positive Screen 1.7% Invasive diagnostic testing with CMA (1/60) N=729 Other 1.3% N=372 Disorder Prevalence Common trisomies 0.2% cfDNA and chromosomal microarray (13,18,21) Causes of Birth Other chromosome 0.4% Defects and IF: abnormalities Other Adverse Microdeletions and 1.5% CMA detects an abnormality in 1.7% of cases (about 1/60) duplications Perinatal Mendelian Genetic 0.4% AND: Outcomes: Disorders It’s Not All Down cfDNA detects T13,18, 21 – about 1/500 pregnancies Congenital heart defects 0.3% Syndrome THEN: Other structural defects 3% � If cfDNA is the routine screening test, it will detect only about 12% of diagnosable chromosomal abnormalities Adverse OB outcomes 15-20% Total ~25% 13
10/27/2016 Expanded panels “How did this happen? I had the non-invasive amnio…” o Trisomies 9, 16 and 22 • Rarely seen in viable pregnancies except as mosaics • Common causes of confined placental mosaicism - Much more common in CVS samples than amniocentesis • Even complete trisomy in the placenta often associated with a normal fetus o Microdeletions (22q, 1q36, 5p-, 4p-, 15q11-13 ) • Also 8q-, 11q- o MaterniTGenome Should all women be offered screening for Should all women be offered screening microdeletions? for microdeletions? 14
10/27/2016 Microdeletion syndromes are rare Should all women be offered screening Syndrome Frequency Features for microdeletions? 22q11.2 1/4,000 Varies: cardiac, palatal, immune, (DiGeorge) intellectual disability 1q36 1/10,000 Severe intellectual disability (ID), +/- obvious structural anomalies Angelman 1/20,000 Severe ID, seizures, speech delay Prader-Willi 1/30,000 Obesity, ID, behavioral problems Cri-du-chat 1/50,000 Microcephaly, ID, +/- CHD Wolf-Hirshhorn 1/50,000 ID, seizures, +/- CL/CP Total 1/2500 o Microdeletions can be detected by cfDNA, but • Difficult to validate • Much of the data on artificial samples • Clinical testing so far very limited 15
10/27/2016 ACOG/SMFM September 2015 o Conventional screening is most appropriate first line screen for most patients o Ethically any patient may choose cfDNA screening, but should be counseled regarding limitations and benefits o Diagnostic testing is required to confirm abnormal results before irreversible decisions o Testing for microdeletions and in twins should not be performed July 2016 American College of Medical Genetics, 2016 American College of Medical Genetics, 2016 Recommends that ALL pregnant women should be: Other issues addressed: o Diagnostic testing should be offered for a “no o Offered the option of either screening or call” result, rather than repeat testing o Other options should be suggested for women diagnostic testing o Offered cfDNA for sex chromosomal aneuploidies with significant obesity o Referral to genetics professional with positive o Informed of availability of cfDNA for cfDNA, no call results other than FF microdeletions 16
10/27/2016 Oh no, more genetics?? gem.perinatalquality.org 17
10/27/2016 Thank You! 18
Recommend
More recommend