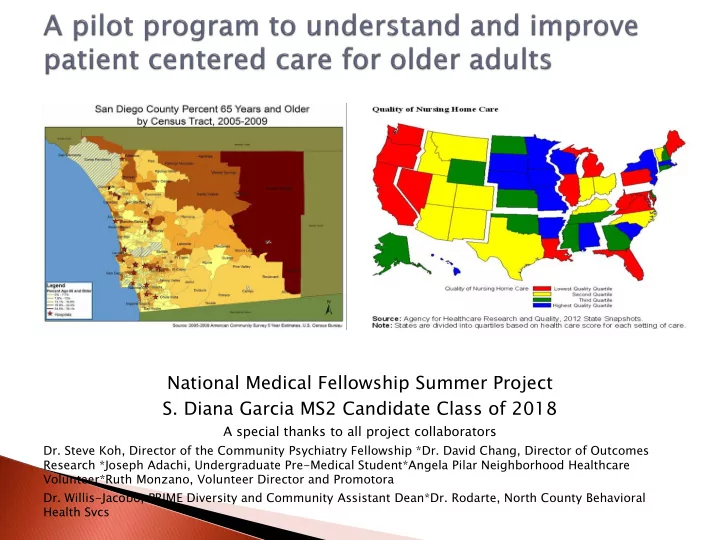
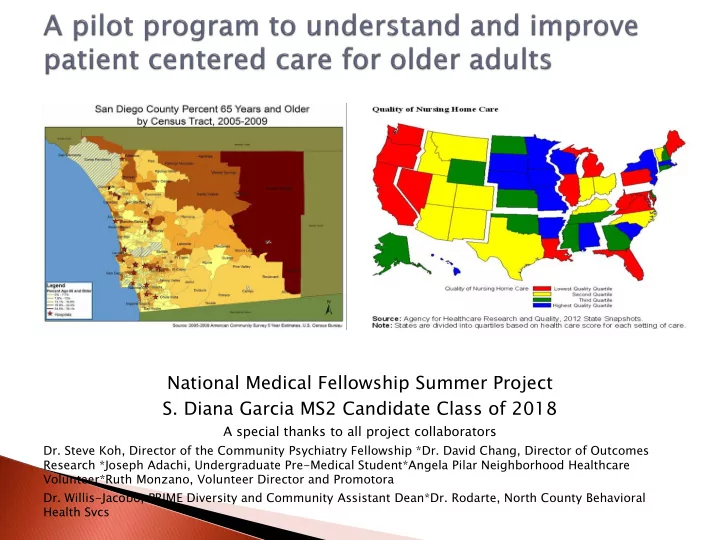
National Medical Fellowship Summer Project S. Diana Garcia MS2 Candidate Class of 2018 A special thanks to all project collaborators Dr. Steve Koh, Director of the Community Psychiatry Fellowship *Dr. David Chang, Director of Outcomes Research *Joseph Adachi, Undergraduate Pre-Medical Student*Angela Pilar Neighborhood Healthcare Volunteer*Ruth Monzano, Volunteer Director and Promotora Dr. Willis-Jacobo, PRIME Diversity and Community Assistant Dean*Dr. Rodarte, North County Behavioral Health Svcs
Ambulatory visits due to adverse effects of medical care Receipt of potentially inappropriate prescription medication Hospital readmission There here is 20% 0% inappr appropr opriat iate e use e of prescription criptions . One ne of the e reasons sons is ions . . that at patien ients s are not t askin ing g the e right ht quest estion Agency ncy for Healthca thcare re Resear arch ch and Quality lity Recom commend mends A S Solution on “Ten questions to ask your provider” Ultimate tely: y: Patient nt + Provider der = O Outco comes mes References: Questions To Ask Your Doctor: Questions Are the Answer. September 2012. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/patients-consumers/patient-involvement/ask-your-doctor/index.html Center for Quality Improvement and Patient Safety (CQuIPS). October 2012. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/cpi/centers/cquips/index.html Calif ifor ornia ia Quality lity Measures Compare red d to Achievable ievable Benchmark arks Agency for Healthcare Research and Quality http://nhqrnet.ahrq.gov/inhqrdr/state/select At the Intersection of Health, Health Care and Policy: Improvin oving g Chron onic ic Illness Care: : Translatin lating g Evide dence e Into Action ion A Bonomi et al http://selfmanagementalliance.org/wp-content/uploads/2013/08/Wagner-CCM.pdf
Improving Worsening
Improved patient Primary Outcome Future Projection awareness of questions to Improved patient Increased ask their providers about satisfaction with communication ie: their medication medical care and asking providers their provider questions will increase adherence to care recommendations Investigate how comfortable patients’ are asking about adverse side effects, related diagnosis, and alternatives. Describe a largely monolingual population’s demographic information, ◦ medical history (primary and behavioral), and satisfaction with their medical care. Satisfaction with care will serve as a surrogate to patient empowerment and ◦ positive patient-provider relationship. Develop a health curriculum tailored to the needs of the older adult population will be developed Train high school students in the Kaiser Permanente Summer Urban Fellowship and Neighborhood Health Volunteers on issues with prescription adverse effects in older adults through case studies and role-play workshops.
Older Adults Rx coordination/reconciliation Improved patient-provider communication Intersection of mood, satisfaction, trust, autonomy, self-perceived health outcomes/improvements Youth Increased likelihood to pursue a career in health care Improved knowledge of issues related to older adults Improved knowledge in patient provider communication and prescription reconciliation
Older Adult Focus: Youth Mentoring Focus: Kaiser Permanente Neighborhood Health’s Summer Urban Fellowship “ Edad De Oro” Older Adult N=40 and Neighborhood Primary Care Mental Health Health Volunteer Program Integration Program Community College ◦ Carried out a needs Student volunteers. N=2 assessment for the – Carried out a program “Prescription Administer Pre-Post survey: Reconciliation 40 Questions: Workshop” demographic information, • Included Pharmacology Crash “10 questions to ask your Course provider” • Training on 10 questions patient satisfaction questions patients to ask their doctor
N= 24 21 females 3 males Majority of those surveyed were not bilingual, ◦ 95.8% (23/24) reported ability to read and write in Spanish. Access ◦ 10 reported seeing their primary care physician in the past month. ◦ All except one had seen a doctor in the last six months. ◦ 82.6% reported receiving regular physicals ◦ 75 % (18/24) reported “always” receiving regular check-ups. Some reported going to Mexico for their care but this specific question was not on the survey to be analyzed. ◦ Six (24%) Neighborhood Healthcare patients Health Literacy ◦ 66% (16/24) always understand what the doctor explains to them during an office visit. ◦ 41.6% (10/24) always feel they can prepare for a surgery, ◦ 29.1% (7/24) reported “No.” they do not know how to prepare for a surgery ◦ 66% (16/24) reported always understanding what the doctor is telling them.
Satisfaction 87.5% reported never having an issue with making an appointment. 70.8 % (17/24) reported “always” liking the care they receive and “always” feeling that their medical problems are taken care of when they leave the clinic. 62.5 % (15/24) said they “always” feel comfortable asking their medical doctor or pharmacist questions about their care. 79.2 % (19/24) participants said they are “always” familiar with the medicine they are prescribed. Social 75% (18/24) of participants do not live alone. 41.6% (10/24) always get together with family and friends. 100% of participants reported always preparing their own meals and majority only “once in a while” going to eat processed foods. Depression 4.16% (1/24), always, 8.3% (2/24) often, 33.3% (8/24) occasionally 37.5% (9/24) rarely 16.6% (4/24) never feel depressed. When asked if they sought treatment 56.5% (13/23) reported not seeking treatment (6/23) did seek treatment. Four did not respond.
To eliminate mental health disparities that impact older adults community partnerships such as UCSD Health Sciences, Neighborhood Healthcare Promotoras, Medical Pathways Program at San Ysidro High School, and Kaiser Permanente are key to the overall wellness and engagement of under-cared for individuals and community at large. Facilitators (promotoras) who are trusted by the community and genuinely understand issues of barriers to care and medication errors are the success factor. Senior peer programs should be opened to the entire community with referring doctors being at non-affiliated sites to the host site. Participants attending the program have been attending from a range of a few weeks to more than 10 years. 16.6% (4/24) have been attending for five or more years. Thus, deciding to start a program should planned for long term attendance. Over the phone, patients who reported being depressed were more difficult to talk to but they elucidate the importance of diversity training. Interact with patients who seemingly made the interview more challenged actually help providers in training understand how to deal with different people and communication styles. Curriculum at the medical undergraduate level is needed to fulfill this training.
Limitat itation ions: s: Satisfaction questions may not have been answer as honestly as we may have preferred. Surveyor has already built relationships with the participants and they may not want to say anything negative with the conception that doing so would hurt the surveyor’s feelings. Furthermore, undoubtedly the results of 24, one- hour interviews from participants at a single site are not sufficient for one to draw conclusive arguments. In the area of mentoring survey questions must be carried out with the youth at the time of the workshop. From that survey, we could consolidate the results and create a tool that can collect further information. Recom omme mend ndatio ations ns- As a program that aims to improve the wellness of marginalized communities using a primary care behavioral health integrative approach, the Edad De Oro – Senior Peer Group is doing an effective job of meetings its key goals. The mental health care needs of communities of color are too vast to expect primary care physicians including psychiatrist to be able to cover the needs with one-on-one consults. Promotoras are trained extensively and effectively outreach to the neediest participants. There is trust, gratitude, motivation, and an overall state of wellness at the center on Friday mornings. Expansion of the program to other sites and to other days of the week could help multiply the positive effects of the program on the nearby communities. Primary care physicians, geriatricians, and psychiatrists must be made aware of these types of programs and must encourage their patients to attend. Get other community clinics on-board. Utilize the mentoring focus in the future as a experiential experience to help them consider a career in geriatrics.
Recommend
More recommend