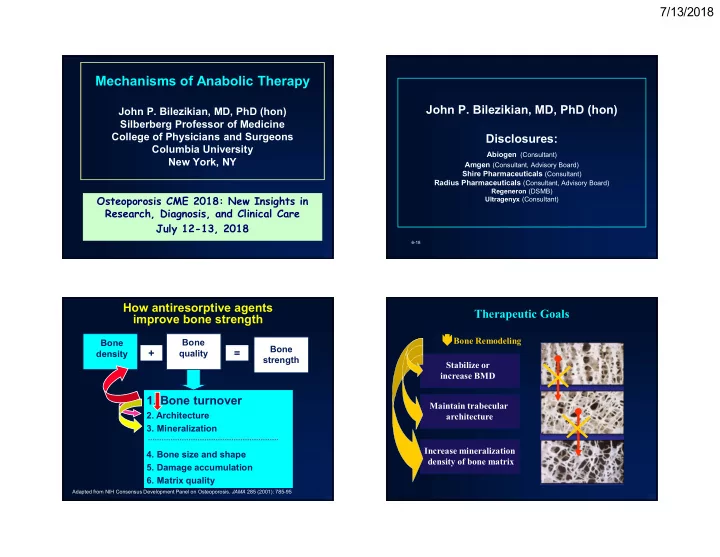
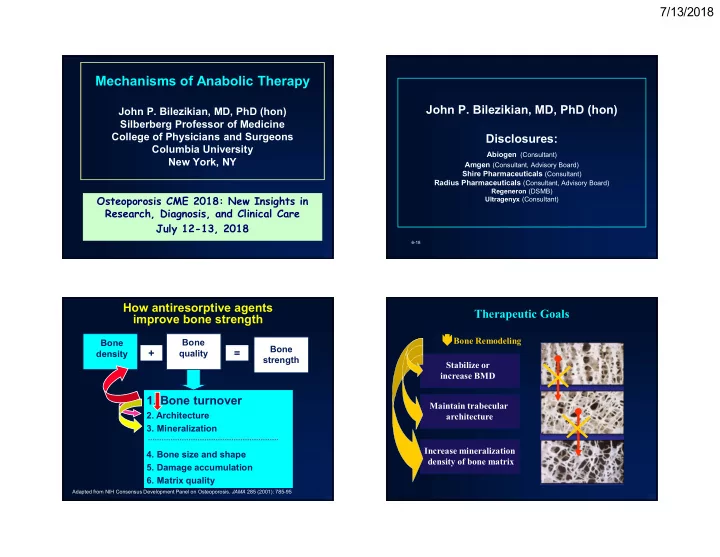
7/13/2018 Mechanisms of Anabolic Therapy John P. Bilezikian, MD, PhD (hon) John P. Bilezikian, MD, PhD (hon) Silberberg Professor of Medicine College of Physicians and Surgeons Disclosures: Columbia University Abiogen (Consultant) New York, NY Amgen (Consultant, Advisory Board) Shire Pharmaceuticals (Consultant) Radius Pharmaceuticals (Consultant, Advisory Board) Regeneron (DSMB) Osteoporosis CME 2018: New Insights in Ultragenyx (Consultant) Research, Diagnosis, and Clinical Care July 12-13, 2018 6-18 How antiresorptive agents Therapeutic Goals improve bone strength Bone Remodeling Bone Bone Bone + = density quality strength Stabilize or increase BMD 1. Bone turnover Maintain trabecular 2. Architecture architecture 3. Mineralization Increase mineralization 4. Bone size and shape density of bone matrix 5. Damage accumulation 6. Matrix quality Adapted from NIH Consensus Development Panel on Osteoporosis. JAMA 285 (2001): 785-95 1
7/13/2018 The chronology of the development of therapies for osteoporosis: irony #1 For the first 20 years or so, the field was dominated by drugs that prevent THE HOLY GRAIL? microstructural deterioration, add mineral content to bone, but do not help to reconstruct the skeleton The chronology of the development of therapies for osteoporosis: irony #2 Parathyroid Hormone? The attempt to improve skeletal “Parathyroid hormone is microstructure as a treatment for bad for bones” osteoporosis began with the development of a drug that was thought to do the opposite! 2
7/13/2018 PHPT IN THE EARLY YEARS, 1929-1970 The densitometric signature of primary The captain (1929-1933) and The lady (1970) hyperparathyroidism in the modern era 100 * *Differs from radius, p<.05 Bone Mineral Density: * % of Expected 90 80 70 Lumbar Spine Femoral Neck Radius Silverberg, Bilezikian et al. JBMR, 1989 Fracture Risk in Primary Hyperparathyroidism Pledging allegiance to the proposition Vertebral Distal Forearm that BMD predicts fracture risk….the expectation in PHPT was: All Rib Vertebral sites Non-vertebral sites Khosla et al, J Bone Min Res 14:1700-1707, 1999 3
7/13/2018 Vignali E, Viccica G, Diacinti D et al. Morphometric Vertebral Fractures HRpQCT (Xtreme CT) In Postmenopausal Women with Primary Hyperparathyroidism J Clin Endocrinol Metab 2009;94:2306-2309 • 3-D stack of 110 high 40 40 P <0.0001 resolution slices P =0.15 35 35 Non-dominant distal radius and tibia P <0.0001 • ~ 3 min scan time 30 30 P =0.03 Fractured cases (%) • <4 µSv radiation 25 25 P <0.0001 • Reproducibility: 20 20 • Density: 0.7-1.8% 15 15 P=NS • Structure: 1.2-5.2% 10 10 5 5 0 0 Surg. Surg. Controls Symptomatic Asymptomatic Controls Criteria Criteria (n=300) (n=41) (n=109) (n=300) Met Not Met Patients Radius Tibia (n=64) (n=45) Asymptomatic Boutroy et al. JCEM 2005. 90(12):6508-15 Trabecular microstructural abnormalities in PHPT by HRpQCT Parameters HRpQCT (Hansen S et al. J Bone Miner Res 2012;27:1150-1158) Matched Control Baseline data: PHPT vs Controls (p<0.05) * * # Index RADIUS TIBIA * * TV BMD Trabecular and cortical indices are ** Cort BMD reduced at radius and tibia in * # * Trab BMD Asymptomatic PHPT * PHPT # Trab BV/TV * Tb.N Tb. Th * Tb. Sp * * Strength Failure Load Stein E, Silva BC et al. HRpQCT in PHPT, J Bone Miner Res, 2013 4
7/13/2018 Individual Trabecular Segmentation Deteriorated Trabecular Microstructure by Trabecular Bone Score in Postmenopausal PHPT Analysis in PHPT (Silva et al, J Clin Endo Metab, 2013) Stein E, Silva BC J Bone Miner Res, 2013 Characteristics PHPT (n=22) Microarchitecture partially TBS 1.24 ± 0.02 degraded L1-L4 T-Score -1.0 ± 0.4 Total hip T-Score -1.1 ± 0.3 <1.2= degraded Femoral neck T-Score -1.4 ± 0.3 1.2 – 1.35= partially degraded >1.35= normal 1/3 radius T-Score -1.3 ± 0.4 Osteoporosis at any site 11 (50%) L1-L4 T-score n (%) L1-L4 TBS classification n (%) classification Degraded 8 (36) Matched Control Primary Hyperparathyroidism Osteoporosis 3 (14) Partially degraded 8 (36) Osteopenia 7 (32) Green: horizontal plates (more competent) Normal 6 (27) Normal 12 (53) Red: vertical plates (less competent) The chronology of the development of The inescapable conclusion therapies for osteoporosis: irony #3 E ven when presenting as an During the time that the symptomatic asymptomatic disorder Primary phenotype of PHPT was being well hyperparathyroidism is characterized (1930-1960), another set of observations was leading to another conclusion: BAD FOR BONES! Parathyroid Hormone is not always bad for bone 5
7/13/2018 Parsons, Reeve, Potts, Slovik, Neer, Parathyroid Hormone is not always Hodsman, Dobnig et al. bad for bones (circa 1969-1997) Rats will gain enormous amounts of bone (Bauer, Aub, Albright, 1929; Pugsley and Selye, 1932 ) All demonstrated an anabolic effect of PTH under certain circumstances DXA, even though it proved to be misleading in A common cautionary note: PTH alone might serve an anabolic function on trabecular bone but a catabolic PHPT, did give the idea that under certain function at cortical bone (“borrowing from Peter to pay circumstances, PTH might be advantageous to Paul”) bone under certain circumstances (Silverberg, Bilezikian, Use of either an active Vitamin D analogue or an et al. 1986- ) antiresorptive was thought to be important in demonstrating a true anabolic effect of PTH, namely an The visionaries who were listening to a different increase in total bone mass (subsequently shown not to be the case- Neer et al. N Eng J Med 2001) drummer (Parsons , Neer & Potts, 1971) PTH Mode of Administration, Timing and Dose PTH dose and timing determine Determine whether PTH is anabolic or catabolic in the rat skeleton its effect on bone MODE EFFECT 40 (% Trabecular Bone Perimeter) Vehicle *p<.01 vs vehicle * **p<.001 vs vehicle 1 hour/day 30 Cell Abundance Continuous Continuous Catabolic ** (high dose) 20 Daily 10 Anabolic (low dose) 0 Osteoblast Osteoclast Dobnig H, Turner RT. Endocrinology. 1997;138(11):4607-4612. Dobnig H, et al. Endocrinology 1997;138:4607-12. 6
7/13/2018 Anabolic Activity of PTH: Osteocyte – the mechanosensor Osteocyte – the mechanosensor Putative Mechanisms • Regulatory • Cellular – RANK ligand- – Recruitment of osteoprotegerin system new osteoblasts – Sequences in the – Activation of PTH molecule lining cells – Intracellular signaling – Increased osteoblast life pathways span and activity – Activation of specific genes – Increased function of – Post receptor mechanisms periosteal cells or their (IGF I, Wnt signaling, progenitors sclerostin) – Shift from adipocyte to – Increased secretion of local osteoblast differentiation factors (IGF-I) – Increased osteocyte function Marotti G, 1996 Marotti G, 1996 Three keys to the PTH anabolic potential of PTH Runx2-expressing Intermittent • Low dose osteoblast progenitor • Intermittent administration SOST BMP BMP Wnt Wnt cAMP/PKA • Pulsatility with rapid “on” and “off” kinetics P Smad4 s d -catenin -catenin P P a m CtBP CtBP CREB CREB S Tcf Tcf Under these conditions….. TFs - R RANKL OPG Anabolism Catabolism 7
7/13/2018 PTH is anabolic: Quadruple Labels in Bone Formation Markers increase before Teriparatide-treated and Bone Resorption Markers Control Subjects 80 70 Mean % Change in 60 Turnover Marker 50 40 30 20 Osteocalcin 10 n-telopeptide 0 0 1 2 3 4 5 6 Time (Months) Teriparatide Control Lindsay R, et al. Lancet. 1997;350(9077):550-555. Dempster et al. 2003 PTH as an Anabolic Agent for Bone: Initial Cellular Mechanisms of PTH A Kinetic Model Bone formation markers Peak Index of Bone Turnover Early increase in bone formation also seen in dynamic histomorphometic indices by transiliac bone biopsy PTH stimulates bone formation directly first and PTH stimulates bone formation directly first and then stimulates the remodeling process then stimulates the remodeling process Months 8
7/13/2018 Dynamic mechanisms utilized by PTH as an Anabolic Agent for Bone: A Kinetic Model osteoanabolic drugs Bone formation markers Modeling-based bone formation Peak Index of Bone Turnover Remodeling based bone formation Bone resorption markers Overflow remodeling-modeling-based “ Anabolic bone formation Window ” Believed to limit the osteoanabolic potential of PTH Months Osteoanabolic Mechanisms Three Types of Bone Formation RBF: bone Remodeling-based Formation (RBF) formation over RBF = Remodeling- Scalloped cement Line remodeled based formation surfaces MBF: bone formation over MBF = Modeling- Modeling-based Formation (MBF) quiescent based formation Smooth cement line surfaces Overflow modeling-based oMBF : bone Formation (oMBF) formation oMBF = Overflow Double-labels extend beyond the beyond the Modeling-based boundaries of the scalloped cement boundaries of formation the BRU line Dempster DW et al Longitudinal Effects of Teriparatide or Zoledronic Acid on Bone Modeling- and Remodeling-Based Dempster DW et al Longitudinal Effects of Teriparatide or Zoledronic Acid on Bone Modeling- and Remodeling-Based Formation in the SHOTZ Study. J Bone Miner Res. 2017 Nov 30. 10.1002/jbmr.3350. [Epub ahead of print] Formation in the SHOTZ Study. J Bone Miner Res. 2017 Nov 30. 10.1002/jbmr.3350. [Epub ahead of print] 9
Recommend
More recommend