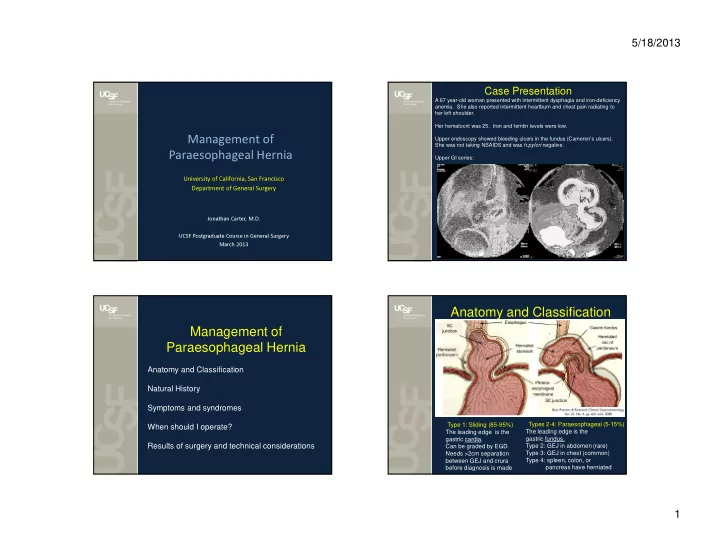
5/18/2013 Case Presentation A 67 year-old woman presented with intermittent dysphagia and iron-deficiency anemia. She also reported intermittent heartburn and chest pain radiating to her left shoulder. Her hematocrit was 25. Iron and ferritin levels were low. Upper endoscopy showed bleeding ulcers in the fundus (Cameron’s ulcers). Management of She was not taking NSAIDS and was h.pylori negative. Paraesophageal Hernia Upper GI series: University of California, San Francisco Department of General Surgery Jonathan Carter, M.D. UCSF Postgraduate Course in General Surgery March 2013 Anatomy and Classification Management of Paraesophageal Hernia Anatomy and Classification Natural History Symptoms and syndromes Type 1: Sliding (85-95%) Types 2-4: Paraesophageal (5-15%) When should I operate? The leading edge is the The leading edge is the gastric fundus. gastric cardia. Results of surgery and technical considerations Type 2: GEJ in abdomen (rare) Can be graded by EGD. Type 3: GEJ in chest (common) Needs >2cm separation Type 4: spleen, colon, or between GEJ and crura before diagnosis is made pancreas have herniated 1
5/18/2013 Natural History Natural History Attempt to model elective PEH repair versus watchful waiting in Markov decision analysis. The best available statistics were used in the model: Skinner and Belsey (1967) reported on cohort of 21 patients Mortality of elective PEH repair: 1.4% managed with watchful waiting and reported 6 deaths (29%) Mortality of emergency PEH repair: 5.4% (based upon NIS data) related to strangulation, perforation, or hemorrhage. Probability of symptoms with watchful waiting: 1.1% /year Hill (1973) reported a 30% rate of incarceration in a cohort of patients managed with watchful waiting The reported mortality of emergency operations was 17%. …and as a result, for years textbooks recommended prophylactic repair for all comers. Many questioned these recommendations because the predicted disasters weren’t evident in everyday practice. There was not (and still isn’t) good data on the natural history of PEH Ann Surg 2002;236:492. Natural History When to operate? • For patients >65 years, watchful waiting was superior to elective PEH repair with an improvement of 0.13 QALYs. Reflux symptoms • Sensitivity analysis showed that this result persisted across a Heartburn, regurgitation, chest pain, cough, hoarseness, aspiration wide range of expected surgical mortalities: with or without pneumonia Obstructive symptoms Dysphagia, chest pain, early satiety, bleeding or iron deficiency anemia from gastric stasis ulcers (Cameron lesions) Respiratory symptoms Recurrent aspiration. Shortness of breath and dyspnea on exertion are generally caused from anemia, not mass effect / displacement of lung Entrapment symptoms Acute pain, perforation, sepsis • The data supporting this model have been questioned. Peters Borchardt's triad =acute epigastric pain, inability to vomit, inability reported a 21% in-house mortality for emergency PEH repairs to pass NG tube = impending gangrene = immediate exploration and 1% mortality for elective repairs in the modern era needed. (JGISurg 2010). And the 1.1%/year rate of symptoms based upon very weak data. These data favor elective repair over watchful waiting. Indications for surgery In general, repair the PEH when these symptoms are present. • Confounder: The are no truly asymptomatic patients. Careful pearl: if you have a young patient, find some symptoms interview will reveal foregut symptoms in over 90%. 2
5/18/2013 Completed dissection Key Elements of the Operation • Reduce the stomach. Dissect • Close the crura posteriorly. the herniated stomach away No benefit to pledgets. from the hiatus and get a Mesh to be discussed. penrose around all the • Do a 360 ° fundoplication. herniated contents. Don’t • Divide the short gastrics injure the left gastric artery or • Do a posterior gastropexy vagus nerves. Detach the sac • Do collar anchoring from the stomach stitches circumferentially. • No anterior gastropexy or • Mobilize the lower esophagus gastrostomy tube in high into the mediastinum primary repairs. circumferentially. This lengthens it. Stop when GEJ Sack Attack is in abdomen without having to pull on it. • Remove the sac and fat pad off the stomach, GEJ, hiatus. Fat will be hypertrophied. Sutured cruroplasty Completed repair 3
5/18/2013 Results: recurrence Results: Symptom control • Radiographical recurrence will occur in 20-60% of patients who are followed for at least 5 years. • The vast majority of patients with radiographical recurrence will be minimally symptomatic. The few with symptoms can generally be managed with PPIs. preop Day 1 Day 120 Results: Symptom control Results: Symptom control 4
5/18/2013 Results: Symptom control Results: Symptom control Strategy 1: reinforce hiatus with synthetic mesh • Granderath et al (2005) – Prospective randomized trial of 100 patients undergoing So what can be laparoscopic floppy Nissen fundoplication for GERD and hiatal hernia repair. 1 year follow-up. – 45 with simple sutured crural closure (Group 1), done to reduce – 45 with onlay of polypropylene mesh (Group 2). – Intrathoracic wrap migration in 13 patients (26%) with suture closure vs only 4 (8%) with onlay polypropylene mesh. the risk of recurrence? 5
5/18/2013 Strategy 1: reinforce hiatus Strategy 1: reinforce hiatus with synthetic mesh with synthetic mesh Strategy 1: reinforce hiatus Strategy 1: reinforce hiatus with synthetic mesh with synthetic mesh • Carpelan-Holmstrom 2010 o PTFE Mesh erosion 6
5/18/2013 Strategy 1: reinforce hiatus Strategy 1: reinforce hiatus with synthetic mesh with synthetic mesh • Frantzides 2012 De Moor 2012: Protack and Parietex mesh migration into Cardiac tamponade can result from inappropriate fixation of gastric lumen mesh to the central tendon of the diaphragm. 10 cases of cardiac injury reported in literature after hiatal hernia repair with 6 being fatal. Central tendon of diaphragm averages 3mm in thickness ProTack helical tacks are 4mm in length. Strategy 1: reinforce hiatus Strategy 1: reinforce hiatus with synthetic mesh with synthetic mesh • Frantzides 2012 Cardiac tamponade can result from inappropriate fixation of mesh to the central tendon of the diaphragm. 10 cases of cardiac injury reported in literature after hiatal hernia repair with 6 being fatal. Central tendon of diaphragm averages 3mm in thickness ProTack helical tacks are 4mm in length. 7
5/18/2013 Strategy 2: reinforce hiatus with biological mesh How many recurrences is one erosion worth? Strategy 2: reinforce hiatus Strategy 2: reinforce hiatus with biological mesh with biological mesh Outcome Variable Biomesh Sutured 9% 24% Radiographical recurrence at 6 months Radiographical recurrence at 5 years 54% 59% Heartburn at 5 years 2.3 ± 3.1 1.4 ± 2.4 Regurgitation at 5 years 0.8 ± 1.7 1.5 ± 2.5 Dysphagia at 5 years 1.4 ± 2.5 1.6 ± 2.8 Chest Pain at 5 years 0.6 ± 1.4 1.0 ± 2.4 Abdominal pain at 5 years 2.0 ± 2.8 2.1 ± 2.7 Bloating at 5 years 2.1 ± 2.5 2.3 ± 2.6 Early satiety at 5 years 1.2 ± 2.0 2.1 ± 2.5 SF 36 QOL physical at 5 years 44 ± 11 44 ± 13 SF 36 QOL mental at 5 years 47 ± 15 49 ± 13 8
5/18/2013 Other strategies? Conclusions 1. The lifetime risk of incarceration or strangulation of PEH decreases with age and is not very high. The older and more frail your minimally symptomatic patient is, the less he/she is likely to benefit from repair. 2. Younger patients (i.e. age<65) have higher lifetime risk of symptoms and the operation is less risky. Your threshold to operate should be lower. 3. True short esophagus rarely exists. Perform a high mediastinal circumferential mobilization and you will almost always get the GEJ into the abdomen. 4. Resect the sac around the stomach, lower esophagus, and hiatus. This means also resecting the hypertrophied phenoesophageal fat pad. 5. Close the crura with permanent sutures. Pledgets don’t add benefit and can erode into esophagus. Collis lengthening procedures are rarely needed and don’t improve long term results. 6. Prosthetic mesh reinforcement probably reduces radiographical recurrences at the cost of occasional catastrophic complications. 7. Biological mesh reinforcement may reduce short term radiographical recurrence, but not long term, and has no proven symptom benefit. 9
Recommend
More recommend