Management Issues in Hypoglossal Stimulation for OSA Kingman P - PDF document
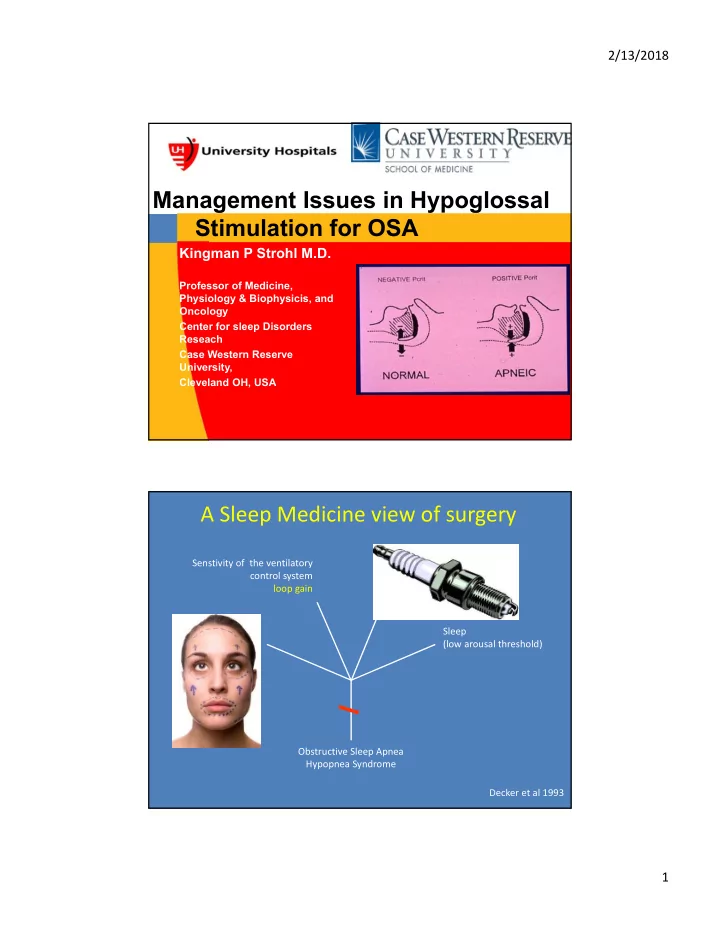
2/13/2018 Management Issues in Hypoglossal Stimulation for OSA Kingman P Strohl M.D. Professor of Medicine, Physiology & Biophysicis, and Oncology Center for sleep Disorders Reseach Case Western Reserve University, Cleveland OH, USA
2/13/2018 Management Issues in Hypoglossal Stimulation for OSA Kingman P Strohl M.D. Professor of Medicine, Physiology & Biophysicis, and Oncology Center for sleep Disorders Reseach Case Western Reserve University, Cleveland OH, USA A Sleep Medicine view of surgery Senstivity of the ventilatory Pharyngeal muscle activation control system (low gain and reflex response) loop gain Sleep Anatomy (low arousal threshold) (small, collapsible upper airway) CPAP Oral Appliance, etc. Anatomic Surgery Obstructive Sleep Apnea Hypopnea Syndrome Decker et al 1993 1
2/13/2018 Disclosures Inspire Medical – Site PI for the STAR Trial, and Inspire Post‐Approval and Registry Studies – Consultant on FDA application NIH and VA research Awards on Causes and Consequences of Sleep Apnea Galvani Bioelectronics (Consultant) Sommetrics (Consultant and Research Support) Summary Hypoglossal Stimulation is a somewhat predictable treatment option for some……. Who: • Have moderate to severe OSA • Struggle to get consistent benefit from CPAP • Have a compatible airway anatomy profile • Have a body mass index (BMI) <35, ideally <32 A team is best to determine if this invasive, non-anatomic therapy is right at this time for any given patient. • Success is dependent upon its action to reduce the closing pressure of upper airway. • In our hands, best success is when it opens the retropharyngeal space. 4 2
2/13/2018 Therapy Process Assessment Implant Follow Up Routine Follow-ups CPAP Profile Typically Therapy outpatient activation Anatomy check Therapy Sleep Study optimization Profile Follow up DISE (Drug-Induced Sleep Endoscopy) Assessment for Neural Stimulation Senstivity of the ventilatory Pharyngeal muscle activation control system (low gain and reflex response) <25% Central or Mixed Apneas Rx: Neurostimulation Sleep Anatomy ????? Insomnia and OSA Office and DISE (low arousal threshold) examination do not appear to be limiting factors. ?? Obstructive Sleep Apnea Hypopnea Consequences (AHI 20‐60) Decker et al 1993 3
2/13/2018 Insurance/Cost Considerations • Inspire therapy is FDA approved. Currently, the therapy is being reviewed by insurance companies on a patient-by- patient basis. • The first step is to see if a patient qualifies for the therapy and then the work with the patient and/or an insurance company on the Inspire implant. UAS Therapy Process Assessment Implant Follow Up Routine Follow-ups CPAP Profile Therapy activation Anatomy check Therapy Sleep Study optimization Profile Follow up ENT and DISE (Drug-Induced Sleep Endoscopy) 4
2/13/2018 Sleep Medicine • Inclusion/exclusion criteria needs • CPAP/oral appliance and documentation of attempts, reasons, and face validity of non‐use (HNS is not a choice therapy) ………….. then • Explanation of the purpose and manner of therapy including follow‐up • Restate the patient goals and assess committment • Include some documentation by the patient of why they need it. Post‐Implant Management Activation Titration Implant Long‐term Phase Phase 1 month post‐op 2 month post‐op 6 months • Thresholds and Annually* Post‐op check @ 1 week Office Visit: Office Visit: • Stimulation • Battery * In‐lab tuning • Usage Thresholds PSG 2‐6 months • Stimulation • Thresholds • Therapy Home Use: Across states • Acclimatization and positions Adjustment • HST in many cases are considered 5
2/13/2018 Final Thoughts: Patient Cost, Physician Roles, Volume Assessment Implant Follow Up Routine Follow-ups Eligibility visit Therapy Typically (1 of 5 move forward) activation Outpatient * Anatomy visit* Therapy optimization Sleep Study Profile Follow up DISE* (Drug-Induced Sleep Endoscopy) Often a stopping point Checklist for a Center: Build a Team OSA Common Knowledge Sleep Health Economics • Incidence/ prevalence/demographics • Cost of Inspire vs. alternate therapies • Disease pathophysiology • Cost vs. non-treatment • Outcomes of untreated OSA • Hospital economics • Inspire Mechanisms of Action • Physician economics Inspire vs. Alternative Therapies • Reimbursement • Efficacy • Coding • Safety profiles Assessment and Implant • Patient selection • Surgical techniques • Patient preference • Device follow-up and programming Clinical Evidence • Post operative complications • Reduction AHI/ODI (%) Practice & Patient Mgmt • Safety Profile • Patient selection • Effect on Co-morbidities/mortality • Clinical trials - best practices • QOL/ADL • Medical management after implant • Psychological issues 6
2/13/2018 Question 1 What is the operational need to establish upper airway stimulation as on option for OSA? 1. A committed surgeon 2. A sleep laboratory that can focus on higher levels of recording and analysis 3. Research level sleep medicine group 4. Both 1 and 2 5. All factors Question 1 What is the operational need to establish upper airway stimulation as on option for OSA? 1. A committed surgeon 2. A sleep laboratory that can focus on higher levels of recording and analysis 3. Research level sleep medicine group 4. Both 1 and 2 5. All factors 7
2/13/2018 Question 2 What is the hardest issue in the assessment of a patient who really wants hypoglossal stimulation? 1. Cost 2. Defining CPAP failure 3. Organizing DISE 4. Scoring the PSG for eligibility 5. Physical examination Question 2 What is the hardest issue in the assessment of a patient who really wants hypoglossal stimulation? 1. Cost 2. Defining CPAP failure 3. Organizing DISE 4. Scoring the PSG for eligibility 5. Physical examination 8
2/13/2018 Question 3 What statement about management planning is true? 1. The hospital will not be worried about the cost. 2. The cost to the patient is more than they ever expected. 3. The routines in the ENT and Sleep Medicine sections for this therapy will mesh perfectly. Question 3 What statement about management planning is true? 1. The hospital will not be worried about the cost. 2. The cost to the patient is more than they ever expected. 3. The routines in the ENT and Sleep Medicine sections for this therapy will mesh perfectly. 9
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.